9 Future of Lung Cancer Screening
Summary
This chapter explores several diverse factors that may potentially predispose different populations to an increased risk of lung cancer including genetic predisposition, dietary habits, cultural beliefs, and environmental exposures. Disparate variations in the detection, diagnosis, staging, and treatment of lung cancer among various ethnic groups and races are also reviewed. The role of various exhaled and serum biomarkers in the early detection, staging, and stratification of lung cancer patients is also discussed and they are likely to have a more prevalent role in the near future to both help identify high-risk populations and minimize false-positive screening rates. Lastly, this chapter reviews various clinical risk assessment models including the Bach, Spitz, LLP (Liverpool Lung Project), and PLCO (Prostate, Lung, Colorectal, and Ovarian) models and demonstrates the application of the Brock University risk calculator.
Keywords: racial disparity, ethnic disparity, epidermal growth factor receptor mutations, oncogenic driver mutation, MicroRNAs, COSMOS, C-reactive protein, prolactin, hepatocyte growth factor, cancer-testis antigen NY-ESO-1, zyxin, osteopontin, ProGRP, S100B, exhaled breath condensate, TNF-α, vascular endothelial growth factor, sICAM-1, bronchial genomic classifier, risk assessment models, Bach model, CARET, Spitz model, Liverpool Lung Project in Liverpool model, Prostate, Lung, Colorectal and Ovarian model, Brock University calculator
9.1 Other Potential Increased Risk Populations
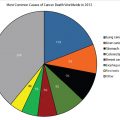
Cigarette smoking is the single most important risk factor for developing lung cancer. Despite the strong relationship between smoking and lung cancer, only about 20% of smokers develop lung cancer. Additionally, about 15 to 25% of new lung cancer diagnoses are in never smokers. Clearly other factors must also play a role in the eventual development of lung cancer.
Diverse factors such as genetic predisposition, dietary habits, cultural beliefs or faith, and environmental exposures have been investigated. Most of these factors overlap and many are common in people of the same race/ethnicity. As such, there has been significant interest in identifying racial differences and susceptibility factors to lung cancer that may affect treatment choice, treatment response, long-term follow-up, and end-of-life care.
In the NLST, 89.6% of the participants were Caucasian, whereas 4% were African Americans and 5% were of other racial groups. About 0.4% had missing racial data. Compared with Caucasians, African Americans tended to be current smokers (albeit less consumption), younger, unmarried, experienced more comorbidity, and had less formal education. However, lung cancer screening (LCS) with low-dose computed tomography (LDCT) was beneficial in all racial groups, resulting in a reduction of lung cancer mortality across all groups, but especially in African Americans. The NLST data also showed that among all racial groups, current smokers had a worse lung cancer–specific mortality, but this risk was 2X greater in current African American smokers than in Caucasians. Additionally, all-cause mortality was 1.35 times higher in African Americans than in Caucasians, but screening with LDCT had a more significant reduction in all-cause mortality in African Americans compared with Caucasians.
Smith et al examined lung cancer stage, treatment, and survival in American Indians and Alaskan Natives. The investigators found these two ethnic groups were more likely to be diagnosed with stage IIIA lung cancer and had lower 5-year survival compared to Caucasians, African Americans, and Hispanics. Racial disparity not only exists in the distribution of lung cancer, but also in treatment choices, hospice utilization, and participation in cancer clinical trials. African American and American Indians are less likely to receive stage-appropriate therapy. Byrne et al demonstrated that even though African Americans and Hispanics were equally willing to participate, Hispanics were less likely to engage in clinical trials due to language barriers, mistrust, and lack of knowledge of clinical trials. Individuals living in areas with a high percentage of either African American or Hispanics were also less likely to use hospice during the 12 months before dying of lung cancer.
Multiple risk factors including economic, behavioral, cultural, genetic, occupational, education, and awareness about screening methods may contribute to disparity in lung cancer incidence, stage at presentation, treatment choices, and survival. Genomic differences also contribute and may explain the racial differences in non–small cell lung cancer (NSCLC). The estimated prevalence of epidermal growth factor receptor (EGFR) mutations in Asians with lung adenocarcinoma is about 50 to 60%, whereas it occurs in only 15 to 20% of Caucasians. There is limited information about oncogenic drivers in African Americans and Hispanics. Steuer et al found that 81% of Asians, 53% of African Americans, and 68% of Hispanics with lung adenocarcinoma had at least one oncogenic driver mutation. Multiple studies have also identified various single nucleotide polymorphisms in Chinese, North Indian, and African American populations. These findings have been linked to an increased incidence of lung cancer along with environmental exposures and by using various prediction models have been used to identify persons at higher risk of lung cancer. Lin et al showed in a study of over 300 persons with lung cancer that African Americans were less likely to receive stage-appropriate therapy compared with Caucasians, even after adjusting for age, sex, marital status, insurance, income, and performance status. These findings were directly related to personal patient beliefs regarding lung cancer, fatalism, and medical distrust. Similar findings were found in both the American Indian and Native Alaskan population. These studies highlight factors other than genetic predisposition, and health care access may explain differences in preference and barriers to receiving stage-appropriate therapy. Hispanics are the largest and fastest growing minority group in the United States and accounted for 17% of U.S. population in 2014. Heterogeneity in lung cancer rates in Hispanics was postulated to reflect smoking patterns and their overall susceptibility to lung cancer. So it may come as a surprise that the overall percentage of Hispanic smokers is actually lower than that observed in both Caucasians and African Americans. Actually the rates are higher among U.S.-born Hispanics than among foreign-born Hispanics. Also, Cubans and Puerto Ricans are more likely to smoke than Mexicans. But, even given similar smoking patterns, Hispanics have a 30 to 70% lower relative risk of developing lung cancer than comparable African American cohorts. Interestingly, EGFR mutations are more common in Hispanics with lung adenocarcinoma than in Caucasians. Furthermore, EGFR mutations are most prevalent in Hispanics from Peru, followed by Costa Rica, Mexico, Panama, Colombia, and Argentina. There are few factors stratifying the risk at a broader level within people of different countries or race. A Chinese population-based study found the risk of lung cancer was higher in nonsmoking persons with a family history of lung cancer or any other cancer.
Dietary factors have also been shown to effect lung cancer development. In one study, higher intake of carbohydrates and fiber and lower intake of animal fat and protein have a protective effect against lung cancer. However, when adjusted for smoking history, these dietary effects were not statistically significant. This finding is consistent with recommendations of the American Institute for Cancer Research that report carotenoid-containing fruits along with nonstarchy vegetables have a protective effect against lung cancer. There is limited evidence suggesting red meat, total fat intake, and processed meat increase the risk of lung cancer. Dietary factors are often influenced by geography, ethnicity, and country of origin and can indirectly explain the racial disparity and populations at higher risk for lung cancer.
More than 11% of the U.S. population is foreign born. Immigrant population is a higher risk population due to underrepresentation in cancer-related data collection and involvement in National Cancer Institute (NCI) sponsored clinical trials. Immigrants with limited English proficiency risk being excluded from cancer research. Later stage diagnoses and higher mortality suggests that cancer disparities are common in immigrant populations. Another possible reason for such underrepresentation may be a return to the country of origin by those immigrants who wish to spend their final days among family.
Populations with chronic lung disease are also at higher risk for lung cancer. Chronic inflammation associated with diseases like chronic obstructive pulmonary disease (COPD), asthma, and tuberculosis has been contemplated to be the underlying reason for the increased risk of lung cancer in these individuals.
Islami et al even further illustrate the racial and geographic disparity in incidence, prevalence, and mortality of lung cancer. By examining age-standardized lung cancer death rates by education, race, and ethnicity, these authors concluded that 73% of U.S. lung cancer deaths could be prevented each year if overall population rates were reduced to those of educated Caucasians in lower risk states.
9.2 Role of Biomarkers
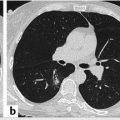
In the absence of LCS with LDCT, more than 75% of lung cancers currently will not be diagnosed until after the disease is already locally advanced or has metastasized resulting in such dismal survival rates. The 5-year survival rate in stage I NSCLC is approximately 50 to 70%. In contrast, the 5-year survival rate drops to 5 to 15% and less than 2% for patients with stage III and IV NSCLC, respectively. Obviously, diagnosing lung cancer at its earliest stages will effectively reduce mortality. Biomarkers will likely have a more prevalent role in the near future to help identify both high-risk populations while keeping false-positive rates to minimum.
Many such biomarkers have been studied and are being developed for this specific purpose. MicroRNAs (miRNAs) are one such class of biomarkers. These small, highly conversed noncoding RNAs are involved in many developmental processes and act as posttranscriptional regulators of gene expression. miRNAs regulate many biologic processes, including differentiation, proliferation, and apoptosis. Altered miRNAs expression is associated with various human cancers, acting instead as oncogenes or tumor suppressor genes. Wang et al developed a panel of three miRNAs identified in the serum of patients with early- and advanced-stage lung cancer using the TaqMan probe–based real-time reverse transcription quantitative polymerase chain reaction (RT-qPCR). These three miRNAs (miR-125a-5p, miR-25, and miR-126) were capable of distinguishing early-stage lung cancer patients from controls with 87.5% sensitivity and 87.5% specificity, respectively. Montani et al developed a panel of 13 miRNAs and performed a large-scale validation study in 1,115 high-risk individuals enrolled in the Continuous Observation of Smoking Subjects (COSMOS) LCS program. The overall accuracy, sensitivity, and specificity of the miRNA test are 74.9, 77.8, and 74.8%, respectively. Sestini et al demonstrated that a 24-plasma-based microRNA signature classifier (MSC) was capable of increasing the specificity of LDCT in a LCS trial. Five-year survival was 88.9% for low-risk MSC, 79.5% for intermediate-risk MSC, and 40.1% for high-risk MSC. The prognostic power of MSC persisted after adjusting for tumor stage. The results from a study by Li et al suggested that miR-486 and miR-150 could serve as potential blood-based biomarkers for the early diagnosis of NSCLC. Monitoring changes in miR-486 expression in plasma might be an effective method for predicting recurrence in early-staged NSCLC patients.
Ma et al tested a panel of four serum proteins: C-reactive protein (CRP) , prolactin , hepatocyte growth factor (HGF) , and circulating autoantibody against cancer-testis antigen NY-ESO-1 . Using the concentrations of all four markers as a panel along with age, gender, and smoking status, the adjusted prediction model correctly discriminated patients with benign nodules from those with lung cancer with 86.96% sensitivity and 98.25% specificity.
Kim et al detected a total of 17 proteins that were significantly elevated in the plasma of NSCLC patients, which could represent potential tumor markers. One of the novel plasma-based tumor markers, Zyxin, demonstrated a potential role as an early diagnostic marker for NSCLC.
Osteopontin (OPN) is a multifunctional cytokine involved in carcinogenesis. Kerenidi et al, in a prospective cohort study, showed increased baseline OPN circulating levels in lung cancer patients compared with controls. They also found a significant association between serum OPN levels and certain clinical parameters, including smoking status, weight loss, and performance status. In addition, their study demonstrated patients with lower OPN levels had better survival.
The primary goal of biomarkers is to identify lung cancer in its earliest stages. But biomarkers may also aid in differentiating the specific subtype of lung cancer. Yang et al, in their study of four biomarkers, found adding ProGRP increased the specificity of a previous panel of tumor markers, such as CEA (carcinoembryonic antigen), SCC, and CYFRA21–1, for NSCLC from 89.1 to 100%. Therefore, ProGRP could potentially help differentiate SCLC from NSCLC and obviate misdiagnosis of the former. Similarly, Choi et al demonstrated the role of serum S100B and S100B autoantibodies to identify brain metastasis in patients with lung cancer. This is based on the underlying principle that S100B is an astrocytic protein that enters the blood stream only when there is disruption of the blood–brain barrier (BBB). Over time, antibodies against S100B develop in the sera of patients with persistent or repeated BBB violations.
Exhaled breath condensate (EBC) is an area of great interest to many investigators. Cheng and colleagues found the expression of keratins 14, 16, and 17 was significantly different between the EBC of patients with NSCLC and healthy controls. It is unknown at this time whether these keratins are derived from the airways or from ambient air. Due to large variations in the levels of keratin expression in the respiratory tract between individuals, their use for diagnostic purposes is not recommended as a standalone biomarker at this time.
Cytokines in EBC have been widely studied targeting the detection of IL-6, vascular endothelial growth factor (VEGF), TNF-α, IL-8, and soluble intercellular adhesion molecule-1 (siCAM1). Carpagnano et al first detected increased levels of EBC IL-6 in NSCLC patients compared with controls and reported a significant positive correlation between IL-6 levels and increasing disease stage. Brussino et al showed that increased EBC IL-6 (along with IL-17 and TNF-α) was associated with increased levels of EBC VEGF , and all of these biomarkers correlated significantly with tumor diameter. Dalaveris et al also reported increased TNF- α and VEGF in patients with stages III and IV NSCLC. In another study by Carpagnano et al, increased levels of EBC IL-2 , TNF- α, and leptin were found in patients with stages I and II NSCLC compared with healthy former smokers. Jungraithmayr et al reported EBC and preoperative levels of TNF- α and sICAM-1 were significantly higher in bronchial carcinoma compared with controls undergoing thoracoscopy with minimal wedge resection. Kullmann et al published one of the few studies using a multiplexed proteomic approach to study EBC in lung cancer. These authors showed the cytokine profile in EBC of lung cancer patients was different from that of controls, regardless of their smoking habits, lung function, and airway inflammation.
Using exhaled biomarkers could be an ideal screening tool for the early detection of lung cancer because EBC collection is safe, noninvasive, and can be easily repeated. Moreover, EBC biomarkers closely represent the respiratory milieu, which could reveal subtle changes in the airway due to pathogenesis and is ideal for screening of early-stage disease in high-risk populations. However, it is not yet known if exhaled biomarkers will reveal disease-induced variations earlier or prove to be more sensitive compared to traditional systemic markers (e.g., serum and plasma) and/or imaging techniques (e.g., LDCT). Before EBC can be more broadly tested clinically, refinement of breath collection and processing methods is critical. Further studies improving the efficacy of breath condensers and standardization of EBC sampling and protein determination are required.
Bronchial genomic classifier is one of few biomarker assays commercially available. Its potential role was demonstrated in the Airway Epithelium Gene Expression in the Diagnosis of Lung Cancer (AEGIS) trials (AEGIS-1 and AEGIS-2) that enrolled 639 total patients. In these trials, 43% of bronchoscopic examinations were nondiagnostic for lung cancer, and invasive procedures were performed after bronchoscopy in 35% of patients with benign lesions. In AEGIS-1, the classifier had a sensitivity of 88% and a specificity of 47%. In AEGIS-2, the classifier had a sensitivity of 89% and a specificity of 47%. The combination of the classifier plus bronchoscopy increased sensitivity to 98% in AEGIS-2, independent of both lesion size and location. The gene-expression classifier improved the diagnostic performance of bronchoscopy for the detection of lung cancer. In intermediate-risk patients with a nondiagnostic bronchoscopic examination, a negative classifier score provided support for a more conservative diagnostic approach. A follow-up study to determine the clinical implication of these results suggested recommendations for invasive procedures were reduced from 57% without the classifier to 18% with a low-risk classifier result. Invasive procedure recommendations increased from 50 to 65% with a positive (intermediate-risk) classifier result. When stratifying by ultimate disease diagnosis, there was an overall reduction in invasive procedure recommendations in patients with benign disease when classifier results were reported (54–41%). For patients ultimately diagnosed with malignant disease, there was an overall increase in invasive procedure recommendations when the classifier results were reported (50–64%).
Salivary microbiota are another class of potential biomarkers. Yan et al showed salivary Capnocytophaga and Veillonella had an 84.6% sensitivity and 86.7% specificity in distinguishing patients with squamous cell lung cancer from controls and 78.6% sensitivity and 80.0% specificity in distinguishing those with lung adenocarcinoma from controls.
A few in vitro studies have demonstrated other potential biomarkers including Stanniocalcin-2 . The latter was elevated in tissue samples of patients with lung cancer and seemed to have influential role in the development of metastasis, but this has not been validated in prospective in vivo studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree