JUVENILE IDIOPATHIC ARTHRITIS
Seropositive and Connective Tissue Arthropathies
Seronegative Spondyloarthropathy
CRYSTAL-INDUCED ARTHRITIDES
Gouty Arthritis
Calcium Pyrophosphate Dihydrate Crystals
Hemochromatosis
Hydroxyapatite Deposition Disease
DEGENERATIVE ARTHRITIDES
Degenerative Joint Disease
Intervertebral Disc Herniation
Spinal Stenosis
Diffuse Idiopathic Skeletal Hyperostosis
Neuropathic Arthropathy
Arthritis is the most common self-reported chronic condition among whites, the second most common among Native Americans and Hispanics, the third most common among blacks, and the fourth most common condition among Asians. For all groups, arthritis is a more prevalent chronic condition than heart disease, hearing impairments, chronic bronchitis, asthma, and diabetes. 106 Arthritis and its related conditions have a significant impact on activities of daily living, such as housekeeping, sleeping, driving, and working. Early recognition and appropriate management of arthritis are important to limit its progression and related disabilities.
IMAGING
Plain film radiography is still the most widely used and useful imaging modality for diagnosing, differentiating, and evaluating the various arthropathies. 552 Despite some limitations (e.g., insensitivity to very early joint changes), it is difficult to imagine proceeding to more advanced imaging techniques without first evaluating the patient with plain film radiography. It adequately demonstrates bone erosions, osteophytes, alterations of joint space, and misalignment. Plain film radiographs yield a relatively low dose of radiation, are inexpensive, and are readily and rapidly obtained. These factors make it perfect for baseline and serial studies that can be used to provide important information about the progression of the disease and the effectiveness of any treatment regimen. The addition of intraarticular injections of air or contrast allows limited demonstrations of the internal components of joints.
Advanced imaging modalities are being used in conjunction with plain film radiography because they may provide early detection of subtle findings such as synovitis, periarticular osteoporosis, and early erosions, when plain films are negative or inconclusive. Advanced imaging also is useful in evaluating joints with complex anatomy such as the sacroiliac (SI) articulations, which may be difficult to evaluate by the use of plain film. Computed tomography (CT) provides excellent anatomic detail and images in an axial plane. Magnetic resonance imaging (MRI) is used to evaluate the cartilaginous and ligamentous joint structures and marrow of the adjacent bone. Scintigraphy provides a useful method of gathering functional information to aid in morphologic assessments provided by other imaging modalities. Ultrasonography has the capability to define joint effusions and identify edematous connective tissues.
CLASSIFICATION
In general, arthritis can be grouped into three major categories: inflammatory (rheumatoid), crystal-induced (gout), and degenerative (osteoarthritis). Inflammatory arthritides are subdivided into rheumatoid arthritis (and related diseases) and connective tissue disorders. They also can be subdivided into rheumatoid types (seropositive) and rheumatoid variants (seronegative) based on the likelihood of the serologic presence or absence of the rheumatoid factor, as established by the latex fixation test.
Arthritis may be monoarticular or polyarticular. All types of arthritis may be monoarticular early in their pathologic course. Joint abnormalities that are caused by trauma or infections usually remain monoarticular. Arthritides are differentiated on the basis of clinical data and imaging studies (Table 9-1 and Fig. 9-1). The most useful information about them comes from plain film radiographs coupled with clinical data that relate to skeletal distribution, patient age, patient gender, joint swelling, joint stiffness, joint range of motion, symptom response to physical activity, and laboratory tests (e.g., erythrocyte sedimentation rate [ESR], antinuclear antibodies [ANAs], human leukocyte antigen [HLA] typing).
| ANA, Antinuclear antibodies; AS, ankylosing spondylitis; CPK, creatinine phosphokinase; CPPD, calcium pyrophosphate dihydrate; ESR, erythrocyte sedimentation rate; HADD, hydroxyapatite deposition disease; IBD, inflammatory bowel disease; JIA, juvenile idiopathic arthritis; LBP, low back pain; MCP, metacarpophalangeal; MTP, metatarsophalangeal; PIP, proximal interphalangeal joint; RF, rheumatoid factor; SI, sacroiliac. | ||||||||
| Arthritismode | F:M ratio | Age of onset | Target joints | Distribution | Radiographic features | Clinical features | Lab | Extraarticular manifestations |
|---|---|---|---|---|---|---|---|---|
| Rheumatoidinflammatory | 3:1 | 40–70 | MTP, MCP, PIP, knees, hips, cervical spine | Bilateral, symmetric | Capsular swelling, symmetric joint space narrowing, juxtaarticular osteoporosis, marginal erosions; joint deformity | Morning stiffness, joint swelling | +RF (IgM), ↑ESR, 10%–50% ANA, ↑C-reactive (CR) protein | Rheumatoid subcutaneous nodules, pulmonary, cardiovascular |
| JIA/inflammatory | 3.5:1 | <16 | Knees; ankles; elbows; wrists; cervical spine | Bilateral, symmetric if polyarticular | Capsular swelling, symmetric joint space narrowing, juxtaarticular osteoporosis, marginal erosions, ankylosis, growth abnormalities, periostitis | Varies with subtype: systemic-fever, adenopathy; arthralgia; rash; limp | ± RF, HLA-B27 and ANA depending on subtype; ↑ESR and C-R protein; systemic = leukocytosis | Varies with subtype; hepatosplenomegaly subcutaneous nodules; iridocyclitis |
| SLE/inflammatory | 9:1 | 30–50 | MCP; PIP of the hands primarily | Bilateral, symmetric | Nonerosive, reversible, joint deformities; osteonecrosis as possible complication | Arthralgia; butterfly rash; constitutional signs and symptoms | ANA (98%); anti–DNA antibodies; LE cells (70%–85%); RF (20%–35%); ↑ESR and C-R protein | Rash; renal disease; interstitial lung disease |
| Scleroderma/inflammatory | 8:1 | 35–65 | Distal tufts; DIP; PIP of the hands primarily | Bilateral, symmetric or asymmetric | Acroosteolysis, erosions, subcutaneous calcifications | Raynaud phenomenon; skin fibrosis; arthralgia of hands; telangiectasia | ANA in 60%; +RF (30%); ↑ESR | Skin fibrosis; renal fibrosis; GI fibrosis; interstitial lung disease; pericarditis |
| Polymyositis/dermatomyositis/inflammatory | 2:1 | 40–60 | Large muscles of the proximal appendicular skeleton; DIP, PIP, and MCPs | Bilateral, symmetric muscle involvement | Muscle edema; subcutaneous, intermuscular, and periarticular calcifications; transient osteopenia, soft-tissue swelling | Muscle weakness and atrophy; rash; arthralgia of hands, wrists, and knees | ↑CPK; muscle biopsy = inflammation and degeneration | Interstitial lung disease; pericarditis |
| AS/inflammatory | 1:10 | 15–35 | SI; spine: vertebral bodies and apophyseal articulations; hip; shoulder | Bilateral, symmetric | Erosions; periostitis; ankylosis; thin, marginal syndesmophytes | LBP and stiffness; limited chest expansion | +HLA-B27 (90%); − RF, ↑ESR, and C-R protein | Interstitial fibrosis; aortic insufficiency; iritis |
| Enteropathic/inflammatory | Varies with underlying bowel disorder | Varies | SI; spine; knee | Symmetric in axial skeleton; asymmetric in extremities | Mimics AS in the axial skeleton; nonerosive in the extremities | LBP and stiffness; IBD | +HLA-B27; − RF; ↑ESR | Underlying bowel disorder |
| Psoriatic/inflammatory | 1:1 | 30–50 | Predilection for upper extremity; DIP and PIP; SI; spine | Bilateral, symmetric, or asymmetric in SI joints; asymmetric in extremities | Sausage digit; marginal or central erosions with periostitis; early joint space widening with eventual narrowing; bulky, nonmarginal syndesmophytes; SI erosions and ankylosis | Psoriasis; nail changes (thickening, pitting, discoloration); LBP | +HLA-B27; − RF; ↑ESR | Psoriatic skin and nail changes |
| Reiter’s/inflammatory | 1:5 | 15–35 | Predilection for lower extremity; MTP; calcaneus; SI; spine | Asymmetric in foot; bilateral, symmetric, or asymmetric in SI joints | Mimics psoriatic in the spine and extremities; calcaneal enthesopathy | LBP; heel pain, urethritis; conjunctivitis | Leukocytosis; ↑ESR; HLA-B27 (75%); − RF | Pulmonary fibrosis; urethritis; conjunctivitis |
| Gout/crystal deposition | 1:20 | 40–50 | MTP of first digit; other MTPs, DIP, midfoot, ankle, DIPs of hand | Asymmetric; often monoarticular | Soft-tissue nodules (tophi) with calcification; paraarticular erosions; overhanging edge; preserved joint space; lack of osteopenia | Red, hot, swollen joint; usually monoarticular | Hyperuricemia; sodium urate crystals in synovial fluid | Tophus in bursa or helix of the ear |
| CPPD/crystal deposition | Varies with site of involvement | Varies; increases with age | Knee; wrist; hip; MCP | Often bilateral, asymmetric | Chondrocalcinosis; DJD–like changes; subchondral cysts | Varies from asymptomatic to acute goutlike pain. | Calcium pyrophosphate crystals in synovial fluid | None |
| HADDcrystal deposition | 1:1 | 40–70 | Shoulder | Asymmetric; usually monoarticular | Cloudlike periarticular calcification | Varies from asymptomatic to acute joint pain | Hydroxyapatite crystals by electron microscopy | None |
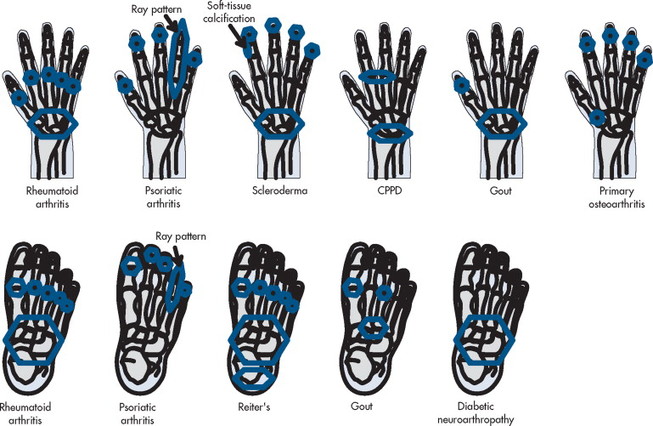 |
| FIG. 9-1 Distribution of selected joint diseases. |
Rheumatoid Arthritis
Adult Rheumatoid Arthritis
BACKGROUND
Rheumatoid arthritis (RA) is an autoimmune disorder, and the most common chronic inflammatory arthritide, affecting approximately 1% of the general population and 2% of the population over 60 years old. 243,607,610 However, studies indicate that the incidence may be on a decline in certain populations. 155,289,303,304,503 The disease primarily affects the synovial lined joints and is frequently associated with a variety of extraarticular manifestations. RA is characterized by an inflammatory, hyperplastic synovitis (pannus), resulting in cartilage and bone destruction and consequent loss of function. Although it is known that genetic and immunologic factors play a role in its pathogenesis, the underlying etiology remains uncertain. 316,537 Proposed etiologic theories revolve around a combination of genetic susceptibility, hormonal changes or imbalances (e.g., pregnancy), and environmental or biologic triggers or risk factors (e.g., smoking, obesity). 30,129,338,679 The T cell is involved in initiating and possibly propagating the chronic inflammatory disease process. Competing theories hold that the T cell initiates the disease process, but the chronic inflammation is self-perpetuated via macrophages and fibroblasts independent of the T cell.
Joint involvement typically is bilateral and symmetric, involving the peripheral and axial skeleton, with the small joints of the hands and feet, the wrists, knees, elbows, hips, and shoulders particularly affected. 89 Changes in SI articulations are relatively infrequent. Although the peak occurrence of disease onset has previously been reported as 20 to 50 years of age, recent trends indicate an increased age of onset as 40 to 70 years old, with the peak occurrence at age 58. 155,303 Women are affected more often than men, and although some studies have shown a ratio as high as 7:1, it is generally accepted that women are affected two to three times more frequently than men. 63,129,406,610 If the disease onset occurs at a more advanced age (>60 years), this ratio approaches 1:1. 488,658
IMAGING FINDINGS
Plain film radiography is an inexpensive tool and may be used by practitioners on a frequent basis in clinical practice to support clinical and laboratory findings consistent with a diagnosis of RA, aid in eliminating possible differential diagnoses, and follow the progression of RA and the effectiveness of its treatment. 568,590 Ultrasonography and MRI are superior in detecting synovitis, and many of the initial subtle joint changes are visible much earlier with MRI; however, it is not used routinely because of its high cost. Therefore this section focuses on plain film findings. 123,165,513
RA is classically symmetric and may involve any synovial joint. The general radiographic findings reflect the underlying pathologic change of chronic synovial joint inflammation with associated hyperemia, edema, and pannus formation. The first feature, which is usually the sole finding for the first few months, is fusiform periarticular soft-tissue swelling arising from capsular distention caused by excessive fluid accumulation seen clinically. Increased blood flow to the synovium leads to a second early radiographic finding of juxtaarticular osteoporosis, which later becomes more generalized because of patient inactivity. 298,380
Joint spaces eventually narrow uniformly as the cartilage is destroyed by the enzymatic nature of pannus. Osseous erosions usually become apparent within the first 2 years of the disease, 84,212,512 first occurring at the unprotected bone margins or “bare areas” (Fig. 9-2) in which the pannus has direct osseous contact, and later involving the subchondral bone. The appearance of alternating pattern of erosions and normal cortical bone has been termed a “dot dash” appearance. Multiple, nonmarginated subchondral cysts or geodes typically develop and may communicate with the synovium. 400,652
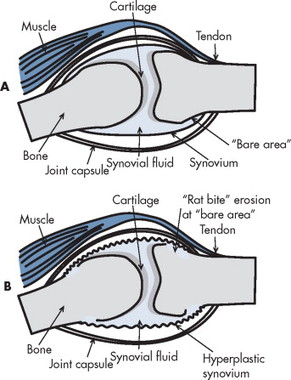 |
| FIG. 9-2 A and B, Inflamed, hyperplastic synovitis of rheumatoid arthritis, known as pannus, classically demonstrates early osseous erosions at the margins of the synovial joint that are unprotected by articular cartilage (“bare area”). |
Later stages of the disease give rise to joint deformities resulting from tendon and ligament laxity, ruptures, and contractures. During periods of prolonged remission, radiographic signs of secondary osteoarthritis (OA) may develop, fibrous ankylosis may occur, and bony ankylosis may develop on rare occasions.
Hands and feet.
The earliest clinical and radiographic changes are characteristically found in the hands and feet. 652 Although evaluation methods of RA focus on radiographs of the hands, the feet appear to show osseous erosions first and to a greater extent. 84,272,284,512,651 The initial involvement is of the head of the fifth metatarsal, with erosion and narrowing of the fifth metatarsophalangeal (MTP) joint.
The classic joint distribution of RA in the hands is bilateral and symmetric involvement of the metacarpophalangeal (MCP) and proximal interphalangeal joint (PIP) articulations. Some or all of the general radiographic features may be seen, with the earliest osseous erosions occurring at the MCP joints of the second and third digits of the dominant hand, 357 and at the radial aspect of the metacarpal heads (Fig. 9-3). Norgaard and Brewerton’s views may aid in visualization of these early joint erosions, although it is difficult to duplicate the exact positioning on serial radiography. 652 In Norgaard’s view, the hands are 45 degrees supine, with the fingers straight, 461 and in Brewerton’s view (ballcatcher’s view), the MCP joints are flexed at 65 degrees. 79
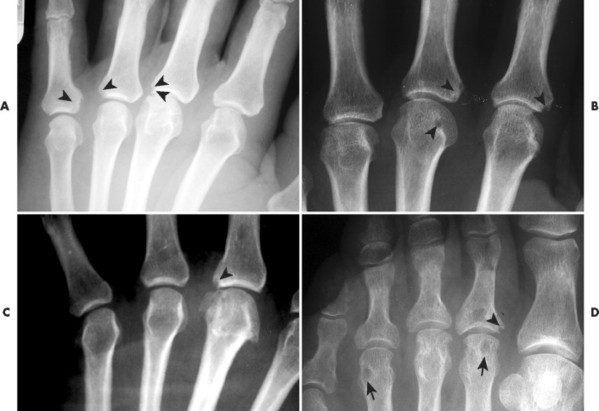 |
| FIG. 9-3 Small marginal “rat bite” erosions (arrowheads) occur in the region of the joint that is unprotected by overlying articular cartilage, known as the bare area. A to C, Small marginal erosions of the metacarpophalangeal and, D, metatarsophalangeal joints are hallmark features of rheumatoid arthritis, noted here in three patients. Subchondral cysts also are noted in case D (arrow). |
Characteristic joint deformities include the swan neck deformity, boutonnière deformity, ulnar deviation of the fingers (doigts en coup de vent), and the hitchhiker’s or Z-shaped deformity of thumb. The swan neck deformity results from hyperextension of the PIP and hyperflexion of the distal interphalangeal joint (DIP) (FIG. 9-4FIG. 9-5FIG. 9-6 and FIG. 9-7), whereas the boutonnière deformity represents the opposite configuration of hyperflexion of the PIP and hyperextension of the DIP. The hitchhiker’s thumb is secondary to MCP flexion and interphalangeal (IP) extension (see Fig. 9-5). Ulnar deviation at the MCPs is called ulnar drift; when combined with radial deviation in the radiocarpal articulations it results in a “zigzag” deformity (see Fig. 9-5). Loosening or disruption of the distal attachment of the extensor tendon to the terminal phalanx leads to a “mallet” finger.
 |
| FIG. 9-4 Rheumatoid arthritis. The ulnar deviation of the fingers, especially prominent at the fifth digit of the right hand, and Z-deformity of the left thumb are the most obvious features of rheumatoid arthritis in this patient. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-5 Ulnar deviations of the fingers and advanced arthropathy of the metacarpocarpal joints and wrist are consistent with rheumatoid arthritis. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
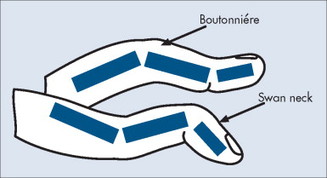 |
| FIG. 9-6 Rheumatoid arthritis characteristically manifests with interphalangeal joint misalignments. The misalignments express either swan neck deformity (flexion of distal and extension of the proximal interphalangeal joints) or boutonnière deformity (extension of the distal and flexion of the proximal interphalangeal joints). |
 |
| FIG. 9-7 Rheumatoid arthritis with ulnar deviation of the fingers, metacarpal joint involvement, and advanced destruction of the wrist. (Courtesy Gary Longmuir, Phoenix, AZ.) |
Changes in the feet tend to parallel those of the hands, with the MTP articulations commonly being affected first and other deformities, including lateral or fibular deviation at the MTPs of the first through fourth digits, flexion of the DIPs (hammer or claw toes), and extension of the MTPs eventually developing (FIG. 9-8FIG. 9-9FIG. 9-10 and FIG. 9-11). Pathologic changes in the deep transverse tendons may lead to spreading of the metatarsals or forefoot. Pathologic changes in supporting ligaments also may lead to hallux valgus. Retrocalcaneal bursitis, plantar fasciitis, Achilles tendonitis, or Achilles tendon rupture may occur in the heel.
 |
| FIG. 9-8 Rheumatoid arthritis presenting with subchondral cysts (arrowheads) and reduction of the first metatarsophalangeal joint bilaterally (arrows). |
 |
| FIG. 9-9 Rheumatoid arthritis of the foot with advanced changes of the fibular misalignment of the toes, osteopenia (more pronounced in the periarticular regions), reduced joint spaces, and generalized atrophy of the bones. |
 |
| FIG. 9-10 Fifty-year-old male rheumatoid patient demonstrating marked symmetric and bilateral fibular deviation of the toes. (Fibular deviation with posterior subluxation of the metatarsophalangeal joints is termed Lanois deformity.) |
 |
| FIG. 9-11 Rheumatoid arthritis manifests with bone reapportion. In this 64-year-old woman, rheumatoid arthritis has caused a tapered appearance of the distal metatarsals. |
Wrist.
