Chapter Outline
The abdomen is a closely packed space containing numerous conduits and organs related to each other in a complex spatial arrangement. Each of these structures is subject to a unique range of diseases, all having specific causes and characteristic manifestations. However, the spectrum of findings on abdominal radiographs is surprisingly limited. Important signs include displacement, enlargement, or atrophy of organs, distention of bowel, extraluminal gas, and calcification in parenchymal and supporting tissues. In many cases, the pattern of calcium deposition is the most informative and distinctive radiographic finding.
Calcification may occur in the wall of blood vessels or other conduits, the lumen of hollow structures, and the solid substance of viscera or neoplasms. Despite the variety of causes of abdominal calcification, a systematic evaluation of the morphologic features, location, and mobility of an abnormal opacity usually narrows the diagnostic considerations to just a few likely possibilities. In many cases, analysis of the appearance of an abdominal calcification on abdominal radiographs provides sufficient information for an unequivocal diagnosis without need for additional examinations. In other cases, careful assessment of the morphology, location, and mobility of an abdominal calcification helps focus the choice and sequence of subsequent imaging examinations.
Physiology
The precipitation of calcareous substances requires an alkaline medium and high local concentrations of ionic calcium. The term metastatic calcification refers to the deposition of calcium salts in normal tissues as the result of hypercalcemia and an elevated pH. Although the stomach and kidneys are the most frequent sites of metastatic calcification in the abdomen, the degree of parenchymal opacification in these organs is usually too faint to be detected on abdominal radiographs. The most common cause of radiographically detectable metastatic calcification is chronic renal failure with secondary hyperparathyroidism. As a result of this pathologic process, diffuse opacification of the kidneys is often accompanied by osteomalacia or osteoporosis.
The term dystrophic calcification refers to a phenomenon, far more frequent than metastatic calcification, that occurs despite normal serum levels of calcium. Dystrophic calcification may be caused by trauma, ischemia, infarction, or other pathologic processes, resulting in a predisposition to calcium deposition. In some tumors, the rapid breakdown of lipids releases fatty acids that bind calcium with particular avidity. Mucin-producing adenocarcinomas of the gastrointestinal (GI) tract possess a glycoprotein similar in chemical configuration to cartilage and share with it an affinity for calcium aggregation. Although some structures in the abdomen have a propensity for dystrophic calcification, the mechanisms and kinetics of calcium deposition have not been fully elucidated.
Some devitalized or degenerative tissues are also associated with new bone formation. However, ossification is less common than dystrophic calcification. Calcified osteoid may be found as an isolated finding, or it may coexist with adjacent areas of calcium deposition that lack the histologic structure of bone. In either case, local tissue damage appears to be the precipitating factor. Ossification may occur in ovarian or retroperitoneal teratomas ( Fig. 13-1 ), abdominal scars, particularly after gastric surgery or suprapubic bladder catheterization and, rarely, colonic and retroperitoneal neoplasms.

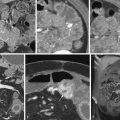
Papillary serous cystadenocarcinomas of the ovary often contain a distinctive form of calcification characterized by a psammomatous or cloudlike opacity attributable to intracellular deposition of calcium salts in the lesion ( Fig. 13-2 ). In contrast, dystrophic calcification associated with other metastatic tumors is caused by extracellular precipitation of calcium salts. Psammomatous and dystrophic calcification may be manifested by amorphous, poorly outlined areas of increased density. When this finding occurs, the distribution of calcified metastases may narrow the differential diagnosis, sometimes leading to an unequivocal diagnosis.

Morphology
The recognition of specific abdominal calcifications has been aided by the attribution of vivid descriptive names to particular radiopacities. For example, a “staghorn calculus” is a large, branching opacity in the renal pelvis. Such appellations are highly evocative and easily remembered; however, they do not help generate a differential diagnosis from among the many causes of abdominal calcification. Unfortunately, most surveys of abdominal calcification have relied primarily on such descriptive designations and have failed to emphasize diagnostic features that might help organize the various opacities into categories with shared characteristics.
In this chapter, a logical scheme is presented for classifying almost all abdominal calcifications. They may be distinguished radiographically on the basis of various morphologic features, including contour, border, sharpness, marginal continuity, and internal architecture. Consideration of these features permits a grouping of calcifications into one of four classes: (1) concretions; (2) conduit wall calcification; (3) cystic calcification; and (4) solid mass calcification. In the following sections, the distinguishing features of each class are discussed in detail. Potential pitfalls and notable exceptions are also considered.
Concretions
Concretions are precipitates removed from solution in a liquid medium inside a vessel or hollow viscus. They often contain a central nidus, composed of an insoluble substance such as an inorganic foreign body, ingested vegetable matter, thrombus, or focal collection of pus and cellular debris. In pelvic veins and in the GI and genitourinary tracts, concretions are likely to calcify. They can be brightly or faintly opaque; the radiographic density depends on the size of the opacity and amount of calcium per unit volume. Concretions do not have a common shape. Biliary calculi are usually oval or rounded, whereas gallstones are often faceted ( Fig. 13-3 ). Ureteral and pancreatic stones often have jagged edges, but in hollow viscera such as the urinary bladder and gallbladder, the concretions usually have smooth margins.

A sharply defined, continuous external margin is a unifying feature of concretions. Stones are almost always characterized by an uninterrupted edge of calcification throughout their entire perimeter, with no lucent gaps along the interface with the surrounding medium. This unique feature permits differentiation of small stones with radiolucent centers from calcified vessels seen on end. The circumferential opacification of the perimeter of large stones also helps distinguish them from calcified cysts.
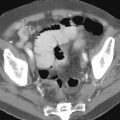
Concretions may vary greatly in their internal architecture. A stone may be homogeneously dense, a pattern often encountered in urinary calculi, or it may contain a slightly eccentric area of lucency, an appearance typical of phleboliths ( Fig. 13-4 ). Concentric laminations are characteristic of gallstones, bladder concretions, and appendicoliths ( Fig. 13-5 ). Each of these various internal configurations has a certain predictability and uniformity. A central lucency is often present. Stones seldom have a mottled, speckled, or patchy appearance. The deposition of calcium on only one surface of the stone is extremely rare.