9 Infrahyoid Neck
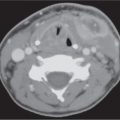
As in the suprahyoid neck, the structures of the infrahyoid neck are surrounded by a layer of subcutaneous tissue (superficial cervical fascia) and are compartmentalized by three layers of the deep cervical fascia: superficial (investing), middle (visceral), and deep (prevertebral). The infrahyoid neck contains 10 distinct spaces defined by the layers of the deep cervical fascia (Fig. 9.1). The visceral space, retropharyngeal space, danger space, and perivertebral space are midline, nonpaired spaces. The anterior cervical space, carotid space, and posterior cervical space are lateral, paired spaces. Of these spaces, only the visceral space and the paired anterior cervical space are unique to the infrahyoid neck. The carotid, retropharyngeal, danger, and perivertebral spaces all traverse both the suprahyoid and infrahyoid neck.
The visceral space is a cylindrical space in the anterior mid-line of the infrahyoid neck, completely enclosed by the middle layer (visceral fascia) of the deep cervical fascia. It is the largest space of the infrahyoid neck, extending from the hyoid bone to the upper mediastinum. It is bordered posteriorly by the retropharyngeal space and posterolaterally by the carotid space bilaterally. Paired anterior cervical spaces are lateral to the visceral space and are continuous with the submandibular spaces superiorly. The contents of the visceral space include the larynx, cervical trachea, hypopharynx, cervical esophagus, thyroid gland, parathyroid glands, recurrent laryngeal nerves, and lymph nodes (level VI group).
A visceral space mass presentation depends on the structures involved. The center of a thyroid mass is within the thyroid gland, with thyroid tissue seen surrounding the lesion. The ipsilateral carotid space is displaced laterally, and the trachea and esophagus are displaced to the side opposite the lesion. The center of a parathyroid mass is between the thyroid gland anteriorly and the longus colli muscle posteriorly (tracheoesophageal groove). When large, parathyroid lesions displace the thyroid lobe anteriorly and the adjacent carotid space anterolaterally. The best indicator of a hypopharyngeal malignancy is a bulky mass with invasion and destruction of submucosal and deep structures, as well as associated necrotic lymph nodes. Cervical esophageal mass lesions are centered in the middle of the posterior visceral space, immediately posterior to the trachea, abutting or surrounding the esophagus, and displace the trachea and thyroid gland anteriorly. The esophagus can pouch out from its normal, retrotracheal location into the tracheoesophageal groove and mimic a paraesophageal nodal mass. Laryngeal lesions are centered within the cartilaginous edifice of the larynx. A cervical tracheal mass lesion is centered in the tracheal wall and may displace the thyroid gland laterally and the esophagus posteriorly.
The retropharyngeal space (RPS), a midline space just posterior to the aerodigestive tract, continues into the infrahyoid neck from the suprahyoid neck above and extends inferiorly to the level of the upper thoracic spine. Unlike the suprahyoid RPS, which contains both fat and lymph nodes, the infrahyoid RPS contains only fat, defined by the visceral fascia anteriorly and the alar fascia posteriorly. The danger space lies between the RPS and perivertebral space in the midline. It continues into the infrahyoid neck from the suprahyoid neck above and extends inferiorly to the diaphragm. It is a potential space, normally containing only fat, and is formed between two parallel slips of the deep layer of the deep cervical fascia, the alar fascia anteriorly and laterally and the prevertebral fascia posteriorly. Although separately defined fascial spaces, the “true” RPS and the danger space are considered together, because they cannot be differentiated from one another by means of sectional imaging.
A mass of the infrahyoid RPS appears rectangular shaped or oval and is centered anterior to the prevertebral muscles and posterior to the visceral space. A mass remains anterior to and flattens prevertebral muscles, as it enlarges and may displace the carotid space laterally. The infrahyoid RPS may be involved by processes arising from tissues within this space, but more commonly it is affected by external invasion from adjacent spaces.
The perivertebral space (PVS), a large cylindrical space surrounding the vertebral column, continues into the infrahyoid neck from the suprahyoid neck above and extends inferiorly to the upper mediastinum. The PVS is completely bordered by the tenacious deep layer of the deep cervical fascia. The attachment of the fascia to the transverse processes of the vertebral body divides the PVS into the anterior prevertebral portion and the posterior paraspinal portion. The contents of the prevertebral portion include the prevertebral muscles, scalene muscles, brachial plexus roots, phrenic nerve, vertebral artery and vein, and vertebral body. The paraspinal portion contains the paraspinal muscles, fat, and posterior elements of the vertebral body. In the infrahyoid neck, the PVS is bordered anteriorly by the RPS, anterolaterally by the carotid space, and posteriorly and laterally by the posterior cervical space.
A mass lesion of the prevertebral portion is centered within the prevertebral muscles or corpus of the vertebral body and elevates the prevertebral muscles, pushing the retropharyngeal space anteriorly. A mass lesion of the paraspinal portion is centered within the paraspinal musculature or the posterior elements of the spine, pushing the fat of the posterior cervical space away. This space is susceptible to the same inflammatory, infectious, and neoplastic processes as the suprahyoid component.
The carotid space is a paired tubular space, encircled by the carotid sheath, composed by slips of all three layers of the deep cervical fascia. The infrahyoid carotid space contains the common carotid artery, internal jugular vein, and vagus nerve. The sympathetic plexus is embedded in the medial sheath walls (between the medial carotid space and the lateral RPS). The internal jugular nodal chain (nodal levels III and IV) is found along the length of the internal jugular vein within the outer layers of the carotid sheath. In the infrahyoid neck, the carotid space is bordered anteriorly by the anterior cervical space, laterally by the sternocleidomastoid muscle, posteriorly by the posterior cervical space and prevertebral space, and medially by the visceral space and RPS.
The center of a carotid space mass in the infrahyoid neck is typically in close association with the carotid artery and the jugular vein. As a carotid space mass enlarges, it may engulf the vessels or push them apart.
The posterior cervical space (PCS) represents the paired posterolateral compartment of the neck confined anteriorly by the carotid space, medially by the deep layer of the deep cervical fascia enveloping the perivertebral space, and laterally and posteriorly by the superficial layer of the deep cervical fascia, just deep to the sternocleidomastoid muscle and the trapezius muscle. Most of the PCS is below the hyoid bone, although the very top of this space extends well into the suprahyoid neck. The contents of the PCS include fat, the spinal accessory nerve, the spinal accessory lymph node chain (node level V), and the preaxillary brachial plexus.

A PCS mass is centered in the fat of the PVS. A strip of fat must separate the mass from the carotid space. Large tumors displace the carotid space anteromedially, elevate the sternocleidomastoid muscle, and compress deeper prevertebral and paraspinal structures.
The anterior cervical space (ACS) is a small, paired space of the ventral infrahyoid neck, encircled by layers of the deep cervical fascia. It is lateral of the visceral space, medial of the sterno-cleidomastoid muscle, and ventral of the carotid space. The ACS is the inferior extension of the submandibular space into the infrahyoid neck and contains only fat.
An ACS mass is centered in the fat of the ACS. Large masses elevate the sternocleidomastoid muscle, displace the carotid space vessels posteromedially, and may compress the thyroid gland lobe. The ACS may be important for mediastinal extension of cervical abscesses.
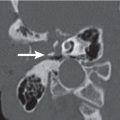
The larynx has a framework consisting of a cartilaginous skeleton connected by membranes and ligaments and moved by muscles. The laryngeal skeleton consists of the hyoid bone, cricoid, thyroid, epiglottis, and paired arytenoid cartilages. This framework supports the mucosa-covered surfaces of the larynx. The endolarynx can be subdivided into the supraglottis, glottis, and subglottis. The supraglottis extends from the tip of the epiglottis above to the laryngeal ventricle below. The glottis includes the true vocal cords and both the anterior and posterior commissures. The subglottis extends from the inferior border of the glottic region to the inferior edge of the cricoid cartilage. There are three intralaryngeal compartments: the paired lateral paraglottic space and the midline preepiglottic space. The paraglottic space lies between the mucosa and the laryngeal framework and is paired and symmetric. The preepiglottic space is a triangular, C-shaped, fat-filled space set between the hyoid bone anteriorly and the epiglottis posteriorly. All structures that predominantly contain fat (preepiglottic space, paraglottic spaces, aryepiglottic folds, and false cords) are hypoattenuating on computed tomography (CT) images. Ossified cartilage shows a high-attenuating outer and inner cortex and a central low-attenuating medullary space due to fatty tissue. Nonossified hyaline cartilage and nonossified fibroelastic cartilage have the attenuation values of soft tissue. On contrast-enhanced CT, neither the mucosal surface nor the submucosal structures of the larynx show enhancement. The abducted position of the true vocal cords during quiet breathing facilitates evaluation of the anterior and posterior commissures. Additional scans obtained with phonation or modified Valsalva maneuvers facilitate evaluation of the aryepiglottic fold, laryngeal ventricle, and hypopharynx.
The primary sign of tumor spread to the deep paralaryngeal spaces on CT is replacement of fatty tissue with fat density by tumor tissue with intermediate density. Neoplastic cartilage invasion occurs preferentially where the attachments of Sharpey fibers interrupt the perichondrium, thus acting as direct pathways for tumor spread into the cartilaginous tissue. These areas typically include the anterior commissure, the junction of the anterior one fourth and posterior three fourths of the lower thyroid lamina, the posterior border of the thyroid lamina, the cricoarytenoid joint, and the area of attachment of the cricothyroid membrane. The diagnosis of neoplastic cartilage invasion on CT is mainly based on the presence of tumor on both sides of a laryngeal cartilage (extralaryngeal tumor spread), combined with erosion or lysis in the thyroid, cricoid, and arytenoid cartilage and sclerosis in the cricoid and arytenoid (but not the thyroid) cartilage.
The hypopharynx is the most caudal portion of the pharynx and extends from the level of the hyoid bone and valleculae to the upper esophageal sphincter. It is formed for the most part by the inferior pharyngeal constrictor muscles. The hypopharynx includes the piriform sinuses, the postcricoid region, and the posterior hypopharyngeal wall. The piriform sinus is situated bilaterally between the thyroid cartilage and the aryepiglottic fold, and is adjacent to the paraglottic space and the cricoid cartilage. The postcricoid region extends from the cricoarytenoid joints to the lower edge of the cricoid cartilage (c ricopharyngeus muscle). The posterior wall of the hypopharynx is the inferior continuation of the posterior oropharynx wall. The mucosal surface of the hypopharynx frequently displays a distinct contrast enhancement; the muscular tissue is not enhancing. The hypopharynx may be filled with air or may be collapsed during quiet respiration (a modified Valsalva maneuver may distend this region and rule out the presence of a tumor).
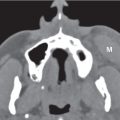
Thyroid lesions are primarily evaluated with radionuclide scanning and ultrasonography. Because of its iodide content, the normal thyroid gland has a density of 80 to 100 HU on CT. After injection of contrast material, the thyroid gland enhances tremendously (drawback: because of iodine uptake from the contrast agent, thyroid localization with nuclear scintigraphy and radioactive iodine treatment must be delayed 4 to 8 weeks after administration of iodinated contrast agents). Thyroid nodules are common and comprise adenomas, cysts, focal thyroiditis, multinodular goiter, and malignant tumors. A multiplicity of nodules in an enlarged thyroid gland usually suggests a benign process or metastases. Calcification occurs in 13% of all thyroid lesions, including 17% of all malignancies and 11% of all benign processes. Punctate, linear, nodular, amorphous, and peripheral eggshell-like calcifications occur in benign and malignant thyroid tumors, whereas fine punctate calcification is more indicative of malignancy. Cystic areas occur in many thyroid masses; 38% of malignancies have cystic components, and 62% of benign masses may be entirely or partly cystic. Hemorrhage may be found in papillary carcinomas or goiters.
Once a lesion is identified as in an infrahyoid neck space, the differential diagnosis should be reviewed. The differential diagnosis of the visceral space lesions as seen on CT is discussed in Table 9.1, of laryngeal lesions in Table 9.2 , of thyroid gland lesions in Table 9.3 , of infrahyoid carotid space lesions in T able 9.4 , of posterior cervical space lesions in Table 9.5 , of infrahyoid retropharyngeal space lesions in Table 9.6 , of infrahyoid perivertebral space lesions in Table 9.7 , and of anterior cervical space lesions in Table 9.8.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree