In the hemodynamic unstable young patient, the first evaluation is performed through e-FAST, a rapid diagnostic method carried out during the first aid approach, which is necessary to depict the presence of hemothorax and pneumothorax and hemoperitoneum.
Should the hemodynamic stabilization occur, and in all stable patients with high-energy trauma, contrast-enhanced CT is performed, which is the gold standard in the evaluation of the injured patient.
After the initial evaluation and during follow-up procedures, the monitoring of an injured child must be performed according to radioprotection criteria, keeping in mind the patient’s medical condition and laboratory exams [4, 5].
4.2 Ultrasound Technique
In high-energy blunt abdominal trauma, emergency US is performed in the emergency room on the unstable patient through e-FAST technique: the purpose is to depict the eventual hemoperitoneum in the four standard abdominal areas, right hypochondrium, left hypochondrium, epigastrium, and pelvis.
In fact, this technique has a high sensitivity, up to 99 % in literature review, in detecting abdominal free fluid even in small amounts. The aim of the exam is to depict in real time a huge hemoperitoneum that may be the cause of hemodynamic instability, which requests an immediate surgery. Therefore, the purpose of FAST is not the evaluation of abdominal parenchymal organs, which instead is carried out by means of computed tomography once hemodynamic stabilization is reached.
In low-energy or localized trauma, basic US is fundamental not only to evaluate the presence of hemoperitoneum but also to highlight parenchymal injuries.
For the latter purpose, US diagnostic efficiency has highly increased with the use of second-generation blood pool contrast agent, performing the contrast-enhanced ultrasound (CEUS). CEUS is much more sensitive than basic ultrasound in depicting parenchymal injuries and in the evaluation of their extension. In fact, CEUS has sensitivity and specificity values very similar to those of CT, which is the gold standard. Furthermore, it can depict active bleeding as a negative prognostic factor even if in a less accurate way as to CT.
The examination, for which it is necessary to obtain the parents’ informed content, consists in the injection of US contrast medium, made up of a 2.4 ml suspension of phospholipid microbubbles of an inert gas (sulfur hexafluoride), through an antecubital vein followed by a bolus of 10 ml of physiological solution. Some specific elements are very important to carry out this procedure: to obtain the correct formation of microbubbles, the suspension should be shaken for at least 40 s and the injection should be done with at least an 18G needle; the use of smaller cannula needles, e.g., 20G, can destroy up to 20 % of the bubbles. After the injection, a rapid sequence exploration is done starting from the kidneys, then the liver, and ending with the spleen. The overall time needed is around 5 min (Fig. 4.1).
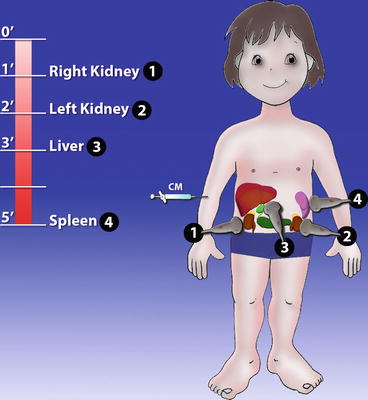
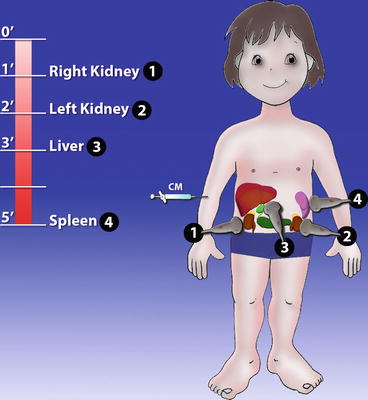
Fig. 4.1
CEUS protocol. CEUS exploration sequence: the kidneys, the liver, and finally the spleen
The US contrast medium elimination is rapid: after around 15 min, all the microbubbles break and the sulfur is eliminated through the lungs. US contrast medium has no nephrotoxic effect, and it is not metabolized by the kidney because it does not pass in the interstitial space, but it remains in the vessels.
Adverse reactions occur very rarely; severe reactions to the US contrast medium are not reported in pediatric patients in the literature.
At CEUS exam, the aspect of normal parenchyma is homogeneously hyperechoic; traumatic lesions appear as hypo-anechoic areas of different sizes and more or less defined, with or without capsular interruption, with morphology and extension corresponding to the CT exam.