Pancompartmental involvement typically is in the wrist, with the earliest erosions usually involving the radial and ulnar styloid processes; distal radioulnar and radiocarpal joints; and waist of the scaphoid, triquetrum, and pisiform (FIG. 9-12FIG. 9-13FIG. 9-14FIG. 9-15 and FIG. 9-16). 357 Ligamentous instability results in patterns that parallel posttraumatic lesions, such as scapholunate dissociation, distal radioulnar dissociation, and dorsiflexion or volar flexion instability.
 |
| FIG. 9-12 Rheumatoid arthritis presenting with wrist and metacarpal destruction with slight ulnar deviation of the fingers. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-13 Rheumatoid arthritis presenting with bilateral, symmetric destructive changes of the intercarpal joints of the wrist. |
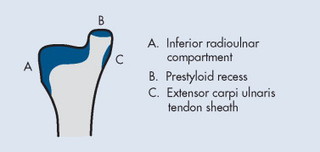 |
| FIG. 9-14 Erosions of the ulnar styloid may manifest in each of the areas that have adjacent synovial tissue: radiocarpal joint, prestyloid recess, and extensor carpi ulnaris. |
 |
| FIG. 9-15 A and B, Erosions of the styloid process in two patients (arrows). |
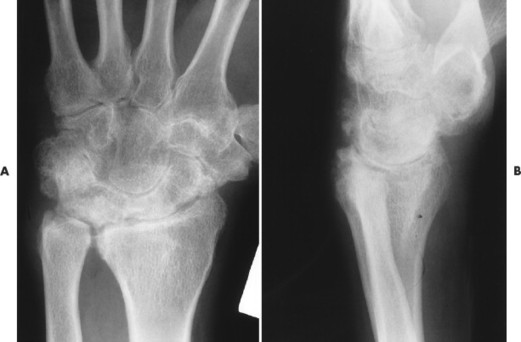 |
| FIG. 9-16 A and B, Rheumatoid arthritis in the wrist. Inflammation is most notable in the proximal row of carpals, radiocarpal compartment, and distal ulna. Mild osseous proliferation is noted, suggesting clinical quiescence. |
Elbows.
Joint effusion is recognized by a positive fat pad sign. Osseous erosions may be noted at each of the articulating surfaces.
Shoulders.
The glenohumeral and acromioclavicular (AC) joints may be affected. Resorption of the distal clavicle, in addition to erosions at the coracoclavicular ligament insertion on the undersurface of the clavicle, is not uncommon. Erosion may be observed on the medial aspect of the humeral neck as it abuts the glenoid process from elevation of the humerus, which is caused by a rotator cuff tear secondary to a chronically inflamed supraspinatus tendon. The acromiohumeral distance narrows with progressive elevation of the humeral head, and sclerosis and cyst formation are noted on the adjacent portions of the humeral head and acromion process.
Hips.
Abnormalities of the hips generally are bilateral and symmetric. Axial migration of the femoral head and bilateral acetabular protrusion are common findings that accompany the other general features of concentric joint space narrowing, erosions, and subchondral cysts associated with RA (Figs. 9-17 and 9-18). 134 There is an absence of sclerosis and osteophyte formation unless secondary OA has developed.
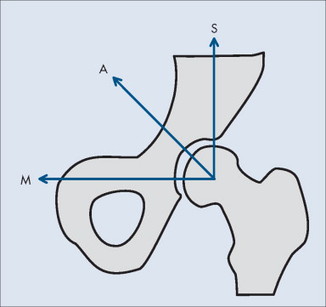 |
| FIG. 9-17 The iliofemoral joint is divided into an, M, medial; A, axial; and, S, superior component. The inflammatory arthritides, inclusive of rheumatoid arthritis, tend to decreased all of these spaces symmetrically, whereas degenerative joint disease reduces the superior, weight-bearing aspect of the joint and increases the medial joint space. |
 |
| FIG. 9-18 Early rheumatoid arthritis of the hip shown by concentric loss of joint space, small erosions of the femoral head and acetabulum, and osteopenia. Note the lack of osteophytosis and eburnation. |
Knees.
Tricompartmental involvement that includes the general features of joint space narrowing and osseous erosions is typical (Figs. 9-19 and 9-20). A genu valgus deformity is more likely to develop than a varus joint deformity (Fig. 9-21). Soft-tissue swelling may be present in the form of suprapatellar effusion or a large popliteal (or Baker’s) cyst. Subchondral sclerosis and osteophytes may be noted with the development of secondary osteoarthritis.
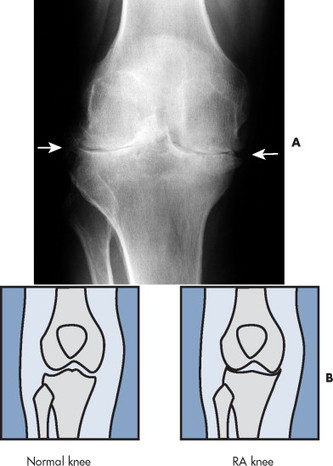 |
| FIG. 9-19 A and B, Rheumatoid arthritis noted by symmetric reduction of both the medial and lateral femorotibial joint spaces (arrows). |
 |
| FIG. 9-20 Rheumatoid arthritis. In this case, rheumatoid manifests with osteoporosis and symmetric loss of the femorotibial joint spaces. The symmetric loss of joint space noted in these cases is contrary to what is expected with degenerative joint disease. Degeneration presents with asymmetric loss of joint space (more advanced in the medial femorotibial compartment) and osteophytes. |
 |
| FIG. 9-21 Genu valgus deformity is noted in this 57-year-old woman. The film is annotated in preparation for surgical placement of a prosthesis. |
Cervical spine.
RA involvement is rare in other regions of the axial skeleton but affects the cervical spine in more than half the patients within the first 10 years of disease onset, 531,652 with a preference for the apophyseal and atlantoaxial joints. The more chronic the disease, the greater is the likelihood of cervical involvement. 466 Radiographs of the cervical spine are a prudent consideration in all patients with RA regardless of symptoms, because many patients are asymptomatic despite cervical involvement. 117 These should include lateral views with the patient in flexion and extension.
Atlantoaxial subluxation or instability is the most common radiographic abnormality encountered in the cervical spine, with the prevalence varying from 19% to 70% depending on the patient selection and radiographic examination (Fig. 9-22). 311 Movement may occur in several directions (listed in order of decreasing frequency): anterior (most frequent, 9.5% to 36%), lateral, vertical, or posterior. 55,107 Movement is usually the result of odontoid erosions or transverse ligament laxity, although the alar and apical ligaments also may be involved.
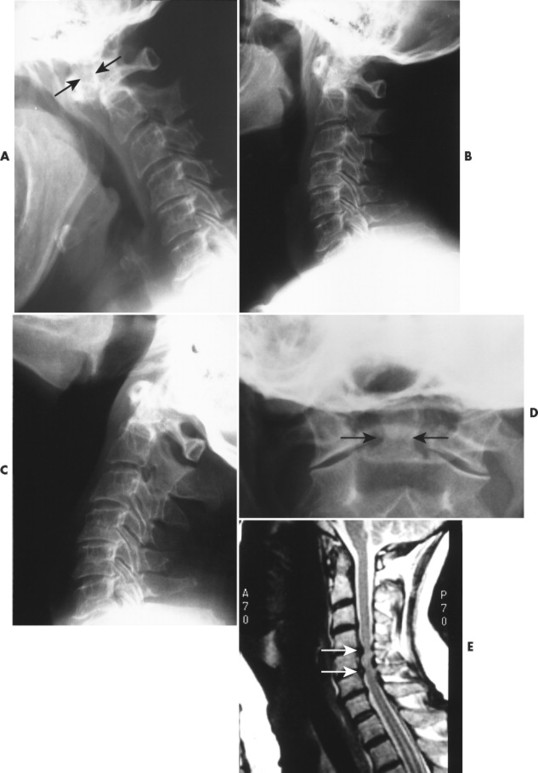 |
| FIG. 9-22 Anterior atlantoaxial subluxation. A, Lateral radiographs of the cervical spine in flexion; B, neutral; and, C, extension positions revealing an atlantoaxial subluxation that is most notable on the flexion radiograph. Note the wide gap between the posterior surface of the anterior arch of the atlas and anterior aspect of the odontoid (arrows). D, The anteroposterior open mouth radiograph of the same patient reveals rheumatoid erosions at the base of the odontoid process (arrows). The lateral atlantoaxial joints appear unaffected. E, Sagittal T2-weighted magnetic resonance image (MRI) of same patient revealing marrow changes of the odontoid process, synovial inflammation, and multiple subaxial subluxations in the middle and lower regions of the cervical spine with disc protrusions (arrows) and resulting cord compression. Instability resulting from rheumatoid pannus is a concern for neck movement, including chiropractic adjustments, neck movement with spinal surgery, or placement of an endotracheal tube related to emergency medicine. If instability is suspected, flexion-extension studies, computed tomography, or MRI are warranted for further investigation. |
The degree of anterior subluxation shown on conventional radiography correlates poorly with neurologic signs and the presence of cord compression, which is in part a result of the unknown thickness of the synovial pannus not visible on plain films. 55,542 The standard method for determining anterior atlantoaxial subluxation has been an anterior atlantodental interval* (ADI) of greater than 3 mm, but it has been shown that a posterior atlantodental interval† (PADI) of 14 mm or less may be a more reliable predictor for neural compression and necessitate an MRI for evaluation of true cord space (Fig. 9-23). 55
*The ADI is the distance between the posteroinferior aspect of the anterior arch of the atlas and the most anterior point of the odontoid process. Measurements of greater than 3 cm are considered abnormal. The measurement should be obtained from a lateral flexion radiograph.
†The PADI is measured from the posterior wall of the dens to the anterior aspect of the C1 lamina.
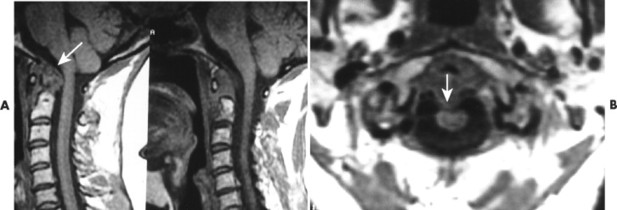 |
| FIG. 9-23 A, Sagittal T1-weighted gradient echo and, B, axial gradient echo magnetic resonance images revealing prominent synovial inflammation (pannus) in the posterior median atlantoaxial joint (arrow) with apparent destruction of the dens and mild compression of the spinal cord (arrow). |
Vertical atlantoaxial subluxation also is known as cranial settling, atlantoaxial impaction, and pseudobasilar invagination. Superior migration of the odontoid occurs with erosion of the occiput-C1 and C1-2 articulations, resulting in approximation of the dens and brainstem, which can lead to direct compression or cause neurologic damage by excessive kyphosis. 92,542 McGregor’s line may be used to assess superior migration, or the Sakaguchi-Kauppi method may be used, which was developed for screening purposes and evaluating the position of C1 in relation to C2. 312
Subaxial subluxations may occur in 10% to 20% of patients and often are at multiple levels. C3-4 and C4-5 are the most common areas of involvement, producing a “stepladder” or “doorstep” deformity and associated kyphosis on the lateral radiograph. 478 Although these are less common than upper cervical spine subluxations, they are potentially more important neurologically because of the smaller spinal canal dimensions. 55,107 A canal measurement may be taken from the lateral radiograph in a similar way that the PADI is taken. If the subaxial canal diameter measures less than 14 mm, MRI is advised. 55
Disc height narrowing, mild subchondral sclerosis, and erosions of the vertebral endplates, facet joints, and spinous processes are other less severe signs of rheumatoid involvement. These signs often are subtle and difficult to diagnose on plain film radiographs.
Lungs.
Lung involvement is common, although not always clinically significant. Pleural involvement (e.g., pleurisy, pleural effusion) is the most common lung manifestation and usually is asymptomatic. 13 Other pulmonary manifestations include pulmonary fibrosis or honeycombing, constrictive bronchiolitis, bronchiectasis, pulmonary nodules, and subpleural micronodules (Fig. 9-24). High-resolution computed tomography (HRCT) is useful for this avenue of investigation. These findings have been observed on CT in patients with symptoms, and those asymptomatic patients with no abnormalities noted on chest plain film. 546 Caplan syndrome describes inflammation and scarring of pulmonary tissue in people with RA who have exposure to coal dust.
 |
| FIG. 9-24 Radiodense linear shadows most prominent in the lower lung fields as a feature of pulmonary fibrosis in a rheumatoid patient. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
The criteria for the diagnosis of RA, which were designed originally to aid in research consistency, have been revised and are now easier for the clinician to use. 22 The diagnosis can be made if the patient meets at least four of the following criteria established by the American College of Rheumatology. The first four must be present for at least 6 weeks.
1. Stiffness in the morning that lasts at least 1 hour
2. Swelling of at least three joints
3. Swelling of the wrist, MCP, or PIP joints
4. Symmetric swelling
5. Rheumatoid nodules
6. Positive rheumatoid factor test
7. Radiographic changes consistent with RA
The joint stiffness is sometimes termed jelling phenomenon and occurs in the morning or after periods of inactivity. Jelling also is described in fibromyalgia.
Although the main sites affected by RA are the joints, extraarticular manifestations are common. Rheumatoid nodules are the classic extraarticular lesions. These subcutaneous lesions are found in approximately 25% to 40% of patients and are typically located on the extensor surfaces at sites subject to trauma. 406,610 These nodules also can be present in visceral organs. Pulmonary and cardiovascular systems often are affected in patients with RA. Two syndromes associated with RA are Felty (a combination of RA, splenomegaly, and neutropenia) and Sjögren (marked by RA and dry eyes and mouth). A laboratory clue to Felty syndrome is decreased white blood cells, which occurs with splenomegaly.
Patients with RA tend to have reduced life expectancies and decreases in their ability to perform activities of daily living and work. 454,510 The disease course is variable, ranging from mild with periods of remission to severe and quickly progressive. The highest rate of joint damage and progression occurs early in the disease; therefore treatment should begin immediately after the diagnosis is made so that irreversible joint damage is prevented. 652 Known risk factors may increase the possibility of developing the severe stages of the disease and early mortality, so these patients may need a more aggressive treatment. 509,510,658,661
Laboratory tests.
Laboratory tests aid in establishing the diagnosis and assessing disease activity. The test for the presence of rheumatoid factor is positive in approximately 70% to 80% of patients with RA (95% if presenting with subcutaneous nodules) but also is positive in approximately 5% of individuals who do not have RA, and in patients with other nonrheumatoid diseases. 368,384 Therefore a positive or negative rheumatoid factor test must be correlated closely with other clinical features. A complete blood count, ESR, C-reactive protein, and ANA assay also may be performed to initially evaluate and as follow-up for rheumatoid patients. 684
Treatment and management.
RA has become one of the most costly musculoskeletal disorders because of loss of work and limitations in daily activities caused by pain and functional disability, 6,10,194,693 and because of the associated treatment cost. More aggressive treatment is being used at the initial onset of RA to combat unfavorable long-term outcomes. 650,656
Treatment is multifaceted and geared toward reducing pain and limiting or slowing the progression of deformities and associated disability. Conservative therapy should include patient education (inclusive of pain coping techniques) and emotional support; 318,367,645 rest; application of heat or cold; dietary changes or supplementation; and resistance training, exercise, and joint mobilization to improve joint range of motion, strengthen muscles, and minimize joint deformity. *
Pharmacologic treatment includes nonsteroidal antiinflammatory drugs (NSAIDs), corticosteroids, and more aggressive second-line of therapy or disease-modifying antirheumatic drugs (DMARDs), such as antimalarial drugs, intramuscular gold, and penicillamine. Infliximab and etanercept are biologic response modifiers that block specific immune factors leading to RA; these treatments have now been approved as second-line therapy. Third-line drugs or immunosuppressants inhibit the immune system and may have serious side effects. 65,610
At the disease onset, radiographs of the hands, wrists, and feet should be obtained as a baseline and then repeated at 6-month intervals for a minimum of 2 years to aid in identifying those patients at risk for serious joint damage and deformity. 85,494 MRI of the spine should be performed on patients with radiographic abnormalities combined with neurologic deficits, and should be considered in patients with superior migration of the dens, a PADI of less than 14 mm, and a subaxial canal diameter of less than 14 mm regardless of symptoms. MRI with contrast (gadolinium) should be used to differentiate synovial fluid from pannus. Surgical intervention may be indicated to replace joints (Fig. 9-25), correct severe deformity, 229 or treat neurologic compromise. 207
 |
| FIG. 9-25 A, Anteroposterior and, B, lateral radiographs showing changes typically associated with rheumatoid arthritis of the knee. The most striking finding is tricompartmental loss of joint space and joint effusion. Small marginal osteophytes indicate secondary osteoarthritis (arrows). C and D, Because of ongoing pain and disability related to the advanced rheumatoid arthritis, the patient underwent total resurfacing knee arthroplasty. |
• Females are more likely to develop the disease than men (two or three times more likely, less in older populations), with the peak incidence occurring between 40 and 70 years of age.
• The primary sites affected are the synovial tissues of the hands, feet, wrists, hips, knees, elbows, and shoulders. Affected metacarpophalangeal and proximal interphalangeal joints of the hand and atlantoaxial subluxation of the cervical spine are most characteristic. The sacroiliac articulations are rarely affected.
• This arthritide is marked by a bilateral symmetric distribution, periarticular soft-tissue swelling, initial juxtaarticular osteoporosis progressing to generalized uniform loss of joint space, marginal erosions (bare areas) progressing to subchondral erosions, subchondral cysts, and joint deformities.
• Hip involvement may lead to bilateral acetabular protrusion.
• Subluxations and joint deformities, including swan neck, boutonnière, and hitchhiker’s thumb, are characteristic.
• Treatment is directed toward limiting pain and disability and may include surgery for joint replacement or to address neurologic complications.
Juvenile Idiopathic Arthritis
BACKGROUND
In the United States juvenile rheumatoid arthritis (JRA) and juvenile chronic arthritis (JCA) are terms often used interchangeably to encompass the three major subsets of JRA, whereas in Europe the designation of JCA includes not only JRA (and its subsets), but also the addition of the juvenile spondylarthropathies (ankylosing spondylitis [AS], enteropathic arthritis, and psoriatic arthritis). 104,105,689 To unify these previous classifications and decrease confusion, which in turn would facilitate research and aid in identification of homogeneous groups of children, a new classification known as juvenile idiopathic arthritis (JIA) has been developed. 506,639 The definition of JIA basically is consistent with the definitions of JRA and JCA, although additional subsets have been added to the new classification system.
Classification according to the International League against Rheumatism: JIA
1. Systemic arthritis
2. Oligoarthritis
a. Persistent
b. Extended
3. Polyarthritis (rheumatoid factor negative)
4. Polyarthritis (rheumatoid factor positive)
5. Enthesitis-related arthritis
6. Psoriatic arthritis
7. Other or unclassified arthritis
Classification according to the American College of Rheumatology: JRA
1. Systemic
2. Pauciarticular or monoarticular
3. Polyarticular
a. Seronegative
b. Seropositive
Classification according to the European League against Rheumatism: JCA
1. Juvenile-onset adult type (seropositive)
2. Seronegative chronic arthritis (Still’s disease)
a. Classic systemic disease
b. Polyarticular
c. Pauciarticular or monoarticular
3. Juvenile spondyloarthropathy (AS, psoriatic arthritis, enteropathic arthritis)
The terms JIA, JRA, and JCA all indicate an inflammatory disease of unknown cause, occurring in childhood (<16 years of age), characterized primarily by arthritis (joint inflammation and stiffness) persisting for a minimum of 6 weeks (JCA symptoms must last at least 3 months). The term juvenile idiopathic arthritis (JIA) is used in this book.
JIA is the most common type of arthritis affecting children. 677 It is an autoimmune disorder with a prevalence that appears to range between 12 and 148 cases per 100,000, 503,601,646 and an incidence rate of 17 per 100,000, that appears to on the decline. 304,503 It targets predominantly the synovial joints, in which synovial proliferation leads to joint and soft-tissue destruction. It is suspected that genetics may predispose a patient to the disease, and an infectious or environmental factor may trigger its onset.
The first four subsets of the new classification system of JIA encompass the vast majority of cases and are essentially the same subsets listed by the American College of Rheumatology (ACR) as representative of JRA. They are the main focus of this section. They are divided according to the presence or absence of rheumatoid factor, systemic symptoms within the first 6 months of onset, and number of joints involved within the first 6 months of onset. Subsets 1, 2, and 3 comprise approximately 70% of all JIA patients. Subset 4 represents approximately 5% to 10% of all JIA cases.
1. Systemic arthritis (essentially classic systemic onset disease) is the most serious. It occurs in children under 5 years of age; affects males and females equally; and presents with spiking fevers, a characteristic salmon-colored rash on the trunk and thighs, hepatosplenomegaly, serositis, adenopathy, leukocytosis, and mild polyarthritis, usually of the wrist, knees, and ankles.
2. Oligoarthritis (essentially pauciarticular or monoarticular) is the most common variety, and is found in young children under 5 years of age and affects no more than four joints during the first 6 months, generally affecting large joints (e.g., knees, ankles, elbows, wrists). This form frequently is accompanied by asymptomatic chronic iridocyclitis, uveitis, cataracts, and (in a minority) blindness. There is a large association with antinuclear antibodies. Two additional subcategories are recognized: persistent oligoarthritis and extended oligoarthritis. Persistent oligoarthritis affects no more than four joints throughout the course of the disease. Extended oligoarthritis affects a cumulative total of five or more joints after the first 6 months of onset.
3. Polyarthritis (rheumatoid factor negative, essentially polyarticular seronegative) involves more than five joints during the first 6 months of the disease, is more prevalent among females between 12 and 16 years of age, and has an early onset between the ages of 1 and 3 years. Symmetric small joint involvement of the hands and feet is common, which is similar to the distribution of adult RA.
4. Polyarthritis (rheumatoid factor positive, essentially polyarticular seropositive) develops in teenage girls and is similar clinically and radiographically to adult RA. 15,572 Juvenile patients may present with subcutaneous nodules, although this symptom occurs less frequently in juveniles than adults. More than five joints are affected, most commonly the hands, wrists, feet, knees, hips, and cervical spine.
5. Enthesitis-related arthritis usually occurs in males over 8 years old and indicates the presence of arthritis and enthesitis, or arthritis or enthesitis with at least two of the following: SI tenderness or inflammatory spinal pain, presence of HLA-B27, or family history of confirmed HLA-B27 in at least one first- or second-degree relative.
7. Other or unclassified arthritis indicates childhood arthritis of unknown cause persisting for at least 6 weeks that does not fulfill criteria for subsets 1 to 6, or fulfills criteria for more than one of the other subsets.
IMAGING FINDINGS
Although other imaging modalities may be more sensitive for early detection of joint pathology, plain film radiography continues to be the primary method of imaging for the diagnosis and follow-up evaluation of JIA. The radiographic presentation in the majority of JIA cases is similar in appearance to adult RA with few exceptions (Table 9-2). Although features within each subset of JIA can differ, there are features that may be common to all. These include early manifestations such as fusiform periarticular soft-tissue swelling and juxtaarticular osteopenia (which may include growth recovery lines) that may become diffuse. Intermediate or later-stage manifestations may include joint space narrowing, osseous erosions, growth disturbances, bony ankylosis, joint contractures, subluxation, or dislocation. Early plain film radiographs may be negative, and a technetium bone scan, CT, or MRI may be more helpful.
| Radiographic finding | Juvenile rheumatoid | Adult rheumatoid |
|---|---|---|
| Joint space narrowing | Common in late stages of disease | Common in early stages of disease |
| Marginal bony erosion | Common in late stages of disease | Common in early stages of disease |
| Intraarticular fusion | Common | Uncommon |
| Growth abnormalities | Common | Absent |
| Periostitis | Common | Absent |
Distinct features of JIA include periostitis and growth abnormalities, which are the result of the disease process combined with skeletal immaturity. Periostitis commonly involves the diaphysis of the metacarpals, metatarsals, and proximal phalanges and may be an early and prominent finding that is likely explained by the exposure of loosely attached periosteum to an inflammatory and hyperemic process. Growth abnormalities result from hyperemia to the epiphysis and growth plates, causing an overgrown “ballooned” or “squared” epiphysis. Hyperemia also may lead to premature growth plate fusion, resulting in shortening of limbs or limb length discrepancies.
Overall joint involvement mimics that of adult RA in the majority of cases, although JIA has more of a predilection for large joints. Individual joint manifestations are noted in the following explanations.
Knees.
The knee is the most commonly affected joint in JIA. Effusion; joint space narrowing; osteopenia and enlargement, or “ballooning” of the metaphysis and epiphysis of the distal femur and proximal tibia; widening or expansion of the intercondylar notch; and patellar squaring are the most distinctive findings associated with JIA in the knee (Fig. 9-26). Growth arrest lines may result from temporary reduction in growth velocity, and frequently are seen around the knee. A discrepancy in leg lengths may occur with knee inflammation. If the inflammation is controlled and occurs before the age of 9, the leg lengths equalize and no residual discrepancy remains. If involvement exists after the age of 9, early epiphyseal closure may occur and result in a permanently shorter leg on the involved side. 600
 |
| FIG. 9-26 A, Anteroposterior and, B, lateral knee radiograph in a patient with juvenile idiopathic arthritis. The femoral condyles are enlarged and the intercondylar notch is widened, both of which are common features of the disease in this joint. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Ankles and feet.
Swelling may be noted on the dorsum of the foot because of involvement of the subtalar and tibiotarsal joints (Fig. 9-27). Tibiotalar slant, valgus, and varus deformities may result. 545
 |
| FIG. 9-27 Juvenile idiopathic arthritis. A, Symmetric findings include generalized osteopenia, diaphyseal overtubulation, widespread joint space narrowing, evolving ankylosis (arrows), and diffuse muscle wasting. B, Another patient exhibits widespread ankylosis (arrows) in the hindfoot and midfoot with a cavus deformity secondary to the disease and stabilizing surgery. Osteopenia and muscle atrophy also are evident. Differential diagnosis should include consideration of other causes of disuse beginning in childhood, and certain congenital foot deformities. (From Sartoris DJ: Musculoskeletal imaging: the requisites, St Louis, 1996, Mosby.) |
Hands and wrist.
Early findings include soft-tissue swelling and juxtaarticular osteoporosis of the carpals, MCPs, and PIPs; preservation of joint space; lack of erosions; and periosteal new bone formation, resulting in a widened midportion of the phalanges (Figs. 9-28 and 9-29). Accelerated skeletal maturation; osseous erosions in the carpus, distal radius, and ulna; joint space narrowing; carpal and carpometacarpal ankylosis; and boutonnière and swan neck deformities (see description in previous section of adult RA) may present in later stages. Growth defects may be seen in the ulna and the fourth and fifth metacarpal bones (positive metacarpal sign).
 |
| FIG. 9-28 Juvenile idiopathic arthritis demonstrating enlarged radial and ulnar epiphyses, carpals, osteoporosis, thin cortices, and soft-tissue swelling in this 14-year-old boy. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-29 A and B, Bilateral symmetric expression of osteoporosis, soft-tissue swelling, carpal and hand joint erosions, and enlarged epiphysis of the distal radius and ulna consistent with juvenile idiopathic arthritis. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Hips.
JIA may be indicated by lack of growth of the iliac bone, femoral head flattening and enlargement, early growth plate closure, coxa valga deformity, and acetabular protrusion. Osteonecrosis also may develop as a complication of the disease but more often is related to treatment (corticosteroids).
Cervical spine.
Atlantoaxial subluxation and odontoid erosions occur, but not as frequently as in patients with adult-onset RA. Cervical spine flexion and extension radiographs should be a consideration. Apophyseal joint ankylosis may occur after facet erosions in the upper and middle cervical spine (Fig. 9-30), and appears to be the most common abnormality of the cervical spine occurring more frequently at multiple levels than at a single level. 172,343,344,401 The ankylosis is thought to cause vertebral body and disc hypoplasia. The so-called juvenile cervical vertebra is more commonly found in patients with early-onset disease172,344 than in those with late-onset disease.
 |
| FIG. 9-30 Juvenile idiopathic arthritis with vertebral hypoplasia and fusion of the posterior joints (arrow) in the cervical spine. Although inflammation may affect the posterior facets in both adult and juvenile forms of rheumatoid arthritis, resultant apophyseal fusion is common in children and unlikely in adults. Vertebral body and disc hypoplasia also are prominent features in juvenile rheumatoid arthritis. (Courtesy Jack C. Avalos, Davenport, IA.) |
Mandible.
Micrognathia may be observed clinically, but more often radiographically in children with JIA.
Radiographic changes in enthesitis-related arthritis.
The SI joint is involved, but usually not at the onset of the disease. There is widening of the joint space with erosions on the inferior aspects of both articulating surfaces. CT may best assess these changes given the presence of a normally wide SI joint space in children. In the feet, the MTP and IP joints of the first digit frequently are affected. Plantar enthesitis also may be noted. Hip involvement may be noted with enlargement of the femoral epiphysis, iliofemoral joint space narrowing, and femoral neck osteophytosis (similar to that seen in adult AS).
CLINICAL COMMENTS
Presentation.
Because there is no single test to diagnose JIA, it is considered a diagnosis of exclusion, 76 as other conditions such as infection; trauma; congenital, hematologic, and collagen vascular disorders; and malignancies are eliminated. The clinical presentation may be a child with persistent joint swelling, pain, and stiffness; a painless limp; or a presentation with systemic symptoms (e.g., fever, rash, lymphadenopathy). Symptoms should be present for 6 weeks before the diagnosis of JIA is made. Children with JIA may be undersized and have generalized or localized growth abnormalities.
Laboratory abnormalities.
Laboratory abnormalities reflect the inflammatory process, and studies are used only to support the clinical suspicion of or monitor the progression of JIA. Depending on the subtype, anemia, leukocytosis, proteinuria, antinuclear antibodies, rheumatoid factor, HLA-B27, and an elevated ESR may be present.
Therapy and management.
The approach to therapy is similar to that for adult-onset RA and varies depending on the course of the disease. It should focus on pain relief, preservation of joint function, maintenance of normal growth and muscle strength, and psychosocial development. Adequate nutrition is essential. Active exercise, maintaining joint range of motion, and physical therapy may aid in preserving or restoring joint space and leading to clinical improvements. 491 Aspirin and NSAIDs usually are given to help with inflammation, whereas the use of systemic corticosteroids initially is avoided because growth retardation is a major complication, but may be used in low doses, or for children with life-threatening complications, and topically for eye involvement. The more “hard-core” second- or third-line therapies are considered with unresponsive patients or those with life-threatening systemic disease. Ophthalmologic examinations should be given at least semiannually to detect asymptomatic iridocyclitis. Eye examinations are given more often in ANA-positive patients.
• Juvenile rheumatoid arthritis (JRA) and juvenile chronic arthritis (JCA) are often used synonymously in the United States, whereas the additional subset of juvenile spondylarthropathies is included with JRA to form JCA in Europe. For unification, a new classification, juvenile idiopathic arthritis (JIA), has been developed to encompass and expand on these two systems.
• JIA is the most common childhood arthritis, affecting children under 16 years of age.
• The subsets of JIA are based on the number of joints involved, systemic involvement, and the presence or absence of rheumatoid arthritis factor.
• Although joint involvement mimics that of adult rheumatoid arthritis, JIA has a greater predilection for large joint involvement and intraarticular fusion. Periostitis and growth abnormalities are noted in juvenile-onset disease, and not adult-onset disease.
• Hands, wrists, knees, hips, and the cervical spine are commonly affected.
• Therapy is similar to that used for adult rheumatoid arthritis, although more caution is used with regard to use of corticosteroids and more “hardcore” lines of defense because of the potentially devastating side effects.
Seropositive and Connective Tissue Arthropathies
Systemic Lupus Erythematosus
BACKGROUND
Systemic lupus erythematosus (SLE) is an inflammatory connective tissue disorder that involves multiple organ systems and is characterized by excessive immunoreactivity (an autoimmune disorder) in which the antibodies are directed against cell nuclei. 457,540 Although the factor that activates this immune response is unclear, a major element of the underlying pathogenesis is widespread vasculitis, which may be secondary to local deposition of immune complexes. 39 Virtually any tissue can be damaged, but the joints, skin, kidneys, and serosal membranes are most frequently affected. 70,346 There is a genetic predisposition or a familial link associated with SLE. In addition, factors known to trigger flare-ups include exposure to sunlight and certain medications.
SLE usually follows an irregular chronic course of exacerbations and remissions. The mean length of time between the initial onset of symptoms and diagnosis is 5 years. The prevalence of SLE is approximately 24 cases per 100,000, 288 with some evidence of an increasing incidence rate. 648 Recent population-based studies reveal that SLE may now occur at a later age of onset, 30 to 50 years, 268,295,418,648 than the previously reported range of 20 to 40 years. Women are affected up to nine times more often than men, 288 and the most significant ratio variance occurs during the childbearing years. The ratio appears to lessen if disease onset occurs in childhood or at more than 50 years of age. SLE typically occurs 5 to 10 years earlier in women than men, although this difference may be limited to white patients. 418 In the United States, blacks are at a higher risk than whites for the development of SLE; in addition, the age at diagnosis is approximately 7 years younger among blacks. 418
IMAGING FINDINGS
Although up to 90% of patients complain of articular problems, prominent and severe radiographic changes are uncommon. 342 The most frequently affected joints are the hands, feet, wrists, and knees. Soft-tissue swelling and minimal periarticular osteoporosis are the earliest radiographic manifestations and usually present bilaterally and symmetrically. Joint deformities may ensue in later stages. Subcutaneous calcifications (calcinosis cutis) are not common in SLE, but when they occur they have a predilection for the lower extremities and can be diffuse or nodular. 675 These calcific densities are prone to ulceration and infection.
Hands.
In the hands, SLE has a joint distribution similar to RA, affecting the MCPs and PIPs. 456,543 Joint spaces typically are not narrowed. Chronic joint inflammation and effusion may lead to ligamentous laxity and result in joint deformities. The most common deformities include ulnar deviation at the MCPs, flexion and extension deformities of the IP articulations resembling swan neck and boutonnière deformities, and malalignment of the first carpometacarpal joint. These deformities are typically nonerosive and reducible (Jaccoud’s-type) and therefore are more visible on an oblique or lateral radiograph of the hand as compared with a postero-anterior radiograph, in which the pressure of the cassette may make the subluxations less pronounced. These nonerosive, flexible deformities are considered pathognomonic and are present in less than one half of patients with SLE who demonstrate articular abnormalities. Rarely these deformities eventually become permanent or fixed. Erosive changes may be seen with lupus, if subtle, and periarticular MRI may be needed for their detection. 474
Axial skeleton.
Although spinal changes are uncommon, atlantoaxial subluxation has been reported in patients with SLE. It is wise to obtain a lateral cervical flexion radiograph because this abnormality may be present and not apparent on a neutral lateral radiograph. 28
Unilateral or bilateral sacroiliitis, with radiographic features that are similar to those associated with seronegative spondylarthropathies, has been reported as an uncommon manifestation of SLE. 337
Chest.
Plain film chest radiography may be normal, or may reveal pleural or pericardial effusion, acute infiltrate, interstitial reticulation, or cardiomegaly. High-resolution chest CT may find evidence of airway disease and interstitial lung disease in patients without respiratory symptoms and with normal chest radiographs. 31,191 Chronic intersitial changes appear to predominate in the lower lung fields. 471
Osteonecrosis.
Avascular necrosis is a common complication in patients with SLE. The radiographic features are identical to those associated with osteonecrosis caused by factors other than SLE (see Chapter 11). The femoral condyle, humeral head, and femoral head are the most common sites involved; the latter is most affected. Other common sites include the proximal tibia and distal tibia. Although high doses of corticosteroids can significantly increase the risk of osteonecrosis, some treatment regimens may reduce this risk. 260 The disease process itself also seems to increase risk for developing osteonecrosis, because patients not receiving steroids also develop this condition. 336
Presentation.
The revised criteria for SLE must include four of the following: 629
• Malar rash
• Discoid rash
• Photosensitivity
• Oral ulcers
• Arthritis
• Serositis
• Renal disorder
• Neurologic disorder
• Hematologic disorder
• Immunologic disorder
• Antinuclear antibody
The clinical presentation varies according to the distribution of lesions and extent of systemic involvement. Many patients initially present with constitutional signs and symptoms (malaise, fever, and weight loss), polyarthritis, or a skin rash. The classic malar “butterfly” erythema may be noted but is only one of several cutaneous lesions that may present intermittently during the course of the disease. 346 The renal system is almost always involved, but the extent differs widely from one patient to the next. 18 Manifestations in any organ system (e.g., respiratory, cardiac, gastrointestinal, central nervous) may appear eventually. 579 Associated life-threatening conditions may include intestinal perforation and vasculitis, seizures, stroke, pulmonary embolus, and nephritis. Pregnancy may be related to an increase in the disease morbidity. 504
Laboratory tests.
The screening test for SLE detects the presence of ANAs, which are present in virtually all patients with SLE. Although this test is sensitive for SLE, it is not specific and therefore may be positive in nonlupus conditions. However, the presence of antibodies to native (double-stranded [ds]) DNA and anti–Sm antibodies strongly suggests SLE. Lupus erythematosus cells* also may be observed. Rheumatoid factor is found in a minority of patients, which may indicate an overlap syndrome other than true SLE.
*ANAs react with nuclei of damaged cells, which disrupt the cells’ chromatin structures and transform them into lupus erythematosus bodies. These bodies undergo phagocytosis by neutrophils to form lupus erythematosus cells.
Treatment and management.
The diagnosis of idiopathic lupus should be made only after ruling out the possibility of a drug-induced condition, which can be concluded if discontinuing use of a suspected drug alleviates all signs and symptoms. 260 Treatment depends on the location and severity of the disease. In mild cases it may involve counseling, use of sunscreen, exercise, and NSAIDs, whereas in more severe disease immediate corticosteroid or other immunosuppressive drug therapy may be necessary. 133,382 Unfortunately, the use of immunosuppressive drugs increases the risk of infection, which is currently a major cause of morbidity and mortality in these patients. 282 New drug therapies are being tested that may reduce disease activity. 263,642 Sex hormones are being investigated as potential therapeutic agents because of their immunomodulatory properties. 659
• Systemic lupus erythematosus (SLE) is an inflammatory connective tissue disorder that affects many organs (skin; vascular endothelium; central nervous system; and renal, hematologic, musculoskeletal, cardiovascular, pulmonary, and gastrointestinal organs).
• The disease is more common in blacks, 90% of cases are in women, and the majority of cases develop between 30 and 50 years of age.
• The metacarpophalangeal and proximal interphalangeal joints of the hands are affected, and nonerosive, flexible deformities are characteristic.
• Although not common, atlantoaxial subluxation may occur; therefore lateral flexion-extension radiographs of the cervical spine should be a consideration.
• The clinical presentation is marked by arthralgia, “butterfly” rash, ulcers in the nose and mouth, and constitutional signs and symptoms (e.g., fever and fatigue).
• Infection and nephritis are major causes of mortality in all stages of SLE.
• Laboratory tests include a test for the presence of antinuclear antibodies, anti–Sm antibodies, lupus erythematosus cells, and rheumatoid factor.
Scleroderma
BACKGROUND
Scleroderma, which literally means “hard skin,” describes progressive thickening of the skin from increased collagen deposits. The disease also is known as progressive systemic sclerosis (PSS), a term that more appropriately describes the entire disease process, because it is a connective tissue disorder characterized by small vessel disease, fibrosis, and excessive deposits of collagen that may affect not only the skin, but also the musculoskeletal system and internal organs (e.g., gastrointestinal tract, lungs, heart, kidneys). Scleroderma has been divided into two major classifications, localized and systemic, and subclassifications depend on the existence and extent of systemic involvement, as well as the rapidity of the disease progression. Localized scleroderma usually only involves the skin and may affect the musculoskeletal system to a limited degree. There are three subtypes: morphea (localized), generalized morphea, and linear scleroderma. Systemic sclerosis causes more widespread skin changes and may be associated with internal organ damage (lungs, heart, and kidneys). Systemic sclerosis has two subtypes: limited and diffuse. Systemic limited scleroderma also is known as CREST, an acronym for its most prominent features: calcinosis, Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly, and telangiectasia. Systemic diffuse scleroderma is the most serious form of the disease because of its severe onset and rapid progression.
Although the etiology is unknown, genetics, hormonal events, the immune system, and an environmental agent or trigger are believed to play important roles in its pathogenesis. * A positive family history appears to be the greatest risk factor, although the familial risk is still relatively low (<1%). 23 The prevalence in the United States has been noted to be 4.4 to 27.6 cases per 100,000, 414,613 with an incidence rate reported to range between 1.4 to 1.9 cases per 100,000. 414,613 It is unclear as to whether this rate is stable or on the rise. 413,426 The female-to-male ratio has been reported as 3:1, although in the United States it is approximately 8:1, 414,612,613 with the highest rates occurring during the childbearing years. There is evidence to suggest that the age of onset is later than has been reported in earlier studies, with the age of occurrence typically 35 to 65345,414 rather than 20 to 50. 611,612 In the United States African Americans are at a higher risk of developing scleroderma compared with whites, and young African American women appear to be stricken most often and most severely. 345,414,426,613
The majority of patients with scleroderma eventually develop joint involvement. The major abnormalities discovered on plain film examination are noted in the hands and include soft-tissue atrophy, osseous resorption, and subcutaneous calcification. Gastrointestinal contrast studies may reveal characteristic findings in the esophagus, small intestine, and large bowel that are primarily caused by fibrosis and atrophy. Plain film chest radiography may be negative or reveal signs of pulmonary hypertension or interstitial fibrosis.
Hands.
Atrophy of the soft tissues of the fingertips (acral tapering) is a very common feature, the incidence of which increases if the patient has accompanying Raynaud’s phenomenon. 35 Involved digits often have accompanying bony changes (acroosteosclerosis, acroosteolysis) and soft-tissue calcification. Bone resorption or erosion is noted frequently, primarily involving the tufts of the terminal phalanges (acroosteolysis) (FIG. 9-31FIG. 9-32 and FIG. 9-33). 581 Resorption may of lead to a “penciled” or pointed appearance of the phalanx; most of the entire distal phalanx may be destroyed with continued resorption. Erosions also involve the DIP and PIP articulations, but to a lesser degression distal tuft. 158 Erosion at the first carpometacarpal joint is a distinctive feature also, 582 and may lead to radial subluxation of the metacarpal base. Juxtaarticular or diffuse osteoporosis may be present. Joint space narrowing and marginal erosions are noted in up to 15% of patients. 51
 |
| FIG. 9-31 Scleroderma presenting on a bilateral posteroanterior hand view demonstrating characteristic resorption of the distal margins of the distal phalanges (acroosteolysis) (arrows) and foci of radiodense soft-tissue calcifications (arrowheads). |
 |
| FIG. 9-32 Acroosteolysis (arrow) and soft-tissue calcifications (arrowhead) of scleroderma. (Courtesy Gary Longmuir, Phoenix, AZ.) |
 |
| FIG. 9-33 Scleroderma causing prominent acroosteolysis of the hand (arrows). (Courtesy Joseph W. Howe, Sylmar, CA.) |
Subcutaneous calcifications.
The presence of subcutaneous and periarticular calcinosis is prominent in the hands and also may develop around other joints and over bony eminences (Fig. 9-34). 158,178,670 These calcifications may have a varied appearance, ranging from punctate, to sheetlike, to large focal conglomerations. Ulcerations, especially over bony prominences, may be a complicating factor. Paraspinal calcifications may lead to localized pain, stiffness, dysphagia, or neurologic compromise. 505,580
 |
| FIG. 9-34 Scleroderma exhibiting subcutaneous and periarticular soft-tissue calcification (arrows) of the, A, hand and, B, feet in this 62-year-old patient. Although fibular subluxations of the phalanges at the metatarsophalangeal articulations are evident, no signs of significant erosions are present. |
Gastrointestinal tract.
The gastrointestinal tract is frequently involved in systemic scleroderma, with the esophagus being involved up to 85%. Smooth muscle dysfunction causes esophageal aperistalsis and reduced lower esophageal sphincter pressure, resulting in gastroesophageal reflux and an increased incidence of peptic stricture and Barrett’s esophagus. The esophageal changes lead to dysmotility and may be reflected on plain film as air or air-fluid levels within the esophagus. 468 Esophageal involvement may be diagnosed by a barium swallow, which shows a “stiff glass tube” appearance. Barium studies initially may reveal rapid transit; esophageal reflux; dilatation of the esophagus and small bowel; and large-mouthed sacculations or pseudodiverticula in the colon, jejunum, and ileum. Over time barium studies reveal decreased motility and possibly obstruction.
Chest.
The lung is the most commonly involved internal organ after the gastrointestinal tract. The two major pulmonary manifestations associated with scleroderma are pulmonary hypertension and interstitial lung fibrosis. Pulmonary arterial hypertension has a high mortality rate and may occur in approximately 15% of PSS patients. It may develop secondary to pulmonary fibrosis or as an isolated complication. Therefore screening procedures should include Doppler-echocardiography and pulmonary function tests. 145
If the interstitial fibrosis is extensive enough to be visible on a plain chest radiograph, it will predominate in the lower lungs. The radiographic findings are characterized by fine reticular, partly nodular fibrosis. There may be thick linear radiopacities and thickened septae near the blood vessels. In later-stage or end-stage fibrosis, a more cystic or “honeycomb” pattern appears. HRCT significantly increases early detection of alveolitis and fibrosis, given that plain film chest radiography may appear unremarkable in the early stages.
Mandible.
Thickening of the periodontal membrane may create an increase in the radiolucent area between the tooth and mandible that is best noted on dental radiographs. The involvement is most visible around the molars or posteriorly located teeth.
CLINICAL COMMENTS
The patient should fulfill the major criterion or two of the minor criteria as defined by the American College of Rheumatology. 619
• Major criterion: proximal diffuse (truncal) sclerosis (skin tightness, thickening, nonpitting induration)
• Minor criteria:
• Sclerodactyly
• Digital pitting scars or loss of substance of the digital finger pads (pulp loss)
• Bibasilar pulmonary fibrosis
Changes in the skin’s appearance (e.g., thickness and fibrosis, tightening, shininess, atrophy), Raynaud’s phenomenon, 299 and arthralgias of the fingers may be the first signs of systemic sclerosis, although visceral involvement may have occurred already. 147,280,628 A thorough, multisystem evaluation is necessary to detect serious problems that may exist in a seemingly asymptomatic patient. 359 As noted, the gastrointestinal tract is the most common internal site affected, with complications including dysphagia, gastroesophageal reflux, Barrett’s esophagus, small bowel bacterial overgrowth, malnutrition, and intestinal pseudoobstruction. 26,206,602 Periodontal membrane thickening causes loose teeth, which further complicates maintaining good nutritional status. The heart, lungs, and kidneys also may become involved; pulmonary disease causes higher mortality than renal failure. 113,147,247,359 Scleroderma renal crisis, a condition that was considered almost certainly fatal, now is being treated successfully with angiotensin converting enzyme (ACE) inhibitors. 611
Laboratory tests.
No single test accurately and definitively determines a diagnosis of scleroderma. Laboratory tests may reveal an elevated ESR, the presence of rheumatoid factor in approximately 30% of patients, and the presence of serum ANAs in more than 90% of cases. A variety of disease-specific autoantibodies (e.g., anticentromere antibodies, anti–Schl-70) have been discovered, and are not only useful in the diagnosis of PSS, but also provide markers for certain clinical features. 24,264
The nail fold capillary test is a useful noninvasive test that examines the skin beneath the fingernail to determine the presence or absence of normal capillary function. Absence of normal capillary function may aid in confirming a suspicion of scleroderma, given that an early sign of systemic scleroderma is the disappearance of the capillaries in the skin of the extremities. 392,573
Treatment includes patient education, avoidance of temperature extreme, cessation of smoking to reduce digital vascular complications, 245 dietary modification, physical therapy and exercise, drug therapy, and surgery. Treatment and management are directed toward the varied systemic manifestations of the disease. 427,448,459,602 No generalized therapy for progressive systemic sclerosis has been proved to be effective. Evidence suggests that drug therapy should target one or all of the involved disease processes: vascular disease, autoimmune disorder, and tissue fibrosis. The extent of specific organ involvement must be known to make an appropriate treatment decision. 621 The continuous accumulation of information about pathogenesis of fibrosis in scleroderma and the numerous therapies that are being studied provide hope for the development of a successful treatment or disease-modifying therapy for the complications of this condition. 335,343,459,570
It should be noted that certain chemical compounds (vinyl chloride), solvents (aromatic hydrocarbons), minerals (silica), pesticides, and drugs can induce scleroderma-like disease. 249,251 This should be a consideration if exposure is a possibility in the patient’s work environment or the patient’s drug history is suspicious.
• Scleroderma is a connective tissue disorder that affects the skin, musculoskeletal system, and internal organs.
• It is divided into two major classifications, limited and systemic, based on the extent of involvement.
• In the United States, women are eight times more likely to develop the condition than men.
• The disorder typically develops between 30 and 50 years of age.
• The hands develop distal tuft resorption (acroosteolysis), acral tapering caused by soft-tissue atrophy, and subcutaneous calcinosis.
• Major pulmonary manifestations include hypertension and interstitial fibrosis.
• Gastrointestinal manifestations include esophageal dysmotility and large-mouthed (wide-mouthed) bowel sacculations.
• Laboratory tests may reveal an elevated erythrocyte sedimentation rate, the presence of rheumatoid factor in 30% of patients, and the presence of serum antinuclear antibodies in 90% of patients.
• Specific autoantibodies may aid in the diagnosis of lupus, and provide clues about the onset and prevalence of related clinical feature.
• Certain chemicals and drugs may produce scleroderma-like disease.
Polymyositis and Dermatomyositis
BACKGROUND
Polymyositis and dermatomyositis are two of the three idiopathic inflammatory myopathies. The third, inclusion-body myositis, has most recently been discovered to be a separate entity from polymyositis. The incidence of polymyositis/dermatomyositis has been noted at 0.8 cases per 100,000, with a prevalence of 5.1 cases per 100,000, 288 although these estimates may not be not reliable because the criteria used likely failed to separate inclusion-body myositis from polymyositis. 130,407 The widely used classification system61 was developed before these two entities were found to be distinct. The female-to-male ratio is approximately 2:1. 288 The age at the time of diagnosis typically ranges from 40 to 70 years, with 52 years of age being the mean onset. 393 Dermatomyositis may affect children and adults. 240 Polymyositis is rarely seen before the second decade of life.
The etiology is unknown. However, like most connective tissue disorders, it is believed that an autoimmune disorder631 is responsible for the mechanism of damage, which revolves around a genetic predisposition (there is an association with HLA genes) 208,587 and an environmental trigger or initiating factor. 539 Failure of apoptosis, or programmed cell death, is believed to play a major role in the pathogenesis of inflammatory muscle disease. 507 Both polymyositis and dermatomyositis are nonsuppurative inflammatory disorders that lead to subsequent fibrosis and degeneration of striated muscle and result in muscle atrophy and weakness. Predominant muscle involvement is that of the large muscles of the proximal portions of the upper and lower extremities. In addition, dermatomyositis involves the skin.
IMAGING FINDINGS
The radiographic manifestations of polymyositis and dermatomyositis usually are discussed by dividing them into two major categories: soft-tissue and articular abnormalities.
Soft-tissue abnormalities.
Initial soft-tissue changes are associated with swelling and edema in the subcutaneous tissue and muscle, particularly affecting the proximal appendicular skeleton in a bilaterally symmetric presentation. 616 Radiographically these changes appear as an increase in the soft-tissue density and poor delineation, blurring, or loss of the fascial plane lines. Extensive edema of the subcutaneous tissue may allow visualization of thickened septa. Chronic disease is associated with a loss of soft-tissue mass or bulk resulting from muscle atrophy and marked osteoporosis of the long bones and vertebral bodies.
Soft-tissue calcification is the most striking radiographic abnormality in polymyositis and dermatomyositis. It is uncommon in adults but occurs in approximately 25% to 50% of children (Fig. 9-35). 622 Soft-tissue calcifications can be subdivided by location into subcutaneous and intermuscular. Calcinosis cutis, or scleroderma-like subcutaneous calcifications, may appear as firm nodules or plaques commonly over bony prominences. These may be associated with skin ulcerations, infection, and pain, 132especially at sites of compression. Small, diffuse, linear or curvilinear subcutaneous calcifications also may be evident. Calcification at the fingertips may be associated with terminal tuft erosion.
 |
| FIG. 9-35 Soft-tissue calcifications of dermatomyositis. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Intermuscular calcifications generally are asymptomatic and predominate in the proximal large muscles of the upper and lower extremities. The classic radiographic appearance is large calcareous masses or “tumoral” deposits in the fascial planes. In severe forms they may cause loss of function or bone formation in place of calcification.
Joints.
Joint involvement occurs but is infrequent. Typically the associated arthritis is transient and nondeforming. The most common abnormalities are periarticular osteoporosis and soft-tissue swelling. Destructive joint changes have been reported, although there is discussion as to whether this erosive presentation is representative of overlap syndromes. Radiographic changes that have been described include soft-tissue swelling, small periarticular calcifications and erosions involving the DIP, PIP, and MCP articulations of the hands, and radial subluxations or dislocation of the IP joint of the thumb (“floppy thumb” sign). 91 Joint contractures may occur and are most commonly associated with dermatomyositis.
CLINICAL COMMENTS
Patients with polymyositis and dermatomyositis typically present with fatigue, myalgia, and varying degrees of proximal muscle weakness that is usually symmetric and develops over weeks or months. Gross movements such as lifting or climbing stairs are affected, whereas fine motor skills usually are not affected until late in the disease process. “Head drop” may occur if the extensor muscles of the neck are affected. Sensation and tendon reflexes remain normal, although the latter may be absent in severe cases of muscle atrophy. Pain is present in a minority of patients. 130 Dysphagia and pulmonary symptoms may be present depending on muscle involvement.
In patients with dermatomyositis, characteristic skin manifestations may precede or less commonly accompany the onset of muscle weakness. These include (a) a heliotrope rash that appears as a bluish-purple discoloration on the upper eyelids; (b) an erythematous rash that may occur on the face, “V” of the neck and chest (“V” sign), upper back and shoulders (shawl sign) or the knees, elbows, and malleoli; (c) a Gottron rash, which appears as papules over the bony prominences, especially the MCP and IP articulations; 98 and (d) dermatitis affecting the scalp. 310 Thickened and distorted cuticles and telangiectasis at the fingernail base also may occur.
Laboratory tests.
Several tests are useful in evaluating muscle disorders, including serum muscle enzyme concentrations, urinary creatine and creatinine excretion, electromyogram, and muscle biopsy. The characteristic findings in patients with dermatomyositis and polymyositis are elevated serum enzyme and urinary creatinine levels, an abnormal electromyogram, and muscle biopsy findings consistent with inflammation (myositis). In addition, skin biopsy may be needed in certain cases of dermatomyositis.
Treatment and management.
Treatment is directed toward increasing muscle strength and relieving other associated manifestations of the disease (e.g., rash, arthralgia). A combination of pharmaceuticals and physical activity should be included in the treatment regimen. Studies have shown that patients may benefit from a therapeutic exercise program to improve function and increase strength. 9,170,254,374,680 Regarding drug therapy, Dalakas and Hohlfeld recommend a sequential, step-by-step, empiric, escalating approach (that may be modified) that successively employs corticosteroids, immunosuppressive therapy, 109 intravenous immunoglobulin therapy, 111,131 and an immunosuppressive drug. 130
Other factors that must be considered in the management of polymyositis and dermatomyositis patients are the likelihood of dysphagia resulting from esophageal disease, cardiac abnormalities, pulmonary abnormalities, 260 and the increased risk of specific cancer types. 261,262,598 Patients should be assessed and monitored for these complications.
Ultrasound and MRI may be helpful in defining involved muscle groups and possible associated features such as tenosynovitis and tendon nodules, as well as assessing the degree of involvement and possible response to therapy.
• Polymyositis and dermatomyositis are forms of idiopathic inflammatory myopathies in which there is inflammation, fibrosis, and loss of muscle fiber leading to muscle atrophy that affects strength and function.
• Involves the striated muscle; especially the large muscles of the proximal aspects of the upper and lower extremities.
• Bilateral, symmetric muscle involvement.
• Women are affected 2:1 more than men.
• Dermatomyositis has characteristic skin manifestations that include a heliotrope rash and Gottron rash.
• The most striking and characteristic radiographic features are soft-tissue calcifications, which present as subcutaneous or intermuscular.
• Joint involvement usually is limited to soft-tissue swelling and periarticular osteoporosis, although erosive changes have been noted in the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of the hands.
• Characteristic laboratory results are increased serum enzyme and urinary creatinine levels, an abnormal electromyogram, and muscle biopsy finding consistent with inflammation.
• Exercise therapy, corticosteroids, immunosuppressants, and intravenous immunoglobulin therapy are part of the treatment protocol.
• Polymyositis and dermatomyositis carry an increased association with certain cancer types.
• Pulmonary and cardiac abnormalities may exist.
Jaccoud’s Arthropathy
BACKGROUND
Jaccoud’s arthritis (arthropathy, disease, or syndrome) is a nonerosive, relatively asymptomatic deforming arthropathy of the hands and feet. It was initially described in 1867 (and for some time thereafter) as a rare complication of rheumatic fever (chronic postrheumatic fever arthritis). 287,595 Jaccoud’s arthropathy has since been reported in patients without a previous history of rheumatic fever, and is now more commonly seen in association with connective tissue disorders, such as systemic lupus, 660 scleroderma69 and dermatomyositis, 71 psoriatic arthritis, 641 sarcoidosis, Parkinson disease, and lung disease. * The condition often is called deforming nonerosive arthropathy or Jaccoud’s-type arthropathy when it occurs in non–postrheumatic patients.
Although the etiology is unclear, biopsy studies reveal no evidence of synovial pathology and do not indicate the presence of a synovial inflammatory condition. Jaccoud’s arthropathy is characterized by articular deformities believed to result from capsular inflammation and fibrosis, and in certain cases secondary degenerative changes are noted that presumably result from long-standing joint deformities. 215,646
IMAGING FINDINGS
The hallmark of Jaccoud’s arthropathy is nonerosive, reversible joint deformity, although eventually the deformities may become fixed (Fig. 9-36). The joint deformities cannot be actively corrected by the patient but can be corrected by an examiner if the patient relaxes the joint. Radiographic examination of the hands may reveal this passive reducibility; when the cassette puts pressure on the hand during the PA view, the hand is restored to nearly normal alignment, but the deformities become apparent during the oblique radiography procedure.
 |
| FIG. 9-36 Jaccoud’s arthritis marked by ulnar deviation of the first to fourth digits at their metacarpophalangeal joints. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Hands and feet.
The most common deformities in the hands are flexion and ulnar deviation of the MCP joints, which is most marked in the fourth and fifth digits, and in the foot, flexion and fibular deviation of the MTP articulations. 449 Hallux valgus also may be present in the foot. Swan neck and boutonnière deformities of the digits also are noted (see Rheumatoid Arthritis for descriptions of these deformities), 320 and are more common when associated with an autoimmune disorder such as RA or SLE. A Z-deformity is observed when the thumb is affected. The bone density may be normal or exhibit periarticular osteoporosis. Usually the joint space is preserved until late in the disease, when mechanical stress of the accompanying subluxation may cause secondary degeneration. Osseous erosions are rare, but when they occur they appear as “hook lesions” on the radial and palmar aspect of the metacarpal heads. 490
CLINICAL COMMENTS
Jaccoud’s arthropathy is no longer considered a rare condition and should be mentioned in the differential diagnosis of chronic arthritis. 449 The pattern of joint involvement mimics that of RA and SLE; therefore it may be misdiagnosed given that these diseases also lack erosions early in their course. Laboratory tests may help establish the correct diagnosis because patients with Jaccoud’s arthropathy typically have negative tests for the rheumatoid factor and ANA. Patients with Jaccoud’s arthropathy (despite its striking deformities) usually have no pain, little or no evidence of synovitis, and good functional capabilities. In fact, the arthropathy may not be the reason the patient is seeking care.
• Jaccoud’s arthropathy is a chronic arthritis that follows rheumatic fever, although it is now seen more in association with connective tissue disorders such as systemic lupus erythematosus.
• It is often an asymptomatic, nonerosive arthritis that is marked by reversible joint deformities.
• It is characterized by ulnar deviation of the second to fifth fingers and subluxations of the metacarpophalangeal joints. Similar findings may involve the metatarsophalangeal joints of the feet.
Seronegative Spondyloarthropathy
The seronegative spondyloarthropathies are a group of interrelated, sometimes overlapping but distinct inflammatory conditions of unknown cause that have a high prevalence of HLA-B27 antigen, and an affinity for the axial skeleton (spine and SI joints), entheses sites (bony attachments of tendons or ligaments), and to varying degrees the peripheral joints. In addition, they have several common extraarticular manifestations (e.g., iritis, skin lesions). This group of diseases is composed of AS, arthritis of inflammatory bowel disease (enteropathic arthritis), Reiter’s syndrome, psoriatic arthritis, and undifferentiated spondyloarthropathy.
