GROSS ANATOMY
Overview
- •
Major lymphatic vessels and nodal chains lie along major blood vessels (aorta, inferior vena cava, iliac)
- •
Lymph nodes carry same name as vessel they accompany
- •
Lymph from alimentary tract, liver, spleen, and pancreas passes along celiac, superior mesenteric chains to nodes
- ○
Efferent vessels from alimentary nodes form intestinal lymphatic trunks
- ○
Cisterna chyli (chyle cistern)
- –
Formed by confluence of intestinal lymphatic trunks and right and left lumbar lymphatic trunks, which receive lymph from nonalimentary viscera, abdominal wall, and lower extremities
- –
May be discrete sac or plexiform convergence
- –
- ○
- •
Thoracic duct: Inferior extent is chyle cistern at L1-L2 level
- ○
Formed by convergence of main lymphatic ducts of abdomen
- ○
Ascends through aortic hiatus in diaphragm to enter posterior mediastinum
- ○
Ends by entering junction of left subclavian and internal jugular veins
- ○
- •
Lymphatic system drains surplus fluid from extracellular spaces and returns it to bloodstream
- ○
Important function in defense against infection, inflammation, and tumor via lymphoid tissue present in lymph nodes, gut wall, spleen, and thymus
- ○
Absorbs and transports dietary lipids from intestine to thoracic duct and bloodstream
- ○
- •
Lymph nodes
- ○
Composed of cortex and medulla
- ○
Invested in fibrous capsule, which extends into nodal parenchyma to form trabeculae
- ○
Internal honeycomb structure filled with lymphocytes that collect and destroy pathogens
- ○
Hilum: In concave side, with artery and vein, surrounded by fat
- ○
Abdominopelvic Nodes
- •
Preaortic nodes
- ○
Celiac nodes: Drainage from gastric nodes, hepatic nodes, and pancreaticosplenic nodes
- ○
Superior and inferior mesenteric nodes: Drainage from mesenteric nodes
- ○
- •
Lateral aortic (paraaortic/paracaval) nodes
- ○
Drainage from kidneys, adrenal glands, ureter, posterior abdominal wall, testes and ovary, uterus, and fallopian tubes
- ○
- •
Retroaortic nodes
- ○
Drainage from posterior abdominal wall
- ○
- •
External iliac nodes
- ○
Primary drainage from inguinal nodes
- ○
Flow into common iliac nodes
- ○
- •
Internal iliac nodes
- ○
Drainage from inferior pelvic viscera, deep perineum, and gluteal region
- ○
Flow into common iliac nodes
- ○
- •
Common iliac nodes
- ○
Drainage from external iliac, internal iliac, and sacral nodes
- ○
Flow into lumbar (lateral aortic) chain of nodes
- ○
- •
Superficial inguinal nodes
- ○
In superficial fascia parallel to inguinal ligament, along cephalad portion of greater saphenous vein
- ○
Receive lymphatic drainage from superficial lower extremity, superficial abdominal wall, and perineum
- ○
Flow into deep inguinal and external iliac nodes
- ○
- •
Deep inguinal nodes
- ○
Along medial side of femoral vein, deep to fascia lata and inguinal ligament
- ○
Receive lymphatic drainage from superficial inguinal and popliteal nodes
- ○
Flow into external iliac nodes
- ○
IMAGING ANATOMY
Overview
- •
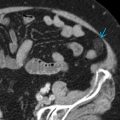
CT is test of choice for cancer staging
- •
May be supplemented by PET/CT in select cancers
- •
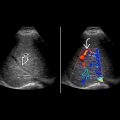
US may be useful in children or thin adults
- ○
Normal nodes are elliptical with echogenic fatty hilum and uniform hypoechoic cortex
- ○
Normal lymph nodes rarely detected on abdominal US
- ○
- •
Normal diameter of lymph node varies depending on location
- ○
Short-axis diameter
- –
Abdominopelvic < 10 mm
- –
Hepatogastric ligament < 8 mm
- –
Retrocrural < 6 mm
- –
- ○
ANATOMY IMAGING ISSUES
Imaging Recommendations
- •
Transducer: 2-5 MHz or 5-9 MHz for thinner adult patients
- •
Patient examined in supine position with > 4 hours of fasting to decrease bowel gas
- •
Graded compression technique to clear overlying bowel loops
CLINICAL IMPLICATIONS
Clinical Importance
- •
Nodal enlargement is nonspecific, may be neoplastic, inflammatory, or reactive
- •
Normal-sized lymph nodes may harbor metastatic malignancy
- •
Node morphology is more specific for pathology
- ○
Abnormal nodes have replacement or loss of fatty hilum
- ○
Look for central necrosis, cystic change, or calcification
- ○
- •
Lymphoma
- ○
Multiple enlarged hypoechoic or anechoic nodes
- ○
- •
Metastatic lymphadenopathy
- ○
More echogenic and heterogeneous nodes compared to lymphomatous nodes
- ○
- •
Infectious/reactive lymphadenopathy
- ○
Nonspecific sonographic features
- ○
May contain necrotic centers in mycobacterial infection
- ○
RETROPERITONEAL LYMPH NODES