The partial or total lack of enhancement of an organ is related to a vascular injury. The flow of contrast medium microbubbles out of the injured organ is due to extraparenchymal active bleeding. The presence of microbubbles in the damaged area can suggest intralesional blush.
It is possible and correct to administer a second dose of US contrast medium to solve any type of diagnostic doubt.
US and CEUS main benefits concern different aspects, as to its rapid performance, accuracy, and the possibility of avoiding unnecessary CT exams, thus reducing radio-exposure risks.
Besides the radioprotection aspects, US is ideal for pediatric use since a child has a higher quantity of water and a lower quantity of fat in his body as to an adult, so US imaging is of a higher quality in children than in adults.
CEUS limits are the same as those of basic US: the built of the patient, the presence of pneumoperitoneum, the presence of cutaneous wounds, and the evaluation of hemoretroperitoneum, together with the background experience knowledge and skills of the radiologist.
Furthermore, CEUS has specific limits in the evaluation of abdominal organs, in particular in depicting hollow viscera lesions, intestinal and mesenteric traumatic lesions, urinary tract injury, and the presence of active bleeding, as it has lower sensibility to the contrast-enhanced CT exam [6–9].
4.2.1 CT Technique
CT is the imaging method of choice in the evaluation of abdominal and pelvic injuries after blunt trauma in hemodynamically stable children.
In patients with major trauma, when the type of injury is not yet identified, it is best not to apply a specific-organ technique but a method which can show in detail any type of injury. CT scans are obtained from the lower chest to the pubic symphysis. Monitoring devices and metallic leads should be moved from the scanning plane because they will yield streak artifacts.
In traumatic young patients, after the scout view, it would be preferred not to perform the basal phase, in order to reduce radio-exposure.
Unenhanced CT scan, if instead performed, allows to highlight abdominal presence of free air, parenchymal or mesenteric hematoma, and bone fractures.
Imaging study with oral contrast medium administration is not recommended, due to the little advantage compared to the complexity of its administration in major trauma patients.
A 3-mm-thickness scan allows to perform good-quality imaging and subsequent good-quality reconstructions without excessive radiation exposure.
The intravenous iodine contrast medium volume depends on the patient’s weight (approximately 2 ml/kg).
The CT technique has two contrast-enhanced phases: an arterial phase which is extended to all the body, to depict vascular injury or active bleeding, and an abdominal portal phase, to evaluate parenchymal and hollow viscera injury.
In the suspect of urinary tract injury, if the patient’s clinical conditions are favorable, a later phase after 5 min is performed.
On the contrary, in case of suspected bladder injury, a retrograde distension with air may allow better visualization of the wall injury, especially in the anterior wall.
4.3 Physiopathology
The continuous growth of the developing pediatric patient’s body and the anatomical and structural differences with that of an adult are the main causes of the diversity of lesions and differences in the management between adult and child.
Whatever high-energy trauma occurs to a child, it is to be considered a potential cause of multiorgan lesions: this is why an equal impact force will determine a major impact area on a child due to the smaller body dimension compared to an adult.
A child reports less frequently bone fractures (e.g., ribs), due to a major flexibility in the bone structure of his body. This is why the absence of bone fractures does not imply a low-level energy impact, whereas the presence of bone fractures confirms a high-level energy trauma.
Besides, the protection provided by the lower ribs on abdominal parenchymal organs in the child is lower, both for the major flexibility of the ribs and for the relatively bigger dimension of the liver, spleen, and kidneys which protrude from the ribs, thus being directly exposed to the impact. The diaphragm muscle itself, which is in a more horizontal position, pushes down the liver and the spleen contributing in the protrusion from the ribs.
Other differences are the fact that the abdominal wall is thinner, due to the reduced muscle development, thus less adept in protecting in case of impact; there is less fat tissue in both subcutaneous abdominal tissue and in the intra-abdominal site, where it wraps parenchymal organs and all structures, partially absorbing the impact of the energy involved.
Ureters are wider and less tonic due to poor development of muscular tunic; the bladder is in a higher position because the pelvis is smaller and almost completely occupied by the rectus. Furthermore, the bladder which is intraperitoneal in the first years of life tends to descend in the pelvic area and to become retroperitoneal.
In the management of traumatic pediatric patient, nonoperative strategy is highly performed with respect to an adult patient, thus requesting surgery only if strictly needed.