Ankylosing Spondylitis
BACKGROUND
Ankylosing spondylitis, also called Bechterew disease or Marie-Strümpell disease, is the most common of the seronegative spondyloarthropathies, affecting approximately 0.1% to 0.2% of white North Americans, 301 with a prevalence of 68 to 197 per 100,00 people in the United States. 655 It is a chronic, progressive, inflammatory condition involving predominantly the synovial and cartilaginous joints of the axial skeleton and often the large, proximal appendicular joints. Alterations at entheses, the sites where ligaments and tendons attach to bone, also are a prominent feature.
Although the etiology remains unknown, the high prevalence (>90%) of the genetic marker HLA-B27 in white patients with AS57,78,227 as compared with the prevalence of the antigen in unaffected white patients (6% to 8%) suggests that the disease occurs in persons with a genetic predisposition, 77,301,450 and may be triggered by an environmental factor. The onset is usually between 15 and 35 years of age186 and typically presents as an insidious onset of low back pain and stiffness. The time period between the first spondyloarthritic symptom and the diagnosis may be years, and is longer in those patients who are HLA-B27 negative. 186 The disease is more common and severe in men, with ratios of 1:1 to 10:1 reported. 142,163,170,294,655 There is the possibility of underreporting in women, in whom the clinical presentation is not as consistently “classic” as in men. The spinal involvement appears less severe in women. Sacroiliitis is more likely to be asymptomatic, and there is an increased frequency of peripheral arthritis. 174,226
IMAGING FINDINGS
Plain film radiography is still the conventional mode of imaging for AS and all of the seronegative spondyloarthropathies, probably because of its accessibility and cost. However, because of its lack of sensitivity to the early stages of the disease and consequent delay in disease diagnosis, other modalities such as MRI, CT, ultrasound, and bone scintigraphy may become more heavily used for diagnosis confirmation and monitoring disease progression, depending on the stage of the disease and area of involvement. 209,375,432
Radiographic findings, regardless of the location, reflect the underlying inflammatory condition associated with AS, which is characterized by erosions, osseous proliferation, and bony ankylosis. Joint involvement in the axial and appendicular skeleton is typically bilateral and symmetric, although this may vary early in the disease process.
Sacroiliac joint.
The SI joint is the classic site of initial involvement in AS and usually is symmetric. The ensuing changes may affect both the ligamentous and synovial portions of the joint, but predominate in the middle and lower two thirds of the articulation. The articulating surface of the ilium shows earlier and greater radiographic involvement than the sacral surface apparently resulting from less protection from the thinner iliac cartilage. 45 The early stages of the disease are characterized by subtle periarticular osteoporosis and loss of cortical bone definition. More obvious erosions develop, leading to irregular joint margins and joint space widening. Patchy and ill-defined reactive sclerosis accompanies the erosions and becomes more diffuse and uniform as the disease advances (Fig. 9-37). Bony bridges form across the joint, and lead to eventual fusion or ankylosis, which appears radiographically as obliteration of the SI articulation. After ankylosis occurs, the reactive sclerosis is resorbed, and generalized osteoporosis becomes a prominent feature. Approximately 50% of patients progress to complete SI fusion (FIG. 9-38FIG. 9-39 and FIG. 9-40).
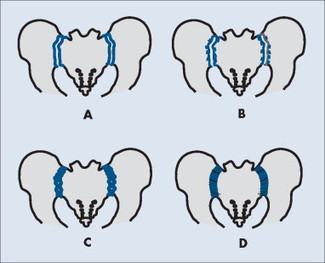 |
| FIG. 9-37 A, Normally the sacroiliac joint margins are well defined. B, Inflammation may initially appear hazy with loss of cortical definition. Progression leads to joint space widening, C, erosions, and, D, fusion. |
 |
| FIG. 9-38 Normal sacroiliac joint. A, Because of its obliquity, the normal sacroiliac joint appears as a double projection (anterior margin of the joint is lateral and posterior margin of the joint is medial) in the anteroposterior or, to a lesser extent, posteroanterior projection. B, An oblique projection of the joint allows the examiner to better visualize the joint without the confounding double projection. In all views, the cortical margins of the joints should be well defined and continuous (arrowheads). Sacroiliitis presents with ill-defined and interrupted margins of the joint. |
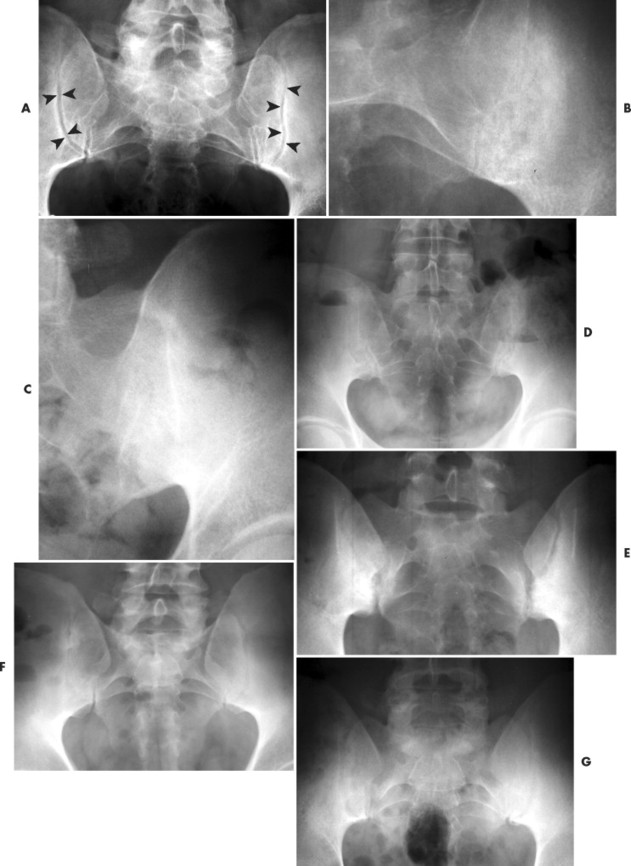 |
 |
| FIG. 9-39 A, Normal sacroiliac joints and, B to I, multiple cases of early sacroiliitis in ankylosing spondylitis. Early involvement presents with an irregularity of the normally well-defined cortical margins of the joint. The erosions in the joint surface become noticeable as the disease progresses. |
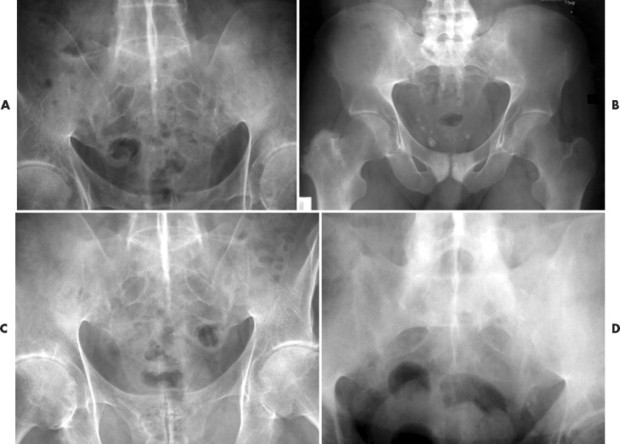 |
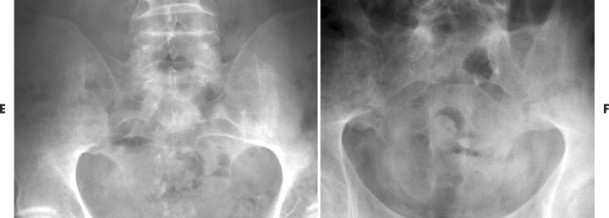 |
| FIG. 9-40 A to D, Multiple cases of sacroiliac joint fusion in ankylosing spondylitis. Joint fusion results in an absence of the normal thin, radiodense, vertically curvilinear cortical margins and joint space (see FIG. 9-37FIG. 9-38 and FIG. 9-39). E to F, Multiple cases of sacroiliac joint fusion in ankylosing spondylitis. Joint fusion results in an absence of the normal thin, radiodense, vertically curvilinear cortical margins and joint space (see FIG. 9-37FIG. 9-38 and FIG. 9-39). (B, Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Early changes in the SI joints are not well visualized, if at all, on plain film radiography. The diverging rays of a pelvic radiograph taken in the anterior to posterior direction directly opposes the plane line of the joint, and therefore cannot clearly define the subchondral bone or joint space because of superimposition. Two ways to optimize visualization are to (a) perform a posterior to anterior examination and decrease the tube distance to 90 cm, thereby attempting to parallel beam and joint divergence; and (b) perform two separate oblique radiographs (Figs. 9-38, B) for each joint with a caudocranial tube angulation. Plain film radiographs may still be negative given the subtlety of these findings in combination with the complexity of the SI joint surfaces, and other more sensitive modalities such as MRI or CT may be needed. 375,432
Spine.
Spondylitis occurs in about 50% of patients and as a rule develops after SI disease, with the thoracolumbar and lumbosacral junctions being the most common initial target sites. 152,220 The disease process typically ascends the spine contiguously without skip lesions and progresses bilaterally and symmetrically. The most characteristic spinal finding occurs at the discovertebral junction, but the inflammatory process also may affect the apophyseal joints, posterior ligamentous attachments, costovertebral joints, and atlantoaxial joint (FIG. 9-41FIG. 9-42FIG. 9-43FIG. 9-44FIG. 9-45FIG. 9-46 and FIG. 9-47).
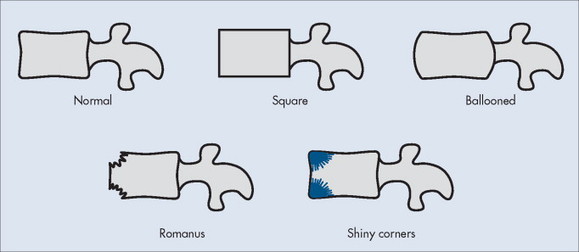 |
| FIG. 9-41 Several key radiographic features of ankylosing spondylitis are noted in the lateral projection, including thin marginal syndesmophytes (see Fig. 9-42), a square or ballooned configuration of the vertebral body (as opposed to the normal slight concavity of the anterior and posterior margins of the vertebral body), sclerotic “shiny” corners of the vertebrae (representing reactive sclerosis to the enthesopathy), and small erosions at the corners of the vertebral body, known as Romanus lesions. |
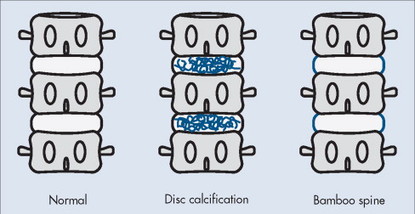 |
| FIG. 9-42 As with other conditions of spinal hypomobility, dystrophic calcification of the intervertebral disc may occur with ankylosing spondylitis. A hallmark feature of ankylosing spondylitis is the formation of thin sydnesmophytes, connecting adjacent vertebrae. In the anteroposterior view the thin sydnesmophytes bow outward slightly, giving the spine the appearance of a bamboo stick. |
 |
| FIG. 9-43 Rarely ankylosing spondylitis manifests with advanced endplate destruction, known as an Andersson lesion, mimicking an infection. |
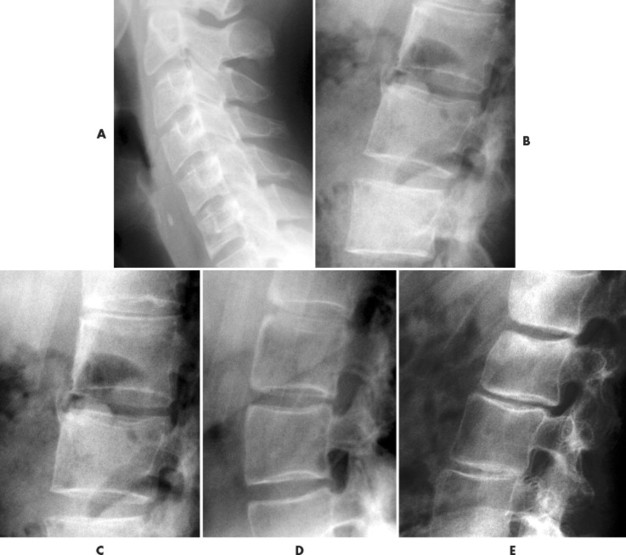 |
| FIG. 9-44 A to C, Multiple cases of square and, D and E, ballooned vertebra in different patients with ankylosing spondylitis. |
 |
| FIG. 9-45 A and B, Shiny corners in two patients with ankylosing spondylitis (arrows). |
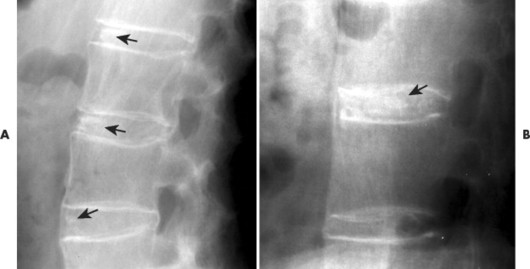 |
| FIG. 9-46 A and B, The spinal fusion associated with ankylosing spondylitis often results in dystrophic calcification of the involved intervertebral discs (arrows). |
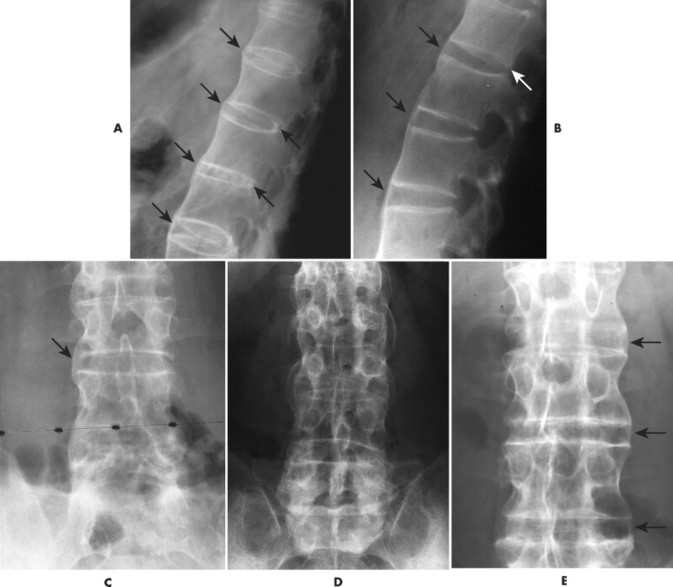 |
| FIG. 9-47 A and B, The thin marginal syndesmophytes (arrows) characteristic of ankylosing spondylitis appear fairly straight in the lateral projection but are more curved in, C, the frontal projection. In the frontal projection, the curved syndesmophytes give the spine, especially the lumbar spine, an appearance that has been likened to a bamboo stick. D, A second and, E, third, slightly oblique, is presented. |
Discovertebral junction.
The classic spinal findings associated with AS are thin, vertical ossifications or syndesmophytes that bridge adjacent vertebrae and cause ankylosis of multiple segments. Complete ankylosis occurs as the disease progresses, resulting in a distinctive, undulating spinal outline that radiographically resembles a piece of bamboo. The classic “bamboo spine” occurs in a minority of patients and takes an average of 10 years to develop (see Figs. 9-42 and 9-47).
A syndesmophyte begins as a focal osteitis or erosion with surrounding sclerosis at the anterior vertebral body margins. The small corner erosions, or Romanus lesions, combined with new bone formation in the anterior curve of the vertebrae, lead to a loss of the normal anterior body concavity and may cause vertebral “squaring,” which is most apparent in the lumbar spine (see Figs. 9-41 and 9-45). This early finding often is overlooked, but new techniques are being designed to evaluate this subtle change in an attempt to aid early radiologic diagnosis and assess spinal progression. 533 The radiographic brightness of reactive sclerosis is intensified by the accompanying vertebral body osteoporosis and is appropriately called the shiny corner sign. Ossification then develops in the outer annular fibers and results in thin, marginal syndesmophytes that are predominantly found on the anterolateral aspects of the spine but can arise posteriorly and may cause symptomatic spinal stenosis. 239
Other abnormalities occurring at the discovertebral junction include discal calcification (see Fig. 9-46), which is common to many conditions of spinal hypomobility; discal ballooning, which is found in the later stages of spinal ankylosis as osteoporosis causes the endplates to weaken and become biconcave (fish vertebrae) and the disc to appear “ballooned” or biconvex; and Andersson lesions, which are discovertebral erosions or a destructive process that result from inflammation and stress fractures in the ankylosed spine (posttraumatic pseudoarthrosis). 153
Rarely the discovertebral junction undergoes advanced destruction and sclerosis, known as an Andersson lesion (see Fig. 9-43). The appearance is easily confused with an infection of the disc. The presence of radiographic features of AS of the posterior elements and other spinal levels is an important differential clue.
Apophyseal joints and posterior ligaments.
Ankylosis of the apophyseal joints is secondary to an underlying erosive process followed by reactive sclerosis that leads to osseous fusion and capsular ossification. This process is considered a prerequisite for the postural changes of reduced lumbar and cervical lordosis, and the increased thoracic kyphosis associated with patients in the later stages of the disease (Fig. 9-48). One study that examined 50 radiographs of the cervical and lumbar spine demonstrated greater involvement of apophyseal joints than in bridging syndesmophytes, suggesting the possibility that the apophyseal joint is primarily involved in AS. 139 The lateral cervical radiograph well demonstrates the changes in the apophyseal articulations. Oblique radiographs may be needed in the thoracic and lumbar spine to better visualize these changes. Radiographically, bilateral apophyseal fusion resembles two thick, vertically oriented linear radiopacities, which are known as the railroad track sign on the anteroposterior (AP) radiograph. If this appearance is present in combination with ossification of the interspinous and supraspinous ligaments, the resulting three vertical stripes are called the trolley track sign. The single vertical stripe caused by ossification of only the supraspinous and interspinous ligaments is called the dagger sign (FIG. 9-49FIG. 9-50FIG. 9-51FIG. 9-52 and FIG. 9-53).
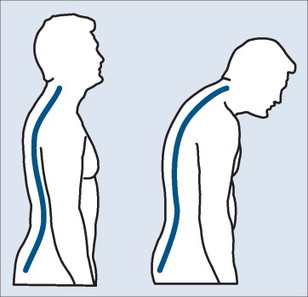 |
| FIG. 9-48 Advanced ankylosing spondylitis results in an increased thoracic kyphosis, loss of lumbar lordosis, and an anterior weight-bearing posture of the cervical spine. |
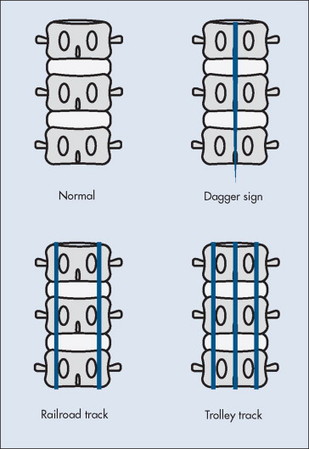 |
| FIG. 9-49 Ossification of the supraspinous and interspinous ligaments results in a midline, thin, vertical radiodense band running down the lumbar spine, known as a “dagger” sign. Fusion of the capsular ligament of the posterior joints causes similar bilateral radiodense vertical bands to be seen in the frontal radiographic projection. The appearance of only the capsular ligament bands is termed a “railroad track” sign. When the dagger sign and railroad track sign coexist, the configuration of the three vertical bands is termed a “trolley track” sign. |
 |
| FIG. 9-50 Trolley track sign. In the frontal radiographic projection, ankylosing spondylitis may appear with three radiodense vertical bands. The appearance has been likened to the three rails of a trolley track, hence the term trolley track sign to describe the appearance. The outer vertical bands represent ossification of the posterior joints (known as a railroad track sign when present alone) (arrows), and the midline radiodense band is secondary to ossification of the supraspinous and interspinous ligament (known as a dagger sign when found alone) (arrowheads). |
 |
| FIG. 9-51 Dagger sign. In the frontal projection, ossification of the interspinous and supraspinous ligaments appear as a midline radiodense vertical band in the lumbar spine known as the dagger sign (arrowheads). (See also Fig. 9-49.) |
 |
| FIG. 9-52 Railroad track sign. A 26-year-old male patient with fusion of the posterior joints secondary to ankylosing spondylitis. The fused posterior joints appear as parasagittal radiodense vertical bands in the frontal projection, nicknamed a railroad track sign (arrowheads). |
 |
| FIG. 9-53 Fifty-three-year-old male patient with ankylosing spondylitis. Characteristic features of the disease are noted by fusion of the sacroiliac joints, fusion of the posterior joints and ossification of the interspinous and supraspinous ligaments (trolley track sign), bilateral concentric loss of joint space of the hips, and osteopenia. |
Costovertebral and costotransverse joints.
Osseous fusion of the costovertebral and costotransverse joints is responsible for the limited chest expansion and chest or thoracic spine pain associated with AS. 356 It is difficult to visualize on plain film and may require specialized imaging such as radionuclide scintigraphy (hot scan initially, and cold once fused) or CT. 356,499 Involvement of the sternoclavicular joints also may be present.
Spinous processes.
Spinous process involvement is most common at the cervicothoracic junction, and appears as “whittling” or “sharpening” of the spinous processes secondary to subligamentous erosions.
Cervical spine.
Special attention should be given to the cervical spine, although involvement typically occurs later in the disease process than involvement in the thoracic and lumbar regions (Fig. 9-54). 87,381 In addition to the universal changes noted throughout the spine, atlantoaxial instability may develop with a rate of occurrence that has been noted to range between 2% and 23%. 275,534 Atlantoaxial instability in AS is less frequent and severe, but mimics the atlantoaxial involvement seen in patients with RA. Inflammatory changes of the synovium and adjacent ligamentous and osseous structures may lead to atlantoaxial subluxation, cranial settling, odontoid erosions, or complete destruction of the dens. Anterior atlantoaxial subluxation appears to be the most common presentation.
 |
| FIG. 9-54 A, Normal and, B to D, three cases of abnormal lateral cervical projections. The normal study exhibits loss of the normal cervical lordosis, but the vertebrae are of normal configuration and the posterior joints spaces are clearly seen (arrows). The abnormal cases reveal a loss of the posterior joint spaces secondary to joint fusion occurring with anklylosing spondylitis. (B, Courtesy Robert Tatum, Davenport, IA.) |
Spinal fractures associated with AS usually are caused by extension injuries and may occur even after minor trauma. 262 Fractures may occur in any spinal region; however, they are most prevalent in the cervical spine. These may be difficult to detect with plain films and CT; MRI or bone scans may be necessary. 221 With the ankylosed spine, fractures involve all three columns of the spine; therefore they are unstable with significant incidence of neurologic injury. 196,224 Resultant pseudoarthrosis in the cervical spine is extremely rare. It also is rare in the thoracolumbar spine, but not to the degree noted in the cervical spine. 140
Appendicular skeleton.
Peripheral arthritis occurs in approximately 40% of AS patients; 227 the hips, shoulders, knees, and small joints of the hands and feet are the most commonly affected sites.
Hips.
AS has a particular affinity for the large proximal joints (rhizomelic spondylitis), primarily the hip, which it affects in approximately 25% of patients (Figs. 9-55 and 9-56). 87 The associated radiographic findings are consistent with any inflammatory disorder, and include concentric joint space narrowing, mild erosions, subchondral cysts, ankylosis, and rarely acetabular protrusion. Bony proliferation may occur as femoral osteophytosis, which begins at the lateral margin of the femoral head and progresses to form a circumferential ring around the femoral neck (Fig. 9-56). Hip disease is more prevalent in patients with an early age of onset, and appears to be a prognostic marker for long-term severe disease and more severe cervical spine involvement. 86
 |
| FIG. 9-55 Anteroposterior projection of the pelvis revealing bilateral fusion of the sacroiliac joints consistent with ankylosing spondylitis. The projection also demonstrates bilateral concentric joint space reduction of the hips (direction of arrows). |
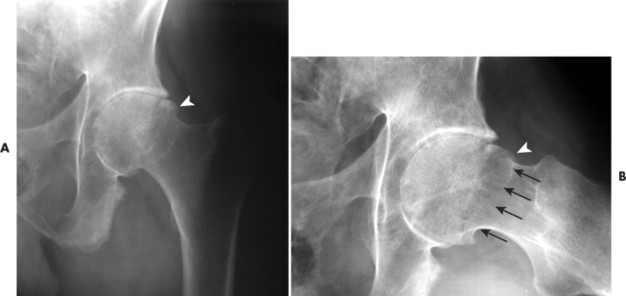 |
| FIG. 9-56 A and B, Ankylosing spondylitis presenting with joint space reduction of the superior, axial, and medial aspects of the hip equally. In this case, a 58-year-old man with ankylosing spondylitis exhibits mostly even reduction of the illofemoral space, a feature of inflammatory joint disease. Also, a small osteophyte on the lateral aspect of the femoral head is present as an early finding associated with ankylosing spondylitis (arrowheads). With disease progression a ring of osteophytes occurs around the femoral neck (arrows). |
Shoulders.
The glenohumeral joint is the second most common peripheral joint affected. Involvement is usually bilateral, and the osteoporosis, joint space narrowing, erosions, and proliferative changes typically mirror those in the hip. More severe erosions may occur on the lateral margin of the humeral head, and may progress to the appearance of a “hatchet” sign, in which the entire lateral aspect is destroyed. Chronic involvement also may lead to rotator cuff disruption, which is noted on the radiograph as elevation of the humeral head relative to the glenoid cavity.
Enthesopathy.
Enthesopathy is an inflammation at the insertion of tendons and ligaments into bone, and appears to be the hallmark of inflammatory spondyloarthropathies such as AS. 40 These changes usually occur in a bilateral and symmetric manner. 220 Bony erosions and osseous proliferation at entheses are common and most notably affect the pelvis (upper portion of the SI joint, ischial tuberosities and spines, iliac crests, symphysis pubis, greater and lesser trochanters), the plantar or posterior aspect of the calcaneus, and the anterior aspect of the patella. This reactive new bone is termed periostotic whiskering, which describes its frayed radiographic appearance (Fig. 9-57). Similar changes may develop around the shoulders and involve the AC articulations, coracoid process, and greater tuberosity of the humerus.
 |
| FIG. 9-57 Clearly visible periostotic “whiskering” of the ischial tuberosities on the radiograph of a man with ankylosing spondylitis (arrows). |
Lungs.
In addition to the characteristic skeletal changes associated with AS, pulmonary involvement also is a well-known feature. Pleuropulmonary disease has been reported to affect 1% to 2% of AS patients. 558 The classic manifestation is upper lobe interstitial fibrosis. The use of HRCT in addition to plain film chest radiography is revealing much more diverse involvement (nonapical interstitial lung disease, bronchiectasis, emphysema, mediastinal lymphadenopathy), as well as a higher percentage of affected patients. 190,329,583
CLINICAL COMMENTS
Early diagnosis of patients with AS may be delayed because of the mild and vague clinical presentation, nonspecific laboratory findings, and subtle radiographic changes. The initial complaint usually includes an insidious onset of low back pain and morning stiffness, which is relieved with activity and aggravated by resting in the supine position. Fifteen percent of patients have shoulder or hip pain as the initial complaint. 544 Acute iritis is rarely the initial complaint, although eventually this becomes one of the most common extraarticular manifestations and occurs in 25% to 30% of patients. 544 Additional early physical findings may include limited range of motion, limited chest expansion, postural changes (to ease back pain), fever, fatigue, anorexia, weight loss, and anemia. Neurologic signs and symptoms may include radiating leg pain that does not extend below the knee, cauda equina syndrome, and myelopathic changes caused by stenosis or a fracture. 170,234,421 Extraskeletal manifestations include heart disease (especially aortic insufficiency), upper lobe pulmonary fibrosis, and inflammatory bowel disease.
Pain is intermittent in the early stages, but pain and stiffness become more constant as the disease progresses. It has been noted that symptoms actually diminish or disappear in late-stage disease, with ossification of the paraspinal ligaments and apophyseal joints. 353Other studies do not concur and report continued daily pain and stiffness. 227 An increase or recurrence of pain after diminution may signal a superimposed complication such as a fracture. 489,551 Spinal or “carrot stick” fractures are common and usually are a result of seemingly minor trauma, such as slipping, to bone that has become severely osteoporotic because of disease-related ankylosis or surgical fusion. 435 Patients with AS are at an increased risk of spinal cord injury, which occurs most commonly in the cervical spine. 5
Diagnosis of AS is confirmed by radiographic examination. Although plain film radiography is not the most sensitive for the early changes associated with AS, it is still the primary and most widely used imaging modality for the diagnosis and assessment. If a spinal plain film is being used for a baseline study, repeating the radiograph in 6 months may be beneficial to detect early changes. PA radiographs of the hands and feet should be included at baseline, and follow-up radiographs are based on clinical features. If assessing progressive structural damage, serial films of the pelvis and cervical, thoracic, and lumbar spine should not be taken more frequently than annually. 473 Several radiologic scoring systems have been developed for the evaluation of AS. The most commonly used system is the New York criterion, which scores the SI disease on a scale from 0 to 4: 0 is normal; 4 is severe. 41 A more recently proposed system is the Bath Ankylosing Spondylitis Radiology Index (BASRI), which not only grades the SI joints, but also the lumbar and cervical spine. SI grading with BASRI is based on the New York system. 377
Because of its lack of sensitivity for early synovial and bony changes, use of plain film radiography alone may significantly delay the diagnosis. MRI, CT, and other imaging techniques are playing expanding roles to aid in earlier diagnosis and provide a better understanding of treatment response. 27,93,535,536 Investigators are discovering relationships between specific radiographic findings and how they relate to the patient’s physical signs and symptoms and long-term prognosis. 86,358,632,665 One example is the relationship of hip disease as an indicator of more progressive spinal changes and long-term severe disease. 86 These types of correlations will eventually aid assessment, treatment, and evaluation of disease progression while reducing the need for costly or invasive tests.
Laboratory tests.
Laboratory studies may be helpful but are not specific for AS and must be considered only when significant clinical suspicion exists. HLA-B27, probably the most well-known laboratory finding associated with AS, may be found in patients with any of the seronegative spondyloarthropathies and in a small percent of unaffected patients (6% to 8%). The ESR also is nonspecific and may be increased in patients with any inflammatory or necrotic condition. Tests for rheumatoid factor and ANA are characteristically negative and are more useful for excluding seropositive disorders than diagnosing AS.
Treatment and management.
Treatment should focus on pain relief; a long-range plan to prevent, decrease, or delay joint and postural deformities; and preventing or reducing other associated complications (fractures). Patients with AS should be screened for osteoporosis; however, patient selection, time interval, and an optimal screening method are yet to be determined. 42 Osteoporosis of the spine may not be detectable with most current bone density measuring techniques because the ossification of the spinal ligaments produces a falsely elevated reading. 452 Patient education should stress safety, avoidance of fractures and spinal cord injury, and information about factors known to increase functional disability, such as smoking and lack of social support. 671 A rehabilitation and exercise regimen has been shown to slow the progression of functional disability671 and is necessary to maintain proper joint motion and function and promote proper posture by strengthening muscle groups that oppose the direction of the ensuing deformity. If joints are inflamed and painful, NSAIDs may be used to suppress pain, inflammation, and spasms in an effort to facilitate exercise. In the recent past, drug therapy has been fairly stagnant; however, the new tumor necrosis factor-alpha (TNF-α) antagonists appear not only to reduce signs and symptoms associated with AS, but also to reduce structural damage. 73,74,618
• Ankylosing spondylitis is the most common seronegative spondyloarthropathy.
• It primarily involves the synovial and cartilaginous joints of the axial skeleton.
• Males are predisposed to developing the condition (1:1 to 10:1), with the usual onset from 15 to 35 years of age.
• The radiographic findings are characterized by erosions, osseous proliferation, and bony ankylosis.
• Involvement is bilateral and symmetric and targeted to the spine, hips, shoulders, and particularly the sacroiliac joints.
• Ankylosing spondylitis causes sacroiliac erosions, joint widening, sclerosis, and fusion.
• It is associated with vertebral changes such as body squaring, Romanus lesions, shiny corner sign, syndesmophytes, and apophyseal fusion.
• Clinical characteristics are vague and include pain, limited range of motion, limited chest expansion, fever, fatigue, and weight loss.
• The condition causes decreased cervical and lumbar lordosis and increased thoracic kyphosis.
• Diagnosis is confirmed by radiographic appearance, negative test for rheumatoid factor, positive test for HLA-B27 antigen marker, and an elevated erythrocyte sedimentation rate.
• Treatment includes pain relief, with a long-range plan to decrease or delay joint and postural deformities.
Enteropathic Arthritis
BACKGROUND
Enteropathic arthritis, or arthropathy, is a disorder in which the articular alterations of the axial and appendicular skeleton are believed to be a direct pathogenic consequence of a group of bowel abnormalities, predominantly inflammatory bowel disorders. The condition is most frequently associated with ulcerative colitis and regional enteritis (Crohn’s disease), but Whipple disease; enteritis caused by Salmonella, Shigella, or Yersinia organisms; cirrhosis; hepatitis; pancreatic disease; and intestinal bypass surgery are all conditions that somehow can induce joint disease. The suspected mechanisms of the onset of arthritis include simultaneous joint and bowel infections or bowel infections that subsequently reach the joint (impaired barrier function), an immune response against a common bowel and joint antigen, and a genetic predisposition given the increased proportion of HLA-B27 in affected individuals as compared with unaffected individuals. 450
The underlying bowel disorder has an influence on which joints are affected and the percentage of involvement. The axial and appendicular skeletons may be separately or simultaneously involved. In general, peripheral arthritis is seen in approximately 15% to 20% of patients with inflammatory bowel disease, and it is most common in the lower extremities. It typically develops after the onset of bowel disease, and peripheral arthritic flares correlate with the underlying disease activity. 228 Axial involvement is noted in 3% to 18% of patients with inflammatory bowel disease. It may precede or follow the onset of bowel disease, and shows no strong association with disease activity. 228
In ulcerative colitis, peripheral arthritis occurs mostly in females and is noted in approximately 10% to 15% of patients, with the knees and elbow being the most common sites of involvement, respectively. Spondylitis occurs in 5% of ulcerative colitis patients, and they are predominantly male.
Peripheral arthritis is present in 15% to 20% and spondylitis in 5% of patients with Crohn’s disease. The cervical spine is the most common region of spinal involvement. There does not appear to be a particular gender association.
IMAGING FINDINGS
Radiographic alterations reflect the underlying inflammatory disease process, showing peripheral joint involvement similar to RA and axial changes identical to AS.
Axial skeleton.
Bilateral and symmetric SI erosions and sclerosis, joint space narrowing, and possible subsequent fusion occurs in combination with spinal changes or as isolated sacroiliitis in 4% to 18% of patients (Figs. 9-58 and 9-59). 228 The spondylitis that occurs in 3% to 6% of patients begins as a marginal vertebral body osteitis, progresses to the characteristic syndesmophytes that bridge adjacent vertebrae, and results in intersegmental fusion. (Please refer to the imaging section on AS for a more detailed description of the pathologic-radiographic changes that occur in the SI joints and the spine. As noted, these changes are identical.)
 |
| FIG. 9-58 Ulcerative colitis in a 49-year-old man presenting with evidence of bowel surgery (surgical clips and colostomy apparatus). The osseous changes of the sacroiliac joints result from associated enteropathic arthritis. Residual subdural contrast from a past myelogram is noted incidentally. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-59 Bilateral sacroiliitis occurring in a patient with ulcerative colitis. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Appendicular skeleton.
Initially the peripheral joint involvement associated with inflammatory bowel disease was thought to be RA caused by similar inflammatory episodes. However, enteropathic arthritis is usually nondestructive and asymmetric, consisting primarily of soft-tissue swelling and periarticular osteopenia. Osseous and cartilaginous destructive changes occur in rare cases. The arthropathy usually is self-limiting but tends to recur with a flare-up of the bowel disease. The most commonly affected joint is the knee, followed by the ankle, shoulder, wrist, elbow, and joints of the hands and feet, respectively. 47
CLINICAL COMMENTS
Not only do the radiographic features mimic AS, but so may the clinical manifestations (in a young patient with low back pain). Obviously patients may complain of symptoms associated with inflammatory bowel disease, such as abdominal pain, malaise, weight loss, diarrhea, or constipation. However, arthropathy can precede the onset of bowel disease symptoms or the actual disease itself. An ileocolonic study may be useful if inflammatory bowel disease is a possibility in a patient with unusual peripheral arthropathy or radiographic features consistent with AS. 363 Skin lesions and eye infections also can parallel the bowel condition or may precede them and be of diagnostic value. 507
Laboratory tests.
Laboratory test findings typically reflect those of other seronegative spondyloarthropathies. The percentage of positive HLA-B27 enteropathic arthritis patients as a whole is approximately 60%; however, this varies with the underlying gut abnormality and arthritic distribution. For example, the antigen is present in approximately 75% of patients with ulcerative colitis or Crohn’s disease who develop axial involvement but is not an associated genetic marker in patients with peripheral arthritis. 450 Tests for the rheumatoid factor typically are negative, and the ESR may be elevated.
Treatment and management.
Treatment involves control of the intestinal inflammation, which may incorporate the use of NSAIDs, and conservative management of the arthralgia. Surgical removal of the diseased portion of the colon can result in improvement of the peripheral arthropathy but does not seem to affect the progression of axial involvement. 105
Sacroiliitis is conventionally diagnosed with plain film radiography; however, the sensitivity to early joint change is low, and other imaging modalities may become more commonplace in the diagnosis and continued assessment of seronegative spondyloarthropathies. Imaging of sacroiliitis in the early or transient stage appears optimal with bone scan or MRI. 432 Detection of osseous erosions is best performed by HRCT, which also yields positive findings through “cold” or inactive periods when a bone scan may be negative. 432
• Enteropathic arthritis is a seronegative spondyloarthropathy associated with disorders of the gut and most commonly related to inflammatory bowel disease.
• The radiographic features of the axial skeleton mimic ankylosing spondylitis.
• The radiographic features of the appendicular skeleton mimic rheumatoid arthritis but typically are not erosive.
• Enteropathic arthritis has laboratory findings that are typical of other seronegative arthropathies.
Psoriatic Arthritis
BACKGROUND
Psoriatic arthritis is an inflammatory arthritide that may affect 0.1% of the general population, 591 and approximately 5% to 7% of patients with the skin disorder psoriasis, although in certain studies it has been reported at a substantially higher incidence in those with psoriasis (30% to 40%). 81,230,571 In the majority of patients, the onset of arthritis usually follows the onset of the skin disease; however, it may precede it or they may occur relatively simultaneously. 128,511 Articular involvement is more common in those individuals with moderate or severe dermatologic involvement. Although the etiology is unclear, the pathogenesis of both skin and joint disease is believed to be triggered by environmental factors in those with a genetic susceptibility, and mediated by the immune system. 34,127,128,485,663
The age of onset is usually between 30 and 50 years old; no significant gender bias is reported. 127,163 The main target areas are the distal joints of the hands and to a lesser degree the feet (2:1 hand-to-foot ratio). 529 Axial skeleton involvement occurs in up to half (and possibly more) of psoriatic arthritis patients. 37,163,325
Several classification systems for subtyping psoriatic arthritis have been proposed. 256,396,422 One of the most widely accepted is the system described by Moll and Wright that divides the arthritis into five basic patterns of disease, including polyarthritis, asymmetric oligoarthritis, spondylitis psoriatic arthritis, DIP involvement, and arthritis mutilans (a term describing advanced joint destruction and end-stage changes of rheumatoid and other arthritides). 443 These classifications are not clear cut; patients often demonstrate overlapping involvement, or may present with one subtype and progress into another over time.
IMAGING FINDINGS
In the past psoriatic arthritis has been thought of as having a relatively mild disease course when considering the arthritides as a whole. However, recent studies have shown that commonly severe joint damage may occur, and result in a deforming and debilitating disease. 216,529
The radiographic changes in the appendicular and axial skeleton are similar to those associated with RA and AS, respectively, although there are some distinct differences. In general, characteristic radiographic features include erosions, well-maintained bone density (unless during an acute attack when osteopenia can be seen), periarticular and shaft periostitis, osteolysis (including acroosteolysis), initial joint space widening with eventual joint space narrowing, and ankylosis. Joint involvement tends be asymmetric, although up to 50% of those with polyarticular involvement may have a symmetric presentation. 216 Patients with peripheral and axial arthritis have a tendency toward more frequent and severe joint lesions. 627
Hands and wrist.
The bone density usually remains normal (lack of periarticular osteoporosis); however, it may appear osteopenic during an acute attack. The joint spaces may appear unchanged, or may appear to be widened. Swelling and inflammation or tenosynovitis of the entire length of a finger (dactylitis) gives the characteristic appearance of “sausage” digit. Patients with psoriatic arthritis typically have asymmetric small joint involvement, with erosions initially and predominantly involving the DIP joints. Erosions may start at the bone margins, involving the bare area, and be fairly well defined, mimicking the appearance of RA. The erosions then become irregular and ill defined because of the subsequent fluffy periosteal new bone formation or whiskering, which produces a “mouse ears” appearance (FIG. 9-60FIG. 9-61 and FIG. 9-62). In severe cases the erosions may progress centrally, forming a “pencil-and-cup” or “cup-and-saucer” deformity (FIG. 9-63FIG. 9-64 and FIG. 9-65), so named because of the apparent expansion of bone at the distal articular surface and the sharpening of bone at the proximal articular surface. Acroosteolysis or tuftal resorption of the distal phalanx of the hands also may develop. 370 An advanced erosive course leads to the debilitating form of psoriatic arthritis known as arthritis mutilans (Fig. 9-66). The erosive and proliferative changes may be followed by intraarticular fusion (Fig. 9-67). 514
 |
| FIG. 9-60 The periarticular erosions of psoriatic arthritis (arrows) stimulate periostitis, appearing as fluffy bone growth adjacent the erosions (arrowheads). A to C, The appearance of the bone growth on either side of the phalanx has been likened to the ears of a mouse (mouse ear periostitis), seen here in three cases (arrowheads). Periostitis is not limited to periarticular area, but also may be found on the shaft of the bone. |
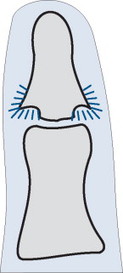 |
| FIG. 9-61 Bone proliferations from marginal periostitis result in a “mouse ear” configuration of the end of the bone. |
 |
| FIG. 9-62 Extensive erosions and disorganization of the distal interphalangeal joints in psoriatic arthropathy. Notice there is no appreciable osteopenia or involvement of the metacarpal phalangeal joints, features that are typical of rheumatoid arthritis, which facilitates differential diagnosis. (Courtesy Gary Longmuir, Phoenix, AZ.) |
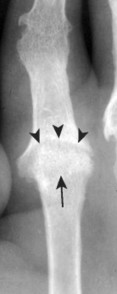 |
| FIG. 9-63 The second metacarpal head inserts into the large central erosion of the base of the adjacent proximal phalanx, forming a “pencil-and-cup” deformity, in which the pencil is noted by the arrow and the cup outlined by the arrowheads. In this case, and almost always, it looks more like a “cup and saucer.” This is the same patient as presented in Figure 9-74. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
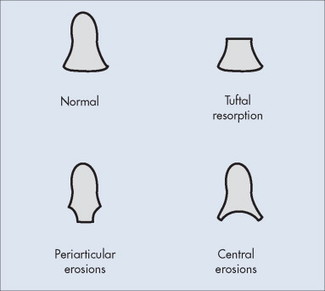 |
| FIG. 9-64 The distal phalanges of the hands provide an important clue to the presence and differentiation of inflammatory arthritides. Normally the distal phalanges appear with a slight spade shape. Abnormality of this shape may occur with distal, central, or periarticular erosions. |
 |
| FIG. 9-65 A, Psoriatic arthropathy appearing with asymmetric wrist and distal interphalangeal involvement. B, A close-up view exhibits the central erosions to better advantage (arrows). |
 |
| FIG. 9-66 Psoriatic arthritis of the hand resulting in severe erosions and misalignments, termed arthritis mutilans. Arthritis mutilans can be caused by other conditions, such as rheumatoid arthritis. |
 |
| FIG. 9-67 End stage psoriatic arthropathy may present with joint fusion. |
In addition to DIP involvement, the MCPs, PIPs, and carpus may develop erosions (Fig. 9-68). If all joints of a single digit are affected, the pattern formed is called a ray pattern. Joint deformities and subluxations similar to those of RA may occur, such as ulnar deviation of the metacarpals and boutonnière and swan neck deformities, but are not as common. If severe erosive disease occurs at multiple joints, one phalanx may “slide” onto another or onto the metacarpal. The overlying excess skin develops overlapping folds and is called an opera glass hand. Wrist abnormalities usually follow DIP involvement and may occur within any compartment.
 |
| FIG. 9-68 A characteristic feature of psoriatic arthritis is its propensity to involve all of the joints in one digit, as opposed to a type of joint in all digits. This tendency toward a digit pattern is termed ray pattern, in which ray is a zoological term for finger. A, The tendency to distribute more pronounced changes in one finger leads to noticeable soft-tissue swelling more in one finger, known as a sausage digit finger. B, The ray pattern tendency of psoriatic arthropathy is in contrast to the metacarpophalangeal involvement of rheumatoid. The ray pattern may present in any digit, not just the second. |
Feet.
Changes in the feet caused by psoriatic arthritis are similar to changes in the hand, although the feet are affected less often. The bone density usually remains normal, without evidence of significant osteoporosis. Dactylitis occurs, leading to the appearance of “sausage” digits. Joint erosions and osseous proliferation commonly take place at the IP joint of the great toe and the DIP articulations of all digits (Fig. 9-69). Tuftal resorption may occur. An “ivory” phalanx may result from exuberant periosteal and endosteal proliferation and sclerosis or the terminal phalanx, and has a predilection for the terminal phalanx of the first digit. This is an uncommon presentation, but one that is unique and specific for psoriatic arthritis; it is of diagnostic importance if tuft resorption and articular abnormalities are absent. 548
 |
| FIG. 9-69 Significantly affected metatarsophalangeal joints with fusion of multiple joints. |
Erosive and subsequent proliferative changes may take place at the calcaneal entheses (enthesitis), leading to findings similar to those associated with other seronegative spondyloarthropathies, particularly Reiter’s disease.
Sacroiliac joints.
It has been reported that 30% to 50% of psoriatic arthritis patients develop SI involvement (Fig. 9-70), 230,248 but a more recent study noted sacroiliitis at a substantially higher incidence of 78%. 37 The sacroiliitis occurring in patients with psoriatic arthritis mimics those changes noted in AS patients. Erosions, joint space widening, sclerosis, and possible fusion typically are bilateral and symmetric; however, other distributions are seen and the bilateral symmetric distribution is less frequently seen with psoriatic arthropathy than with AS. Proliferative enthosopathic changes may be noted in the pelvis, predominantly affecting the ischium and iliac crests.
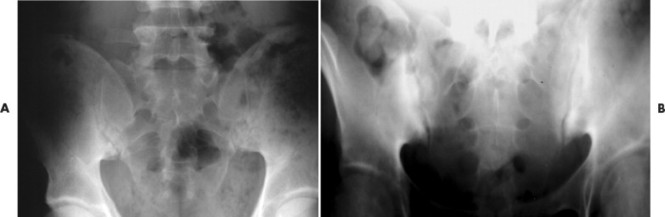 |
| FIG. 9-70 A and B, Bilateral asymmetric sacroiliitis in different patients with psoriatic arthropathy. |
Spine.
Spinal involvement usually but not always is associated with sacroiliitis. Erosions occur on the surface of the vertebrae, with subsequent ossification at the paramarginal site of erosion or in the adjacent soft tissue. In contrast to patients with AS, the spinal lesions or syndesmophytes associated with psoriatic arthritis are typically bulky, asymmetric, and nonmarginal ossifications that do not appear in consecutive vertebrae (“skip” lesions). These “skip” lesions develop most commonly at the lateral aspects of the vertebral bodies in the thoracolumbar junction (Fig. 9-71). 514 Radiographic changes in the cervical spine in patients with psoriatic arthritis have been reported to be 36% to 70% (Fig. 9-72). 292,569 Atlantoaxial subluxations and apophyseal involvement (joint space narrowing, sclerosis, possibly ankylosis) may occur, but these findings are not nearly as common as those noted in patients with AS.
 |
| FIG. 9-71 Psoriatic arthropathy. Thick, bulky syndesmophyte formation (arrows) is noted along the lateral margins of the lumbar vertebra. Uncharacteristically these syndesmophytes appear continuous on the reading right side. Usually they skip segments. The appearance of this case would be impossible to separate from Reiter’s syndrome without clinical data or other imaging, diffuse idiopathic skeletal hyperostosis, or an atypical presentation of degeneration. (Courtesy Trevor Ireland, Anchorage, AK.) |
 |
| FIG. 9-72 The posterior joint margins are sclerotic and ill defined, consistent with involvement in this psoriatic arthropathy (arrowheads). In addition, although the region is underexposed, the atlantodental interval appears suspicious for enlargement (arrow), which is also suggested by the anterior offset of the spinal laminal lines of C1 on C2. |
Radiologic differentiation between the spondylitis caused by psoriatic arthritis and the spondylitis caused by Reiter’s syndrome is impossible, although the latter may be less severe. 492
CLINICAL COMMENTS
The majority of patients who present with joint pain as a result of psoriatic arthritis are aware of the psoriasis; however, some are not. They may have a single, hidden lesion and not realize they have any skin condition, or on presentation of their clinical history patients may fail to mention the skin disorder after it has cleared, assuming it is not related to their joint pain. Therefore if psoriatic arthritis is a diagnostic consideration, a prudent cutaneous search is needed, and the patient’s dermatologic history should be directly questioned. Although the onset of arthritis usually follows the development of the skin lesions; up to 20% of patients develop arthritis before psoriasis, and the condition may present simultaneously in approximately 16%. 571
Low back, hand, and foot pain may be the initial presenting complaints. Joint symptoms are similar to those of a patient with RA and may consist of pain and stiffness (especially in the morning), soft-tissue swelling, and limited range of motion. Physical examination of patients with psoriatic arthritis may reveal skin lesions, soft-tissue swelling of an entire digit (“sausage” digit), 100 and nail lesions (pitting, ridging, and onycholysis), the latter of which seems to best correlate with the arthritis. Nail changes have been noted in 63% to 86% of patients with psoriatic arthritis, and in 37% of patients with psoriasis without arthritis. 163,354,571
Laboratory tests.
Laboratory tests usually reveal an increased sedimentation rate, are negative for rheumatoid factor, and possibly are positive for HLA-B27 (in 25% to 60% of patients). 77
Treatment and management.
Baseline PA radiographs of the hands, wrists, and feet, and radiographs of the spine and other symptomatic regions should be obtained. Serial radiographs then should be taken at 6-month intervals for the first 2 years after disease onset, depending on treatment regimen. 473
Treatment is directed at controlling the joint inflammation and is dependent on the severity of joint involvement. Antiinflammatory agents such as NSAIDs may yield clinical improvement of joint pain, but they may exacerbate skin lesions, 520 and joint damage may continue to progress. 217,241 In these cases disease-modifying antirheumatic drugs (DMARDs), including methotrexate or cyclosporine, may be effective. Cyclosporine in low doses has been used because it aids in treating both skin and joint conditions. 563 High doses of vitamin D also may be beneficial. 270 Recently the Food and Drug Administration (FDA) approved etanercept for the treatment of psoriatic arthritis. This is the first FDA-approved treatment for psoriatic arthritis. 173,424,425 Etanercept is a biologic agent that has been used for the treatment of RA. It is designed to target specific mediators involved in the pathogenesis of psoriatic arthritis.
• Psoriatic arthritis is a seronegative spondyloarthropathy that develops in 5% to 7% of patients with psoriasis.
• The age of onset is between 30 and 50 years of age and does not develop more often in a particular gender.
• The changes in the axial skeleton mimic the changes in patients with ankylosing spondylitis, but often patients may have unilateral or asymmetric sacroiliac involvement.
• Syndesmophyte formation may be thick and asymmetric with “skip” lesions.
• The effects on the hands are similar to those caused by rheumatoid arthritis; however, the distal interphalangeal joints usually are affected first. Erosions may become central and more severe, and periostitis is a prominent feature.
• Physical examination may reveal nail pitting, skin lesions, and soft-tissue swelling of an entire digit.
Reiter’s Syndrome
BACKGROUND
Reiter’s syndrome, a seronegative spondyloarthropathy, is an asymmetric polyarthritis that targets the large joints of the lower extremities, small joints of the feet, and axial skeleton. Incidence is estimated at 3 to 4 per 100,000, but values vary widely. Reiter’s syndrome is commonly associated with eye disorders, skin rashes, and mouth sores. A minority of patients have the classic triad of symptoms (arthritis, urethritis, and conjunctivitis) that originally characterized the syndrome introduced by Hans Reiter’s in 1916. 508
Reiter’s syndrome is considered a form of reactive arthritis, a term often used as a synonym. It is precipitated by a bacterial infection that initially involves mucosal surface. It is an aseptic or sterile, likely immune-mediated, inflammatory process that occurs distant to the primary focus of infection, which is generally in the genitourinary or gastrointestinal tract. 315 Its etiology appears to be linked to genetic factor(s), given the high incidence of HLA-B27 (80%), and to infection, given the frequent occurrence after an infectious episode. 315,528 Most cases follow genitourinary infections with Chlamydia trachomatis, although it may follow enteric infections with some strains of Shigella, Yersinia, and Salmonella. Males are affected five times more frequently than females, with the average age of onset from 15 to 35 years. 180
IMAGING FINDINGS
Reiter’s syndrome has a predilection for the lower extremities and is asymmetric in distribution. As with all of the seronegative spondyloarthropathies it is associated with sacroiliitis and spondylitis. The changes associated with Reiter’s syndrome may be radiographically indistinguishable from those of psoriatic arthritis. However, the propensity for patients with Reiter’s syndrome to have lower extremity involvement and patients with psoriatic arthritis to have upper extremity involvement is helpful. Differential diagnosis also may be accomplished through clinical distinction, not purely radiologic appearance: 197,316 for example, the presence of balanitis circinata and keratoderma blennorrhagica in patients with Reiter’s syndrome or presence of nail pitting and psoriasis in patients with psoriatic arthritis.
Feet.
The feet are the most commonly involved site of Reiter’s syndrome, with the calcaneus, MTP, and IP articulations of the first digit being specifically affected. Calcaneal erosion followed by fluffy periosteal new bone occurs at the insertion of the plantar fascia and Achilles tendon (enthesitis) (FIG. 9-73FIG. 9-74FIG. 9-75 and FIG. 9-76). 596 These inflammatory heel spurs are typically bilateral, present in approximately 59% of patients, and are highly suggestive of Reiter’s syndrome. 594 The erosive changes involving the MTPs are similar to those that occur in patients with RA. Lanois deformity is a term for resultant joint subluxations and deformities at the MTPs, often specifically defined as dorsal subluxation of the MTP joints and fibular deviation of the toes. In addition, these patients have periostitis, “sausage” digits, and relatively little osteopenia, findings that are similar to those of psoriatic arthritis (Figs. 9-77 and 9-78), although osteopenia may be present during acute attacks.
 |
| FIG. 9-73 Reiter’s syndrome. A, The normal calcaneus exhibits a thin uninterrupted cortical margin (arrows). B, The cortex is interrupted by three small erosions (arrows). The posterior superior margin of the calcaneus is a targeted site of involvement for Reiter’s syndrome. (Courtesy Arthur Holmes, Foley, AL.) |
 |
| FIG. 9-74 Reiter’s syndrome. A and B, Bilateral erosions at the insertion of the calcaneal tendon (arrows). (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-75 Reiter’s syndrome. A, Left and, B, right calcaneus exhibit extensive erosions at the attachment site of the calcaneal tendon (arrows) and plantar fascia (arrowheads) in this patient with Reiter’s syndrome. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-76 Erosive changes and multiple subluxations affecting predominantly the metatarsophalangeal articulations. Mild periostitis can be seen along the medial aspect of the tarsals (arrow). Bone density is usually relatively well preserved in Reiter’s syndrome; however, in this patient, pain has caused disuse and resulting osteoporosis. |
 |
| FIG. 9-77 Although the foot is more commonly involved, Reiter’s syndrome can exactly mimic psoriatic disease. In this case there is distal tuft resorption (arrowhead) and sclerosis of the distal phalanx (arrow). These features are more typical of psoriatic arthropathy. Because of the commonality in presentation, definitive differentiation of psoriatic arthropathy and Reiter’s syndrome is done via clinical data, not radiographic presentation. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
 |
| FIG. 9-78 Periarticular erosions and reduced joint space of the distal interphalangeal joints in a patient with Reiter’s syndrome. Although it is not uncommon to see involvement of the distal interphalangeal joints in Reiter’s syndrome, a presentation like the one seen here is more typical of primary degeneration or psoriatic arthropathy. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Tendons.
Tenosynovitis is striking in patients with Reiter’s syndrome, particularly in the tendons of the feet (Achilles). MRI is useful to demonstrate the distended tendon sheath.
Large joints of lower extremities.
The knee and ankle are frequently affected in patients with Reiter’s syndrome, whereas the hip is rarely affected. The radiographic findings are consistent with other inflammatory arthritides: soft-tissue swelling, joint effusion, loss of joint space, and erosions. In addition, mild bony productive changes usually are seen, and osteopenia typically does not develop. Severe joint destruction is uncommon. 399,594 Enthesitis may involve the tibial tubercle at the insertion of the patella tendon.
Sacroiliac joints.
Sacroiliitis may be bilateral and symmetric, bilateral and asymmetric, or unilateral (Fig. 9-79). The joint changes mirror those of the other seronegative spondyloarthropathies. Subchondral erosions, adjacent sclerosis, and joint space widening are noted. Progression to complete joint fusion in patients with Reiter’s syndrome is much less common than in patients with AS. 594 With chronic disease, more than 50% of Reiter’s patients eventually develop sacroiliitis; in the early stages fewer than 10% demonstrate SI involvement.
 |
| FIG. 9-79 A, Reiter’s syndrome appearing with asymmetric bilateral sacroiliitis (arrows) and, B, a single thick syndesmophyte (arrowheads). (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Spine.
The spine is involved less frequently in patients with Reiter’s syndrome compared with patients with AS or psoriatic arthritis. The thoracolumbar junction is the most common spinal site affected. 508 Thick, nonmarginal syndesmophytes, identical to those associated with psoriatic arthritis, bridge the spine and commonly skip segments (Fig. 9-80).
 |
| FIG. 9-80 Close-up view of a paravertebral ossification (arrowheads) characteristic of the spinal changes associated with Reiter’s syndrome, or psoriatic arthritis. This patient is the same as the patient whose calcaneus is presented in Figure 9-73 and is a different patient than presented in Figure 9-79; note how typical these thick syndesmophytes can be. (Courtesy Arthur Holmes, Foley, AL.) |
If associated arthritic changes occur in the cervical spine (Figs. 9-71 and 9-72), they are less common and less severe than in patients with psoriatic arthritis.
CLINICAL COMMENTS
Reiter’s syndrome presents most commonly as a polyarthritis in young men, and therefore should be a diagnostic consideration in any young man presenting with asymmetric oligoarticular polyarthritis. It typically develops within days or weeks after genitourinary infection or dysentery. The patient generally experiences lower extremity polyarthritis for at least 1 month in addition to one or more of the following: urethritis; conjunctivitis (less commonly uveitis); mucocutaneous lesions; nail changes; dysentery; heel pain; low b ack pain; or radiographic signs of sacroiliitis, periostitis, or heel spurs. Nonspecific cervicitis may occur in female patients. Patients also may present with a fever and significant weight loss. The initial disorder usually is self-limiting, but most patients have recurrent episodes of active arthritis. 528
Reiter’s syndrome may produce two characteristic cutaneous lesions. Balanitis circinata is present in about 25% of post–Shigella- and post–Chlamydia-infected patients and is characterized by small, painless ulcers on the glans penis and urethral meatus. Keratoderma blennorrhagica, which develops in 12% to 14% of patients, is characterized by hyperkeratotic skin lesions that usually are on the plantar surface of the feet, toes, penis, and trunk. Painless oral ulcers may be present as well.
Reiter’s syndrome may occur in human immunodeficiency virus (HIV)–infected patients, and sometimes is the initial manifestation of the disease. 688 This should be considered if the etiology of reactive arthritis is unknown.
Laboratory tests.
Laboratory findings are consistent with the other seronegative spondyloarthropathies. There is an increase in the erythrocyte sedimentation (SED) rate, rheumatoid factor is negative, and HLA-B27 is positive in approximately 75%.
Treatment and management.
Tetracycline or erythromycin is the usual treatment for sexually transmitted chlamydial infections. Until recently, similar antibiotic therapy for the treatment of Reiter’s syndrome was unsuccessful; 528 however, more current studies have yielded favorable results. 32,33,352,485 It has been suggested that prophylactic antibiotics eventually may benefit individuals who are at risk for developing Reiter’s syndrome. 33 At the onset, arthritic flare-ups usually respond to NSAIDs. Oral corticosteroids do not appear to be as effective. Intraarticular steroid injections may be necessary if the arthralgia is severe, especially in patients with large knee effusions.
• Reiter’s syndrome is a seronegative spondyloarthropathy that predominantly affects the large joints of the lower extremities and small joints of the feet.
• Five times more men than women develop the syndrome. The average age of onset is between 15 and 35 years.
• The radiographic changes of the axial skeleton (sacroiliitis and spondylitis) may be identical to the changes seen in psoriatic arthritis.
• Inflammatory changes in the feet are similar to a combination of those associated with rheumatoid and psoriatic arthritis.
• Calcaneal enthesopathies (erosive and proliferative) are characteristic.
• Only a minority of patients develop the classic triad of arthritis, urethritis, and conjunctivitis that is associated with Reiter’s syndrome.
• It is associated with nongonococcal genitourinary and enteric bacterial infections.
Crystal-Induced Arthritides
Gouty Arthritis
BACKGROUND
Gout is the most common cause of inflammatory arthritis in men over 40 years old. It is a clinical disorder associated with elevated serum urate levels. Uric acid is the normal by-product of purine metabolism that is filtered and excreted by the kidneys. Hyperuricemia develops if overproduction of uric acid or underexcretion by the kidneys occurs. The excess urate crystallizes as monosodium salt, and is deposited into various connective tissues, including the articular and periarticular structures. When crystalline monosodium urate is deposited in the joint, an inflammatory response occurs, resulting in acute pain and swelling (gouty arthritis). These acute episodes are followed by asymptomatic periods. Chronic gout may result after approximately 10 years of recurrent intermittent acute attacks. A minority of patients (about 20%) with hyperuricemia develop gout. Its development is multifactorial; although hyperuricemia is requisite, it is not the sole determinant.
Gout is classified into two forms based on etiology: (a) an idiopathic or primary form that has no known underlying disorder, and is believed to result from an inborn error of purine metabolism, and (b) a much less common secondary form associated with an acquired disorder that is enzymatic, hereditary, hematologic, endocrine, renal, or associated with amyloidosis, multiple myeloma, or chemotherapy. 66 The first gouty attack of the idiopathic form occurs among individuals 40 to 50 years old; it is 20 times more common in men than women. 225 Women who develop gout generally are postmenopausal; only 17% are premenopausal.
Four phases of idiopathic gout are recognized:
1. Asymptomatic gout. The first phase is hyperuricemia, which may not lead to gout. Patients experiencing their first attack of acute gout have had sustained hyperuricemia for 20 to 30 years.
2. Acute gouty arthritis. The second phase involves acute inflammatory arthritis, which is classically monoarticular and usually involves the first MTP joint of the first toe, although oligoarticular or polyarticular involvement may occur. The ankle, tarsals, and knee also are commonly involved. Early attacks tend to subside without treatment in 7 to 10 days.
3. Intercritical gout. The third phase is the period between acute attacks. This stage may last for months or years, but tends to shorten with recurring episodes.
4. Chronic tophaceous gout. The fourth, or chronic, tophaceous gout phase is marked by the development of radiographically evident gross deposits of urate crystal or tophi in the subcutaneous tissues, synovium, subchondral bone, articular cartilage, joint capsule, and periarticular tissues such as the tendons (calcaneal), ligaments, and bursae (olecranon and prepatellar), and the classic extraarticular location, the helix of the ear. Often patients in the chronic phase of gout may not exhibit tophi for 10 to 12 years after the onset of joint pain.
IMAGING FINDINGS
Acute.
It is difficult for plain film to detect the early phases of gout, as the radiographic findings in the acute phase are nonspecific, presenting as soft-tissue swelling from capsular distention and adjacent soft-tissue edema, and not always easily recognized radiographically. In addition, these initial changes subside when the attacks remiss.
Chronic.
Chronic gout is well demonstrated on plain film with eccentric well-marginated osseous erosions that have overhanging edges of bone, central sclerotic erosions that may appear cystic, and soft-tissue deposits or tophi in and around the joint. These tophaceous deposits are the underlying mechanism for the radiographic appearance. The deposits appear as dense lobulated soft-tissue masses and may contain calcification. They are asymmetric in distribution, and may cause bone erosions that are intraarticular, paraarticular, or located some distance from the joint. The tophi are directly deposited into the bone, or nestle into the bone via mechanical erosion. In the latter case, a thin “overhanging edge” of bone with a sclerotic margin is left above and below the tophaceous deposit (Figs. 9-81 and 9-82). Even in chronic gout, bone density usually remains normal. Osteoporosis is not characteristic of gout, unless severe pain causes disuse atrophy. Joint spaces usually are preserved until late in the disease, irrespective of adjacent large erosions. Bony ankylosis is not a feature; however, fibrous ankylosis may occur as a late manifestation of the disease.
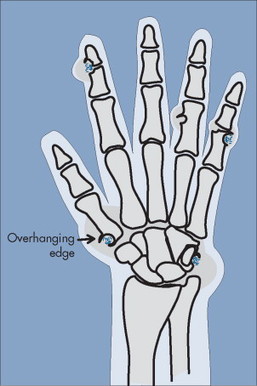 |
| FIG. 9-81 Intraarticular or extraarticular deposits of gouty tophi cause mechanical erosion of the underlying bone. The mechanical nature of the erosion is marked by a sclerotic rim of cater, a feature not seen in inflammatory erosion of rheumatoid arthritis. At times the elevated margin of the erosion caused by the gouty tophus forms a shelf of bone that extends partially around the tophus. The shelf of bone is known as an overhanging edge. |
 |
| FIG. 9-82 Overhanging edge (arrow) partially extending around a gouty tophus of the fourth digit and two small but similar features present with the fifth digit (crossed arrows). |
Lower extremities.
Gout tends to affect the peripheral joints of the lower the extremities, particularly the feet. The MTP articulation of the first toe is the most common initial site of gouty arthritis and when present in this location is called podagra (Fig. 9-83). Ninety percent of patients exhibit changes in this articulation during the course of the disease. Erosions of the first metatarsal head are most pronounced on the dorsal and medial aspects. There is associated soft-tissue swelling, and possibly a resultant valgus deformity. Soft-tissue swelling from tophaceous deposits and erosions may occur over the dorsum of the foot as a result of involvement of the tarsometatarsal, intertarsal, and talocalcaneal articulations. Tophi in the Achilles tendon and the adjacent structures are common.
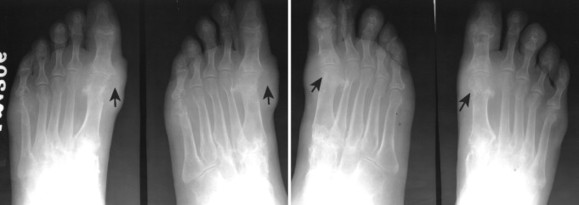 |
| FIG. 9-83 Posteroanterior and oblique projections of both feet in a patient with gout. Gout is predisposed to the first metatarsophalangeal joint. Sometimes gout is called podagra at this site. As is typical, the erosions in this case are more pronounced on the medial and dorsal aspects of the joint (arrows). However, the symmetry noted in this case is not a consistent feature of the disease. (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Erosions may occur on the medial and lateral aspects of the knee, without visible joint space narrowing. Intraarticular tophaceous deposits in the knee may cause pain and swelling. MRI can be used to confirm their presence. 110 Erosive changes may involve the patella, and tophi may lead to inflammation of the prepatellar bursa.
Upper extremities.
Gout has a predilection toward the peripheral joints when the upper extremities are involved. Asymmetric joint changes may be noted in the wrists and hands, particularly involving the carpometacarpal joints, but the DIP, PIP, and to a lesser extent MCP articulations also may be affected (Figs. 9-84 and 9-85). Soft-tissue masses usually are located on the dorsum of the hand and wrist. Soft-tissue swelling, cystic defects, and joint destruction may be present in the wrist. Scapolunate dissociation also may occur. 530
 |
| FIG. 9-84 Gout. The fingers appear with large destructive regions of bone on overlying soft-tissue masses. |
 |
| FIG. 9-85 Gout in one digit. A, The oblique hand reveals a small region of increased radiodensity of the proximal interphalangeal joint of the fifth digit. B, The large dorsal soft tissue mass is noted on the lateral view of the finger (arrows). |
Large tophaceous deposits often are seen near the olecranon process of the elbow (Fig. 9-86). Adjacent bursal involvement may be bilateral, and presents as soft-tissue swelling over the extensor surface of the elbow.
 |
| FIG. 9-86 Large soft-tissue mass of gout tophi near the olecranon process of the elbow (arrows). (Courtesy Steven P. Brownstein, MD, Springfield, NJ.) |
Axial skeleton.
Spinal involvement in gout is rare. SI involvement has been reported more commonly than spinal involvement, but is still considered infrequent.
CLINICAL COMMENTS
Acute gouty attacks present as joint pain, swelling, and erythema (Fig. 9-87). The presentation is usually monoarticular, although several joints may be involved. The presentation mimics cellulitis. The MTP of the great toe is the most commonly involved joint. Attacks are self-limiting, and usually subside within 3 to 10 days. The diagnosis often is presumed based on a classic presentation, but a definitive diagnosis for gouty arthritis depends on confirming the presence of monosodium urate crystals in the synovial fluid or tophi. Fluid samples are ordinarily drawn from the first MTP joint.
 |
| FIG. 9-87 Middle-aged male patient with large subcutaneous masses representing the clinical presentation of tophaceous gout in, A, the elbow and, B and C, both hands. (Courtesy Ian D. McLean, LeClaire, IA.) |
The kidneys are the most common extraarticular organ to be affected by gout. Urate nephropathy is an inflammation secondary to chronic hyperuricemia. Renal stones (uric acid nephrolithiasis) may occur in patients with long-standing gout.
Hyperuricemia is defined as serum urate concentrations of more than 7 mg/dl in men and 6 mg/dl in women. Serum urate levels alone cannot be used to definitively diagnose gout because they may be high or low and therefore are often misleading. A normal level does not exclude the diagnosis of gout. However, serial uric acid measurements are useful in following the disease progression and treatment response.
Treatment and management.
After diagnosis, the treatment objective is twofold. It is directed toward pain relief, consequent restoration of normal joint function, and the prevention of crystal accumulation within the joint that can lead to destruction and secondary degenerative disease. Any osseous changes noted radiographically usually are permanent, although minor improvement may be noted. Of course a search must be made for a possible underlying disorder (secondary gout) that may be treated directly. Acute pain and swelling usually responds well to the administration of NSAIDs, corticosteroids, and colchicine. Prophylactic use of NSAIDs and colchicine may be used in patients with severe, multiple, recurrent arthralgia. Patients should also be aware of factors that may contribute to or trigger the onset of an attack, such as alcohol or drug use, obesity, and high purine diets (e.g., all meats and seafood, meat extracts and gravies, yeast and yeast extracts, alcoholic beverages, beans). Low purine foods include pasta, flour, bread, milk, eggs, and fruits.
• Gout is a clinical disorder resulting in monosodium urate crystal deposition into a variety of tissues, including the joints.
• Four gout phases are recognized: asymptomatic gout, acute arthritic gout, intercritical gout, and chronic tophaceous gout.
• The peripheral joints of the lower extremities are most commonly affected, and the first metatarsophalangeal joint is eventually affected in 90% of gout patients. This classic presentation is known as podagra.
• Early-stage radiographic features of gout are difficult to evaluate radiographically because they predominate as soft-tissue swelling resulting from capsular distention.
• Late-stage radiographic features of gout include randomly scattered eccentric nodular soft-tissue prominences or tophi that may contain calcium, and that have a predilection for the dorsum of the feet and hands and the extensor surfaces of the extremities; preservation of the joint space until very late stage; lack of osteoporosis; and intraarticular or periarticular bony erosions with a sclerotic well-defined “overhanging edge” whose formation is secondary to adjacent tophaceous deposits.
Calcium Pyrophosphate Dihydrate Crystals
BACKGROUND
The deposition of calcium pyrophosphate dihydrate (CPPD) crystals in and around joints results in an arthropathy with protean manifestations. The nomenclature relating to this process and disease is often confusing and incorrectly used. For the purposes of simplification, the text focuses on the following three major presentations of the calcium pyrophosphate deposition disease:
1. Chondrocalcinosis. The classic presentation of CPPD is radiographic evidence of calcified articular cartilage (chondrocalcinosis) involving characteristic sites, which include the knee, wrist, MCPs, and symphysis pubis. Less commonly, crystals also may be deposited and radiographically visible in the synovium, joint capsules, tendons, and ligaments. 499 The term chondrocalcinosis often is used incorrectly as a synonym for CPPD. Although calcium pyrophosphate is the most common crystal to cause chondrocalcinosis, 549 the terms CPPD and chondrocalcinosis are not truly interchangeable because crystals other than calcium pyrophosphates can be deposited in and around joints and lead to visible calcification; in addition, factors other than crystal deposition can lead to chondrocalcinosis or cartilage calcification (degeneration).
2. Pyrophosphate arthropathy. The intraarticular deposition of crystals may degrade the cartilage and lead to a second manifestation of CPPD that radiographically mimics severe joint degeneration, a condition called pyrophosphate arthropathy. The radiographic image is difficult to distinguish from primary OA or secondary OA after trauma; however, the location of joint involvement is helpful. Pyrophosphate arthropathy typically develops in an articulation or compartment that is unusual for primary OA, and there is lack of documented history of trauma that indicates secondary OA.
3. Pseudogout. The clinical presentation of CPPD varies; a patient can be completely asymptomatic or may present with an acute, painful, and inflamed joint that is similar to those associated with gout. The latter presentation has been appropriately called pseudogout.
The underlying cause of this CPPD is unknown, but its frequent association with other conditions such as gout, hyperparathyroidism, hemochromatosis, diabetes mellitus, and neurotrophic osteoarthropathy suggests that it may be secondary to metabolic or degenerative changes in the cartilage. It also has been proposed that the simultaneous occurrence of pseudogout and the aforementioned conditions is purely coincidental.
It is generally accepted that the prevalence of chondrocalcinosis increases with age, and that no particular gender develops the condition more often. 164,187,682 One study suggests that this increased prevalence with age and lack of gender bias may correlate with the affected tissues. 691 The study, which focused on structures of the knee, concluded that the prevalence of hyaline cartilage calcification increases with age and is not gender related, whereas meniscal calcification is not age related and is significantly more prevalent in men.
IMAGING FINDINGS
General radiographic features of CPPD can consist of a characteristic solitary finding such as chondrocalcinosis or a combination of features, which may include other intraarticular and periarticular calcifications, soft-tissue swelling, and progressive structural joint damage such as secondary degenerative joint disease (DJD) or mimic a neurotrophic arthropathy if severe.
Chondrocalcinosis.
Cartilage calcification may involve hyaline or fibrocartilage (FIG. 9-88FIG. 9-89FIG. 9-90FIG. 9-91FIG. 9-92 and FIG. 9-93). Fibrocartilage calcification is most common in the menisci of the knees, triangular cartilage complex of the wrist, symphysis pubis, and acetabular labrum. The calcification presents radiographically as a thick, irregular radiopaque focus within the affected structure. Hyaline cartilage calcification also is common in the knee, wrist, hip, MCPs, elbows, and shoulders. On a radiograph it appears as a thin, linear radiopacity that runs adjacent and parallel to the articular surface of the bone.
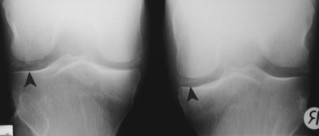 |
| FIG. 9-88 Calcium pyrophosphate dihydrate presenting with chondrocalcinosis in the menisci bilaterally (arrowheads). |
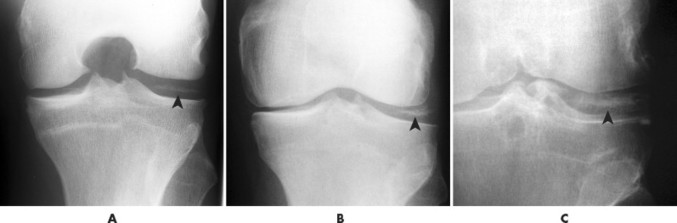 |
| FIG. 9-89 A to C, Calcium pyrophosphate dihydrate meniscal chondrocalcinosis of the knee in multiple patients (arrowhead). |
 |
| FIG. 9-90 Chondrocalcinosis of the articular cartilage of the femur (arrow). |
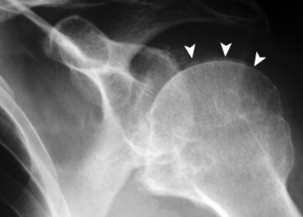 |
| FIG. 9-91 Calcification of the articular cartilage of the humerus (arrowheads) in a patient with calcium pyrophosphate dihydrate chondrocalcinosis. |
 |
| FIG. 9-92 A and B, Chondrocalcinosis manifests in both hyaline (articular) (arrows) and fibrocartilage (arrowheads). In the wrist, C, chondrocalcinosis of the hyaline cartilage appears as a double shadow of the carpal bones, and, D, chondrocalcinosis of the fibrocartilage presents as a wedge of calcification in the triangular fibrocartilage complex (arrows). E, Condrocalcinosis of the hyaline cartilage appears as a thin radiodense line that parallels the articular cortices of the involved bone (blue lines), and chondrocalcinosis of the fibrocartilage appears as a radiodense finding within the joint space (blue triangle). |
 |
| FIG. 9-93 Chondrocalcinosis of the triangular fibrocartilage complex (arrow) and faintly seen involvement of the hyaline cartilage (arrowheads). |
Pyrophosphate arthropathy.
Chronic pyrophosphate crystal deposition within hyaline cartilage may lead to intraarticular damage that radiographically simulate DJD. However, the joint location is unusual, or has an unusual intraarticular distribution when compared to DJD. These changes tend to be progressive and severe, with advanced joint space narrowing, prominent bony proliferation (sclerosis and osteophytosis), and often dramatic cyst formation. The articular and intraarticular (or compartmental) distribution classically differs from that of primary OA and should aid in the diagnosis. Non–weight-bearing joints such as the shoulder, elbow, wrist, and patellofemoral joint compartment are involved, as well as weight-bearing articulations such as the knee and hip. In a patient with no history of trauma, a DJD pattern in the mentioned non–weight-bearing joints suggests pyrophosphate arthropathy. Isolated involvement of the patellofemoral compartment (Fig. 9-94), advanced tricompartmental disease of the knee, and selective radiocarpal or trapezioscaphoid joint degeneration also are unusual for nontraumatic DJD and suggest that an underlying crystal deposition is responsible for the radiographic findings.
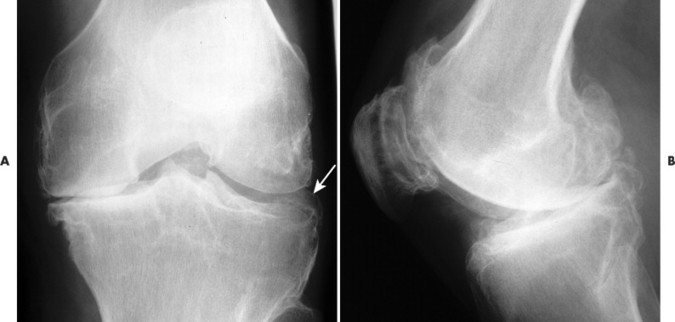 |
| FIG. 9-94 Pyrophosphate arthropathy. A, Anteroposterior and, B, lateral knee radiographs revealing characteristic features of pyrophosphate arthropathy. Advanced femoropatellar compartment degenerative changes are present; the medial and lateral compartments of the knee are relatively spared. Meniscal calcification also is apparent (arrow). Primary osteoarthritis has an affinity for the medial femorotibial compartment and tends to spare the lateral and retropatellar compartments. |
CLINICAL COMMENTS
The varied clinical presentations of CPPD can cause a diagnostic dilemma. CPPD may masquerade as primary DJD (chronic progressive joint pain, crepitus, and limited range of motion), manifest as an acute inflammatory disorder such as RA or gout (with intermittent attacks of painful, red, swollen joints), or appear as an asymptomatic condition in a patient with a concomitant disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree