Chapter Outline
From the 1970s to 1990s, the abdominal radiograph traditionally served as the initial radiologic means of evaluating patients with suspected abdominal pathology. During the past two decades, however, computed tomography (CT) has become the major imaging procedure in patients with suspected acute abdominal pathology. When abdominal radiography was performed as a screening test, the diagnostic yield of this examination was low and most abnormalities that were detected were nonspecific. In a review of 1780 screening abdominal radiographs, important abnormalities were found in only 10% of cases. No clinically significant disease would have been missed if abdominal radiographs had been obtained only in patients with a strong clinical suspicion of disease and/or moderate to severe abdominal symptoms. Abdominal radiographs have the greatest value in patients in whom bowel obstruction or perforation, urinary calculi, or bowel ischemia is suggested on clinical grounds. In patients with mild or nonspecific symptoms, however, abdominal radiographs have a low diagnostic yield. The major value of a normal abdominal series is the exclusion of bowel obstruction or free air secondary to bowel perforation. Despite the increasing use of CT and the declining role of abdominal radiography, this examination is still performed in many patients, especially those who have undergone recent surgery and those who have some form of catheter, tube, or drain in the abdomen. Emergency department physicians may also order abdominal radiographs in patients with a low clinical suspicion of disease to ensure that a major abdominal disorder is not overlooked and to calm a concerned patient.
Technique
Standard Projections
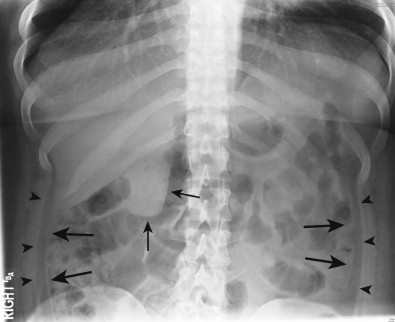
An anteroposterior radiograph taken with the patient in a supine position is the most common plain film examination of the abdomen ( Fig. 11-1 ). Whether one uses conventional film or digital techniques, the patient should be positioned comfortably on his or her back, without rotation of the pelvis. Maximal relaxation of the abdominal musculature is important in reducing artifact caused by motion; this is facilitated by supporting and slightly flexing the patient’s knees. The film or field of view for digital imaging should be positioned with its lower edge at the symphysis pubis and the x-ray beam centered at the iliac crest. Both the lung bases and symphysis pubis should be included on the radiograph. The exposure is made during expiration and should begin 1 to 2 seconds after respiration is suspended.
Delineation of intra-abdominal soft tissues on abdominal radiographs depends on the inherent contrast provided by soft tissues, fat, and intraluminal gas. Subject contrast on the radiograph is caused by differential attenuation of the x-ray beam in the patient. Most abdominal radiographs are taken using routine equipment exposed at a low kilovoltage (60-75 kV), depending on the size of the patient. A short exposure time is desirable to avoid motion unsharpness. Also, an increase in peak kilovoltage increases scattered radiation, which degrades soft tissue contrast. Thus, the lowest possible peak kilovoltage that can penetrate the patient and has an acceptable exposure time should be used. With conventional films, a reciprocating (Potter-Bucky) grid and careful collimation are used to reduce scatter. In males with reproductive potential, gonadal shielding should be used if the gonads lie within 5 cm of the primary beam and if such shielding does not compromise the clinical objectives of the examination.
Portable abdominal radiographs may be obtained in hospitalized, extremely ill patients; however, these radiographs are usually of lower quality than standard abdominal radiographs obtained in the radiology department. Such patients are usually too ill to breath-hold, and most portable x-ray units have fixed milliampere settings, which may necessitate using techniques of higher peak kilovoltage, resulting in reduced contrast. In addition, a stationary grid, rather than a Potter-Bucky grid, must be used to control scatter, and when these grids are poorly positioned, the image may be degraded secondary to grid cutoff. Whenever possible, abdominal radiographs should therefore be obtained using standard x-ray equipment in the radiology department.
Supplemental Projections
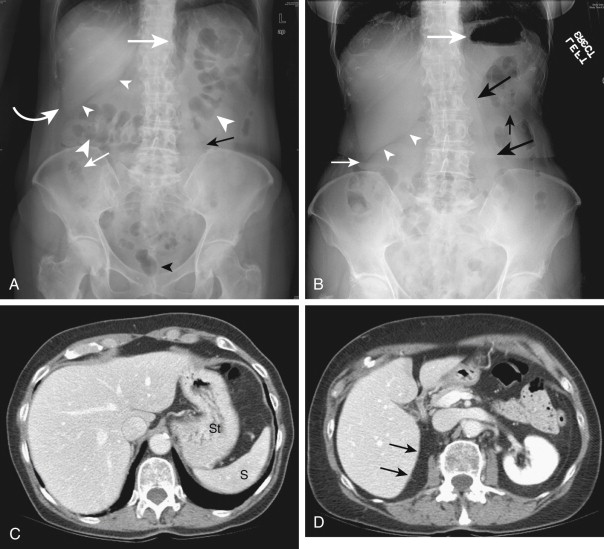
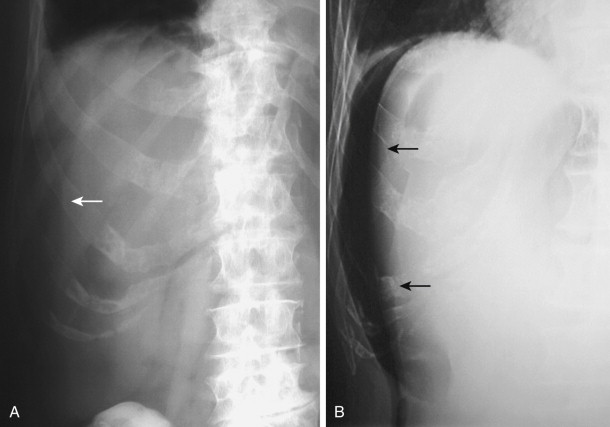
In addition to the standard anteroposterior supine view, other projections may help in specific clinical situations and are frequently used as part of a routine abdominal series. In patients with abdominal pain, upright posteroanterior abdominal or chest radiographs may be useful to facilitate detection of small amounts of free intraperitoneal air, small bowel obstruction, and unsuspected thoracic disease that is causing abdominal pain ( Fig. 11-2 ; see Fig. 11-1B ).
An upright abdominal radiograph is often ordered on a routine basis, but some authors believe that it does not contribute significant information in many patients. Mirvis and colleagues reviewed the emergency department radiographs of 252 patients, which included supine and upright abdominal radiographs and upright chest radiographs. The upright abdominal radiographs did not contribute to the treatment of any patients with acute abdominal conditions in their series. The authors concluded that this view could be omitted to reduce the time and cost of the examination without sacrificing important diagnostic information. However, upright abdominal radiographs may be helpful in patients with suspected bowel obstruction who have a gasless abdomen on supine radiographs to assess the appearance of gas and fluid in the small bowel further (see Fig. 11-2A and B ). Alternatively, this information could be obtained on abdominal radiographs taken with the patient in the lateral decubitus position. For extremely ill patients who cannot stand easily, a lateral decubitus view may be more helpful than a suboptimal upright radiograph.
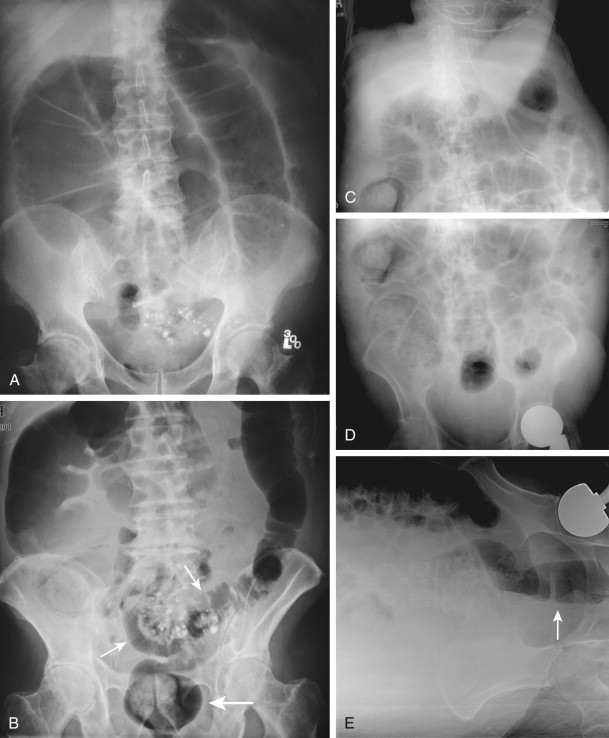
Miller and Nelson showed that when a perforated viscus is suspected on clinical grounds, a specific sequence of exposures is most likely to demonstrate extraluminal gas. They recommended that the patient be placed in the left side down position for at least 10 minutes before a left lateral decubitus view is obtained. This allows gas to rise and accumulate over the right margin of the liver and, occasionally, beneath the iliac crest. If the patient is unable to stand, an abdominal radiograph should be obtained with the patient in the left lateral decubitus position with a horizontal beam, using a short exposure technique. This results in underpenetration of the abdominal viscera but good visualization of extra-alimentary gas between the nondependent lateral abdominal wall and liver ( Fig. 11-3 ). If the patient is able to stand, the table is tilted upright and an upright posteroanterior chest radiograph is obtained. In one study, lateral chest radiographs were found to be superior to frontal radiographs in detecting subtle pneumoperitoneum. Radiographs of the abdomen in upright and supine positions are also obtained to complete the so-called perforation series (see Fig. 11-2C and D ). Even tiny amounts of free air can be detected with use of the proper technique (see Fig. 11-2E ). Some authors have reported that upright posteroanterior chest radiographs are more sensitive for detecting pneumoperitoneum than upright abdominal radiographs. This difference in sensitivity probably occurs because the x-ray beam is centered at the iliac crest on abdominal radiographs, so that it penetrates air beneath the diaphragm obliquely rather than tangentially, making small gas collections more difficult to detect. The higher exposure techniques required to penetrate the abdomen also result in excessive penetration at the lung interface, sometimes obscuring small collections of free intraperitoneal air. Nevertheless, most experts believe that upright and supine abdominal radiographs are a useful part of the abdominal series for detecting intra-abdominal disease in these patients.
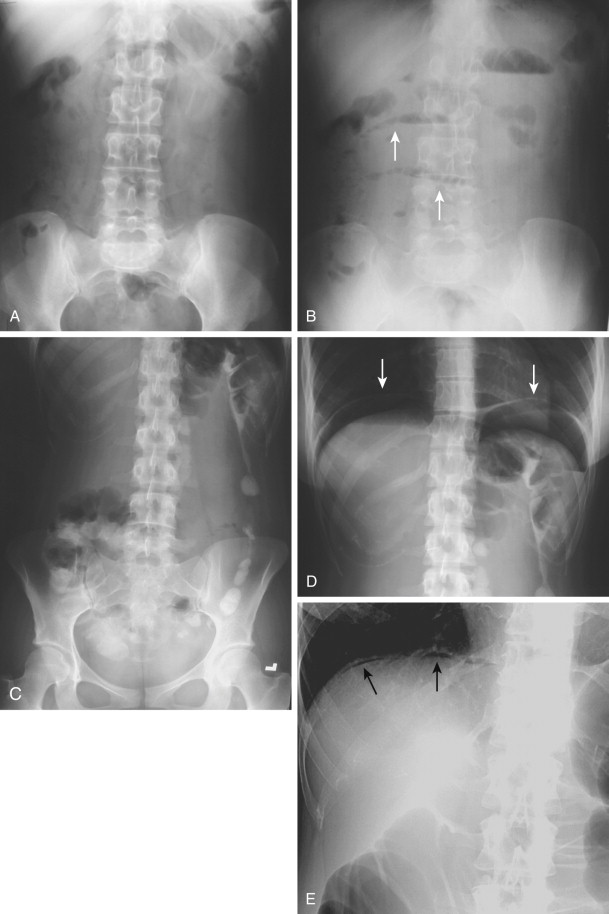
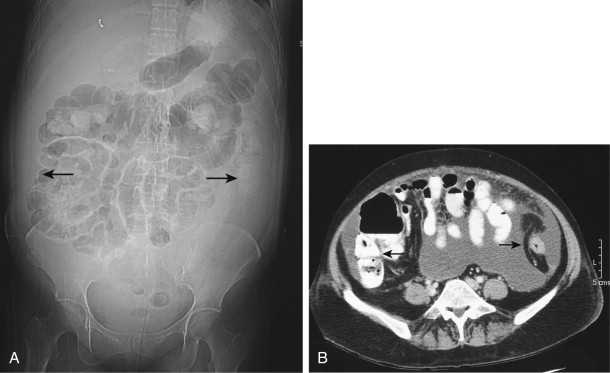
Additional projections such as prone, oblique, lateral, or coned views may be helpful in some clinical situations for better defining and localizing mass lesions, calcifications, or hernias. When distal colonic obstruction is suspected, prone abdominal radiographs are more helpful than supine radiographs because colonic gas occupies the more anterior transverse and sigmoid segments of the colon with the patient in the supine position ( Fig. 11-4A, C, and D ). As a result, a distal colonic obstruction may be difficult to distinguish from an ileus or pseudo-obstruction on supine and upright views of the abdomen. In this situation, a prone radiograph ( Fig. 11-4B ) or right lateral decubitus radiograph ( Fig. 11-4E ) may be useful because abdominal radiographs in these positions allow gas to fill the rectosigmoid colon if no mechanical obstruction is present.
Normal Anatomy
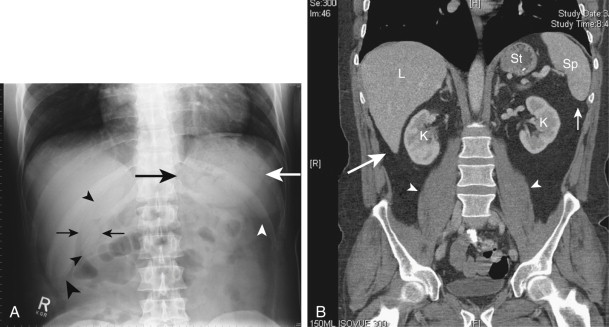
Abdominal soft tissue planes and visceral surfaces are visible on abdominal radiographs because of the natural contrast created by surrounding fat. The best visualized interfaces are those that are smoothly marginated and oriented in a sagittal or transverse plane tangential to the incident x-ray beam. Familiarity with the location of abdominal organs and the most commonly visualized tissue planes is helpful for identifying normal anatomic structures and recognizing and localizing pathologic processes.
Peritoneal Cavity
Liver
In the normal adult, the liver occupies the right upper quadrant of the abdomen. It measures 20 to 22 cm in its greatest transverse dimension and 15 to 17 cm in its greatest vertical dimension near its right lateral border. There is considerable variation in the normal shape of the liver. With its most cephalad portion lying just beneath the dome of the right hemidiaphragm, the superior aspect of the liver is commonly S-shaped or concave. The inferior edge is usually triangular, with its apex directed caudad toward the right lower quadrant. Between 4% and 14% of the population has a prominent inferior extension of the right lower lobe, also known as Riedel’s lobe. This lobe usually extends caudally below the iliac crest and does not by itself indicate hepatomegaly.
Although intraperitoneal fat is not always present around the liver, the right inferior edge of the liver (hepatic angle) is often visible on abdominal radiographs because it indents the extraperitoneal fat in the parietal peritoneum ( Fig. 11-5 ; see Fig. 11-1 ). This fat consists of posterior pararenal fat laterally and perirenal fat medially. The perirenal fat may outline not only the medial aspect of the hepatic angle but also the more cephalad portion of the posteromedial surface of the right lobe of the liver (see Fig. 11-1A ). The hepatic angle may be obscured by effusions or blood that infiltrate the retroperitoneal fat or by ascites that displaces the liver edge away from the adjacent fat ( Fig. 11-6 ). The posterior edge of the liver is visible on abdominal radiographs (see Fig. 11-1 ), whereas the anterior and left lateral margins of the liver are not. Because it is the anterior margin of an enlarged liver that is palpated on physical examination, a discrepancy may arise between clinical and radiographic measurements of the liver. On abdominal radiographs, hepatomegaly may be diagnosed by elevation of the right hemidiaphragm, visualization of the entire liver (not just a Riedel’s lobe) extending into the lower abdomen, inferior displacement of the hepatic flexure of the colon, and lateral displacement of the lesser curvature of the stomach by an enlarged left lobe of the liver.
Gallbladder
The gallbladder occupies a shallow fossa on the inferior surface of the liver between the right and left lobes and is not usually visualized on abdominal radiographs. The gallbladder lies superior and lateral to the duodenal bulb and gastric antrum and superior to the proximal transverse colon. Occasionally, the fundus of the gallbladder may be visualized in normal patients if it indents the surrounding fat ( Fig. 11-7 ; see Fig. 11-5A ). Only about 15% of gallstones are sufficiently calcified to be seen on abdominal radiographs, so the abdominal series is a poor screening study for gallbladder disease.