Nonoperative management is ideal for pediatric patients as blood vessels are smaller with respect to an adult, and there is a major vasoconstrictive response, so visceral organ bleeding tends to be self-limited despite the severity of trauma.
At present, the choice of considering surgery is not strictly linked to the severity of the lesions or to the number of organs involved but to the capacity to normalize the hemodynamic condition despite all the pharmacological therapy in a maximum range of 6 h.
The liver, bowel, and spleen are highly vascularized organs within the peritoneal cavity, so there is a risk of a heavy bleeding. In all issues, active bleeding is a sign of severity and alarm, but still it does not mean that surgery is needed if hemodynamic values are normal.
Only bowel lesions always need surgery due to the high risk of bacterial contamination in the peritoneal cavity in case of traumatic perforation, not like parenchymal lesions.
As to the clinical outcome, we can say that in pediatric patients, hepatic lesions have a slower recovery as to spleen lesions, and multiorgan lesions have a slower recovery compared to isolated lesions.
4.4 Liver
Hepatic lesions are to be found in 10–30 % of blunt abdominal trauma; in many statistics, the liver is considered to be the organ which is mostly involved [12], both with isolated lesions and with lesions involving other organs, mainly the spleen. Lesions are often asymptomatic, and in 70 % of the cases, they can be treated in a nonoperative way. For anatomical reasons linked to coronary ligaments that hold the liver, the most exposed areas are the left lobe posterior segments which hit against the ribs and the dorsolumbar vertebral bodies.
Hepatic parenchymal lesions can extend and involve biliary ducts and blood vessels. Hemoperitoneum is present in around 2/3 of the cases and occurs if the lesion involves the organ capsule; if the capsule is saved, the hematoma will be intraparenchymal and/or subcapsular.
When the lesion involves the posterior surface of the liver which is not wrapped by the peritoneum, the so-called nude area, the blood expansion will occur in the retroperitoneal space. The consequent hemoretroperitoneum is usually located around the right adrenal gland and/or in the pararenal anterior space.
As in all organs, the most used classification of the severity range of hepatic lesions is that of the American Association for the Surgery of Trauma (AAST). This classification valid for both children and adults divides lesions in six categories, and it considers the type and extension of the parenchymal injury and the vascular involvement. Especially in pediatric patients, in whom the trauma management tends to be nonoperative, the grading of parenchymal lesion is not the main factor in deciding the type of treatment to be performed, surgical or conservative. Other elements such as the hemodynamic stability and the multiorgan involvement determine the choice of the management. The severity of the lesion will determine the hospitalization period and the restrictions to be adopted after hospital discharge.
A shorter classification according to the traumatic lesion extension divides hepatic lesions in: minor, in case of less than 25 % of parenchyma injured in the involved lobe or in case of the presence of subcapsular hematoma; moderate, in case of values between 25 and 50 % of the involved lobe; and major, in case of more than 50 % of the lobe involved or in case of bilobar involvement [13].
4.4.1 US–CEUS
The right hypochondrium location immediately below the diaphragm, rib cage, and the intestinal gas cause an even more difficult US evaluation of hepatic dome and of the lateral segments, especially in patients that do not collaborate in breathing and correct positioning.
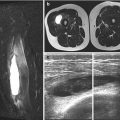
Even if in small amounts, the hemoperitoneum detection appears very clear, while hepatic lesion US evaluation, especially in the smallest lesions, can be difficult (Fig. 4.2).
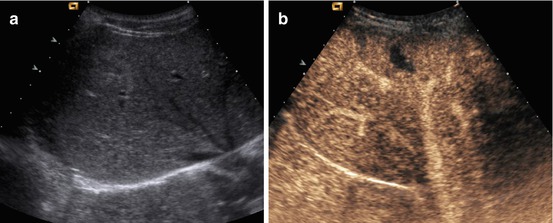
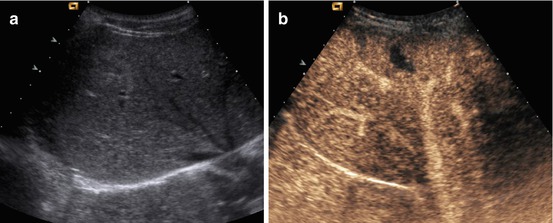
Fig. 4.2
A 10-year-old girl fell off the bicycle. Small hepatic tear. (a) US shows ill-defined hyperechoic area within VII hepatic segment. (b) CEUS well demonstrates a small anechoic laceration in the VII hepatic segment
Lesions can present different shapes, unclear borders, and iso-hyperechoic echostructure for the presence of fresh blood (Fig. 4.3). Subcapsular hematoma, as in CT, compresses the lateral margin of the hepatic parenchyma, and if very corpusculated, it can be difficult to differentiate from the normal parenchyma.
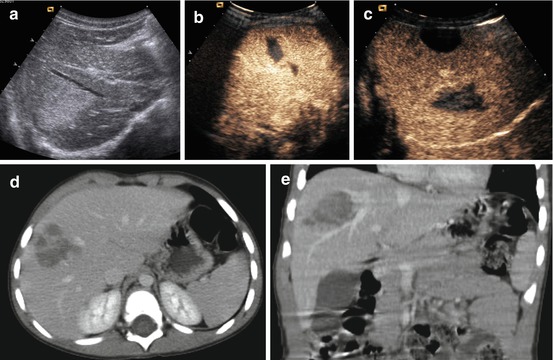
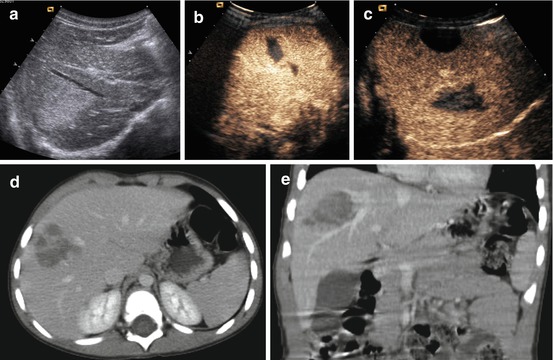
Fig. 4.3
A 4-year-old boy hit against a desk at school. Laceration with hematoma of the right hepatic lobe. (a) US, hyperechoic area in the right hepatic lobe. (b, c) CEUS, hypoechoic well-defined lesion. (d, e) Contrast-enhanced CT scan through upper abdomen shows irregular area with absence of contrast enhancement in the anterior segment of the right hepatic lobe. The images correspond to that of CEUS
With CEUS the lesion will appear as an avascular area, hypo-anechoic compared to the normal hyperechoic parenchyma. In some cases, it is possible to see the presence of hyperechoic spots due to active bleeding in the anechoic lesion (Fig. 4.4).
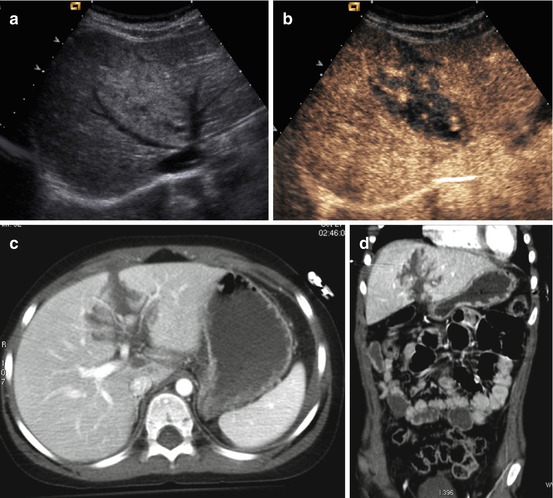
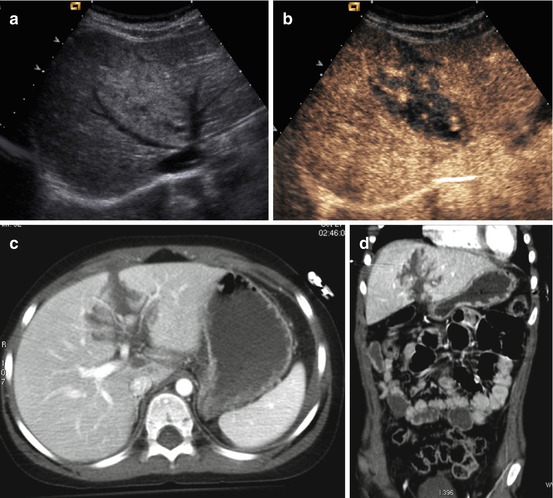
Fig. 4.4
A 14-year-old boy, sport trauma. Laceration of the IV hepatic segment with active bleeding. (a) US shows large hyperechoic area in the IV hepatic segment. (b) CEUS, hypoechoic lesion with hyperechoic spots suggestive of active bleeding. (c, d) Contrast-enhanced CT scan through upper abdomen shows irregular laceration with internal blush of contrast medium according to active bleeding
In US follow-up, the size of the lesion will decrease, changing the echostructure from iso-hyperechoic to anechoic in time; even the hematomas will show the same echostructural changes together with the decrease in the size until the disappearance of the hematoma itself. With CEUS, the avascular area will show a progressive reduction in size and well-defined margins [6, 7, 9].
4.4.2 CT
The most frequent lesion is the parenchymal laceration. Contrast-enhanced CT shows a hypodense area, with a variable shape (Figs. 4.5 and 4.6). When the laceration reaches the capsular surface of the liver and breaks the Glissonian capsule, the hemoperitoneum always occurs; this is depictable through unenhanced CT scans, when performed immediately after trauma, as a high-density fluid, around 40 UH.
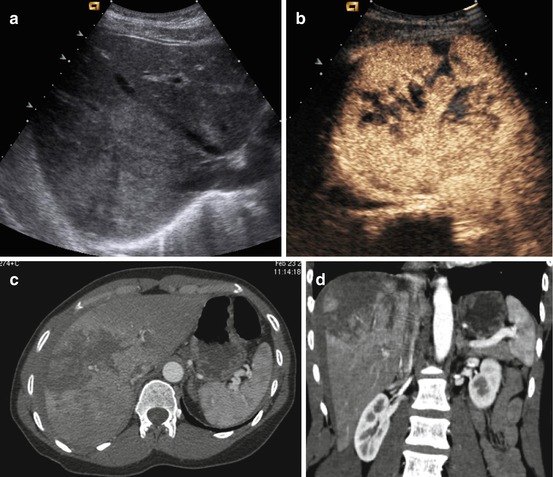
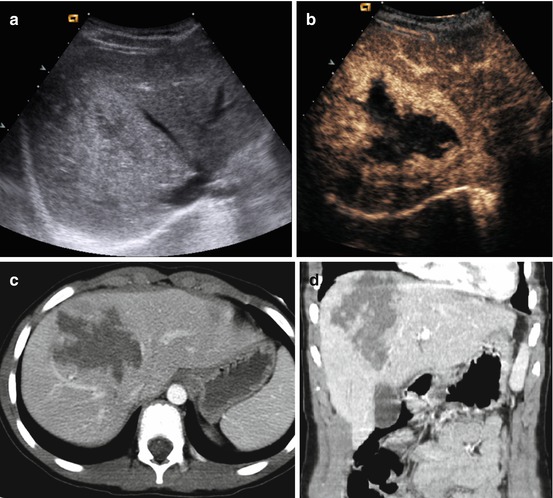
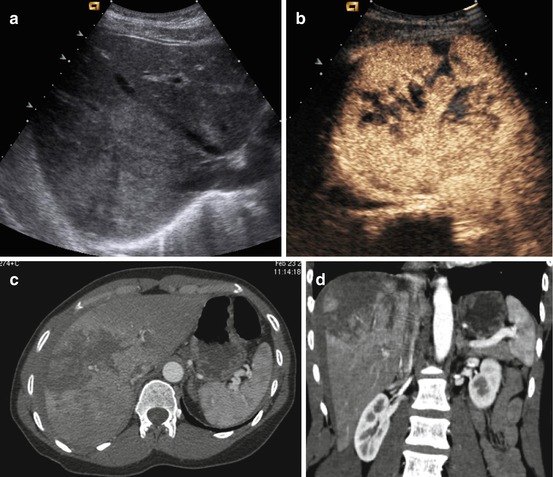
Fig. 4.5
A 17-year-old young girl. Trauma from falling off a horse during horse race. Ill-defined laceration of the liver. (a) US, irregular hyperechoic area in the right lobe. (b) CEUS shows multiple anechoic lacerations in the right hepatic lobe. (c, d) Contrast-enhanced CT confirms the presence of huge lacerations with irregular shape
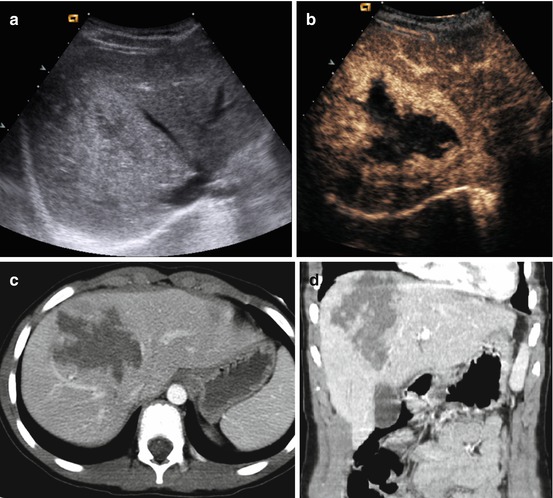
Fig. 4.6
A 9-year-old boy kicked by a horse. Laceration with hematoma of the right hepatic lobe. (a) US shows inhomogeneous hyperechoic area in the right hepatic lobe. (b) CEUS well defines the size and shape of the lesion, showing a large hypoechoic area. (c, d) Contrast-enhanced CT scan through upper abdomen shows irregular area with absence of contrast enhancement in the anterior segment of the right hepatic lobe, corresponding to that of CEUS
When the laceration does not reach the Glissonian capsule, hematoma occurs; it can be intraparenchymal and/or subcapsular. When intraparenchymal hematoma occurs, it is possible to depict it in basal phase CT, as a fuzzy hyperdense zone in the hepatic parenchyma, due to recent bleeding; after intravenous contrast medium administration, hematoma will appear hypodense compared to the normal enhanced parenchyma. Subcapsular hematoma typically compresses the lateral margin of the hepatic parenchyma, thus allowing an easier differential diagnosis compared to the perihepatic fluid (Fig. 4.7).
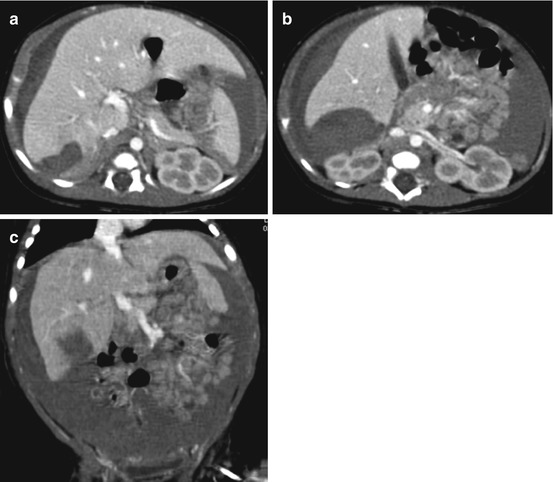
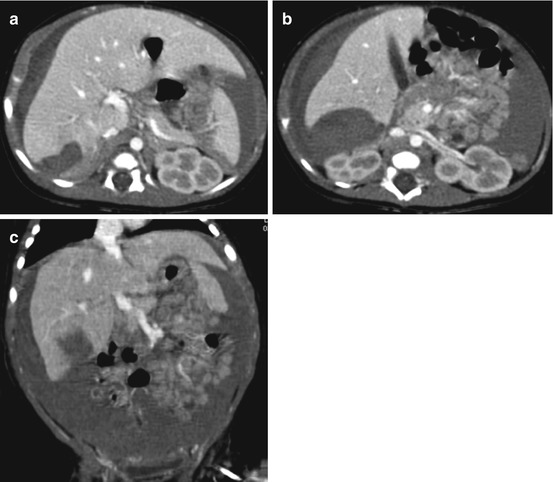
Fig. 4.7
Newborn with laceration and subcapsular hematoma of the liver. (a–c) Contrast-enhanced CT scan through upper abdomen shows laceration of the liver with associated subcapsular hematoma and large amount of hemoperitoneum
To carry out a prognostic evaluation, it is important to search for active bleeding in the hepatic lesion or in the hematoma, which appears as arterial phase contrast medium blush, eventually followed by a pooling in later phases (Fig. 4.8).
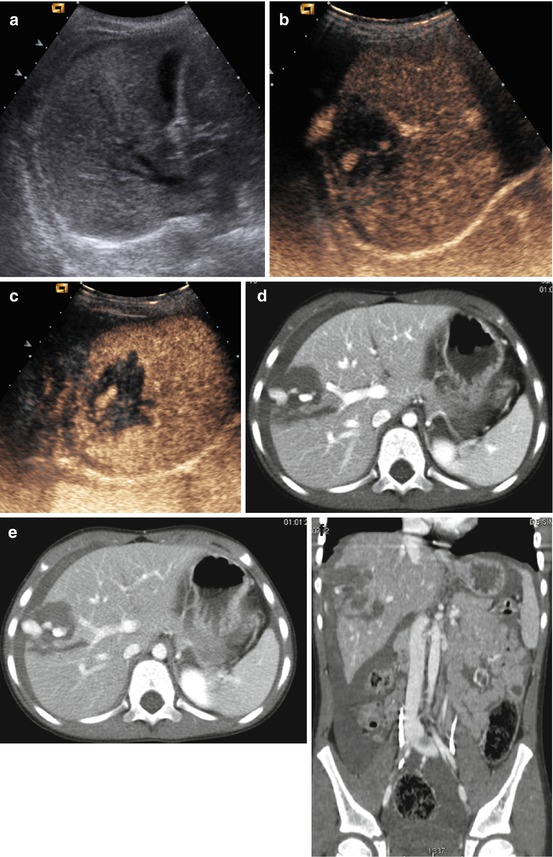
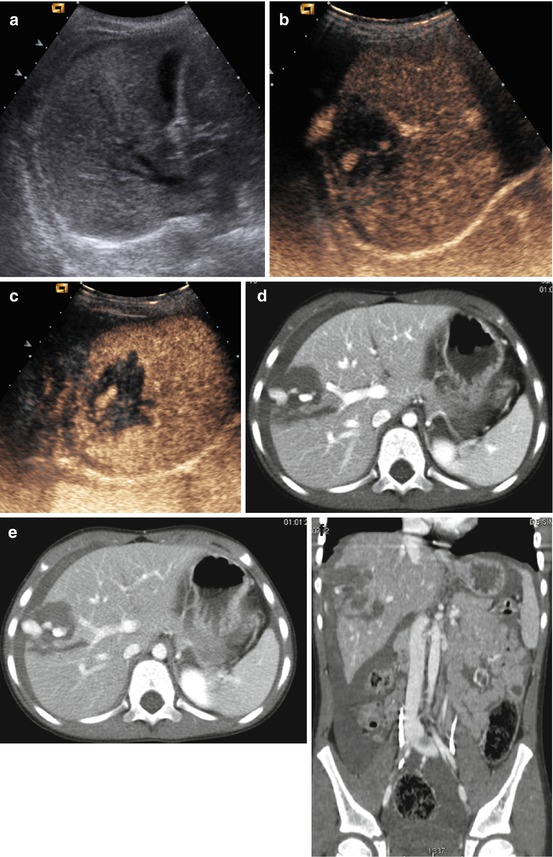
Fig. 4.8
A 6-year-old boy fell beating the right flank. Laceration of right the hepatic lobe with active bleeding. (a) US shows fuzzy hyperechoic area in the right hepatic lobe. (b, c) CEUS demonstrates hypoechoic lesion with hyperechoic large spots, both intralesional and extracapsular, due to active bleeding. (d, e) Contrast-enhanced CT scan through upper abdomen shows irregular tear with internal and extracapsular blush suggestive of active bleeding. Mild amount of hemoperitoneum is appreciable
Traumatic hepatic vascular lesions are rare in pediatric patients. Avascular segments will appear hypodense after intravenous contrast medium administration. When post-traumatic hepatic artery pseudoaneurysm is seen through CT as hyperdense focus in the arterial phase within hepatic laceration, it is necessary to stress the issue and suggest the correct management through emergency embolization, even in the case of hemodynamic stability, as there is a high risk of rupture (around 80 %) [14].
The significance of periportal low hypodensity zones has been a matter of discussion; they have been considered a specific sign of hepatic trauma in the past. In fact, this issue is not only appreciable in traumatic lesions, and it seems to be linked not only to a specific organ lesion but to an overflow in lymphatic vessels in periportal spaces, due to a sudden increase in central venous pressure caused by too much fluid provided during the rescue phase.
During the follow-up, lesions treated nonoperatively after 1 month appear hypodense, due to reabsorbing of the corpusculated component; they gradually reduce their volume, usually to complete resolution, eventually leaving a small parenchymal cyst or a calcification.
It has been verified that usually minor and moderate lesions heal completely in 3–6 months while major lesions can remain even after 8–15 months. Subcapsular hematoma heals in around 2 months [13].
Complications in hepatic trauma are rare, they usually occur in the first month, and the clinical symptoms are fever, hypotension, peritonitis, etc. Other complications can be the abscessualization of the lesion in the first weeks, biloma that occurs between 12 days and 6 weeks (Fig. 4.9), hepatic artery pseudoaneurysm, subcapsular hepatic hematoma due to late bleeding, and choleperitoneum.
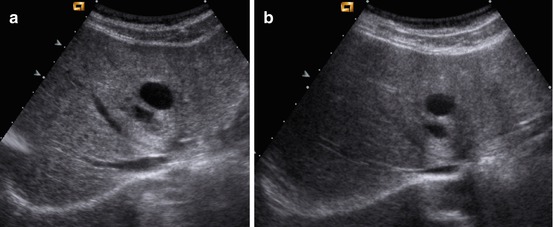
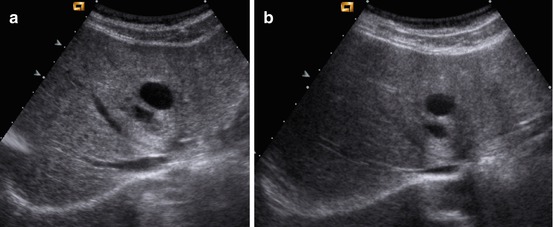
Fig. 4.9
Same patient of Fig. 4.4. Follow-up of hepatic laceration. Biloma. (a) US performed 1 month after trauma shows two fluid collections in the IV hepatic segments. (b) Follow-up US performed 3 months later shows the persistence of the rounded fluid collections, which appear to be related to bilomas
4.5 Spleen
The spleen is an intraperitoneal organ located in the abdominal left upper quadrant. It is the most vascularized organ of the body, in fact around 350 l of blood flow through it every day; this is why its injury is a potential risk for life, exposing the patient to a massive hemoperitoneum. While in adults the spleen is partially protected by the rib cage, in children, it is bigger, and for this reason, it protrudes and it is often involved in blunt abdominal trauma, with a frequency of 25 % of the cases both as isolated lesion and as multiorgan lesions.
The spleen is an important organ for the development and correct functioning of the immune system, especially in pediatric patients. Therefore, it is particularly important to perform the conservative treatment in traumatic splenic lesions [15–17].
Imaging plays a fundamental role in differentiating the minor trauma, in which the observation of the patient is allowed, from those complex traumas which request immediate surgery.
Even for splenic lesions, as for hepatic lesions, the most used injury severity classification is that of AAST. As already said for the liver, this classification is not directly linked to the need of an operative management. In fact, if the patient is hemodynamically stable, despite hemoperitoneum or self-limited bleeding, the conservative management of the patient is recommended, considering its advantages, both because the immune function of the organ is preserved and because early and late complications caused by surgery are prevented, shortening hospitalization. Hemodynamic instability or the possibility of its happening is the main factor to perform splenectomy.
Splenic injuries have different shapes, linear or branched or complex; they can be associated to the presence of hemoperitoneum, in case of splenic capsula rupture, or to subcapsular or intraparenchymal hematoma, if the capsula is undamaged, around 25 % of cases [18].
Hemoperitoneum linked to capsular lesion is most frequent when the hilum region is involved; furthermore, in this case, blood will flow along the splenorenal ligament at first, but then it will reach the retroperitoneum zone, in the anterior left pararenal space and around the pancreatic tail.
Two-time rupture of the spleen occurs rarely in adults, around 6 % of cases, and it is less frequent in children. It is a poor clinical evolution of an unknown subcapsular hematoma or of a vascular lesion as arterial-venous fistula or pseudoaneurysm. Even the late rupture can be treated with a conservative method, following the same criteria already mentioned for acute rupture. There are no links between late rupture and the insufficient rest of the patient. Bed rest is necessary only until abdominal pain is reported, and then a 3-month period of limited physical activity is suggested before going back to a normal lifestyle.
The recovery of the organ is strictly related to the severity of the lesions, and it can range from 3 to 20 weeks for a shattered spleen. The conservative management, even if partial, is very important in the preservation of the immunological function of the spleen; studies carried out on adults have shown that immunological function is preserved if at least 1/3 of the parenchyma is saved.
Literature states that minor lesions (I and II level) can be considered self-healing and patients can leave the hospital just after a 1-day bed rest and start their normal daily functions except sports activity, which can be started again after 6 weeks.
In major trauma, hospitalization and bed rest can be 2–3 days; after, hemodynamically stable patient without pain can be discharged and must follow the above protocol. The patient will undergo a 6–10-week follow-up according to the severity of the lesion [19].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree