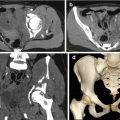
Fig. 2.1
The axial head-MDCT with bone window shows a depressed fracture of the right frontoparietal bone
They are more common patterns in nonaccidental cranial trauma, and each of these collections should be specified [30, 31].
2.3.1 Epidural Haematoma
Epidural haematoma (EDH) is secondary to the laceration of meningeal vessels (arteries or veins), diploic veins or dural sinuses in head injuries [32].
Blood extravasates into the virtual epidural space between the inner tabula of the skull and the dura mater. In 90 % of cases, a skull fracture can be associated with it. EDH can be of arterial or venous origin. The arterial one comes out from middle meningeal artery laceration, while the venous one results from dural sinus laceration or diploic veins, and it is more frequent in posterior fossa injury adjacent to the dural sinus especially when a fracture transverses the involved dural sinus. Arterial EDH is typical in older children, while venous EDH is more frequently seen among younger children [32].
On CT, a biconvex-shaped hyperdense finding is the typical pattern of acute EDH due to the pulling away of the dura mater, attached to the skull, by the haematoma (Figs. 2.2, 2.3 and 2.4).
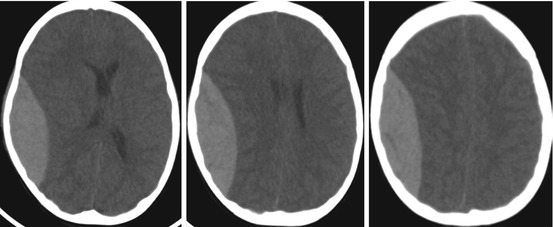
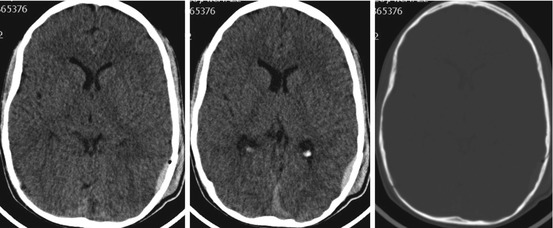
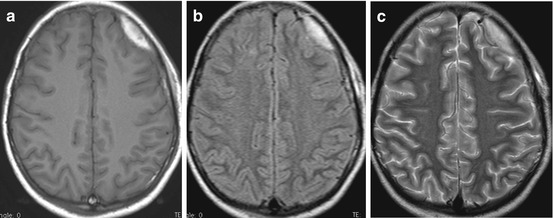
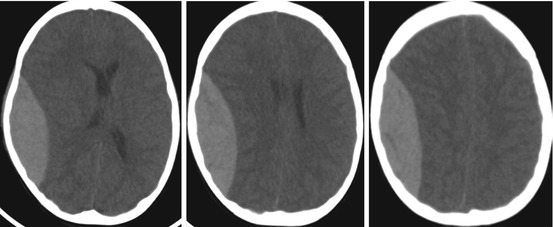
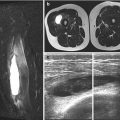
Fig. 2.2
The axial head-MDCT shows a biconvex-shaped hyperdense pattern at the right frontoparietal region as a typical pattern of acute EDH
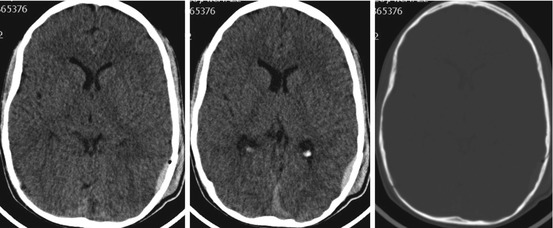
Fig. 2.3
The axial head-MDCT shows a thin biconvex-shaped hyperdense EDH at the left parietal region associated with simple linear fracture of the adjacent bone
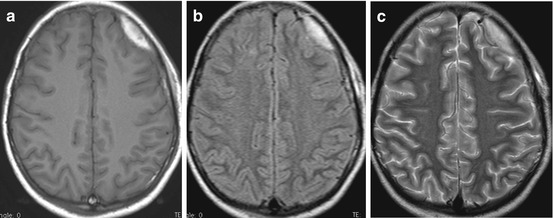
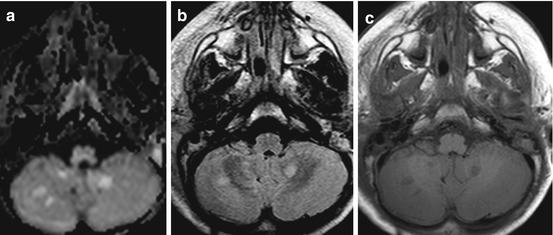
Fig. 2.4
(a–c) The MRI shows a left frontal EDH, hyperintense signal on T1W-MRI (a), FLAIR (b), T2W (c) as EDH with extracellular maetaemoglombin signal
Generally, it does not cross the cranial sutures because the periosteal layer of the dura is tightly adherent to the cranial sutures. This sign is used to distinguish EDH from SDH on CT or MRI. By a retrospective data analysis, Huismann [32] showed that in 11 % of children, EDH can cross the cranial sutures especially when fractures involve cranial sutures or when there is a post-traumatic cranial suture diastasis.
Retroclival epidural haematoma may be associated with ligamentous injury, which may further result in instability at the craniocervical junction [33].
2.3.2 Subdural Haematoma
Subdural haematoma (SDH) is an extracerebral haemorrhage secondary to torn cortical vein or sinus in head injuries. Blood extravasates into the ‘subdural space’ which is a potential space that can be opened by the separation of the arachnoid mater from the dura mater as a result of trauma.
Acute (1–5 days) haematomas appear hyperdense (relative to grey matter), whereas subacute (approximately 7–20 days) haematomas appear isodense and chronic (older than 20 days) haematomas hypodense [30].
Accurate timing of a haematoma is not possible after 1 week. The use of intravenous contrast has been recommended to confirm the chronicity of the subdural haematoma by demonstrating the presence of an inner membrane delineating the haematoma [34].
The subdural membrane may be seen after 7 days. A mixed high- and low-density subdural haematoma, representing a chronic haematoma with re-haemorrhage, is considered as a nonaccidental cranial trauma in children (child abuse) [30].
A small extra-axial haematoma or fluid collection can be missed on CT; therefore, MRI is always indicated for detection, thanks to its higher anatomical resolution and multiplanar capability. On MRI, SDH patterns follow the pattern of the evolution of intraparenchymal haematomas in terms of time course. In the acute phase (1–3 days), the signal intensity alteration is a low signal on T1 and on T2. In the early (3–7 days) subacute phase, the haematoma returns a high signal on T1 and a low signal on T2. In the late subacute (7–21 days) phase, the haematoma returns a high signal on T1 and on T2. In the chronic stage, subdural haematomas may mimic a hygroma by returning a signal similar to that of cerebrospinal fluid on T1 and T2.
A retroclival subdural haematoma may indicate a sentinel event for traumatic injury elsewhere within the brain or posterior fossa [33].
2.3.3 Traumatic Subarachnoid Haemorrhage
Traumatic subarachnoid haemorrhage (tSAH) is defined as a haemorrhage into the subarachnoid space, and it is considered as a marker of severe TBI with adverse outcome [35].
TSAH is caused by the traumatic rupture of small vessels in the pia-arachnoid when the brain is moved under the dura mater by external force during injuries or by haemorrhage associated with cortical contusions. TSAH in the basal subarachnoid cisterns has been considered to indirectly indicate primary brainstem injury in many patients [36].
On CT, the TSAH pattern is a spontaneous hyperdensity into the subarachnoid space or into the basal subarachnoid or sellar cisterns and Sylvian fissures. The degree of TSAH could be classified into three grades according to the density on CT scans: mild, with a faint layer of blood; moderate, with a thin layer of blood; and massive, with a thick layer of blood.
A small amount of blood into the subarachnoid space could be missed on CT scan, but using MRI with FLAIR sequence can detect TSAH [37].
Analysis of the detection of haemorrhagic localizations shows an accuracy, sensitivity and specificity of 89, 82 and 92 % using CT and 90, 83 and 94 % using MRI, respectively. MRI was more sensitive than CT in the detection of subarachnoid haemorrhagic localizations, whereas no significant difference resulted from the detection of epidural and subdural haemorrhagic findings [37].
2.3.4 Brain Oedema
Brain oedema (BO) is a bad prognostic sign and usually results in cerebral dysfunction. It can be reversible as long as there is no brain shift or vessel occlusion or can lead to ischaemia.
There are two typical findings for BO: the ‘reversal sign’ and the ‘white cerebellum sign’.
The ‘reversal sign’ is the diffuse loss of grey–white matter differentiation with decreased attenuation of the cortex. The basal ganglia, cerebellum, thalami and brainstem are relatively spared and may therefore appear relatively bright [38, 39].
The ‘white cerebellum sign’ reflects the loss of differentiation between cerebral grey and white matter with a loss of density and the sparing of brainstem and cerebellum which may look hyperdense. Often this can also reflect an extracranial nonaccidental cause of hypoxia such as strangling or suffocation [38, 39].
2.3.5 Diffuse Axonal Injury
Shear brain injury or more commonly known as diffuse axonal injury (DAI) is diagnosed in children with TBI due to high-impact accident. It is one of the most common and important pathologic features of traumatic brain injury. The susceptibility of axons to mechanical injury appears to be due to both their viscoelastic properties and their high organization in white matter tracts. Although axons are supple under normal conditions, they become brittle when exposed to rapid deformations associated with brain trauma. Accordingly, the rapid stretch of axons can damage the axonal cytoskeleton resulting in a loss of elasticity and impairment of axoplasmic transport. Subsequent swelling of the axon occurs in discrete bulb formations or in elongated varicosities that accumulate transported proteins. Calcium entry into damaged axons is thought to initiate further damage by the activation of proteases. Ultimately, swollen axons may become disconnected and contribute to additional neuropathologic changes in brain tissue. DAI may largely account for the clinical manifestations of brain trauma. However, DAI is extremely difficult to detect noninvasively and is poorly defined as clinical syndrome [40].
DAI is a diagnosis of exclusion whereby the patient who came with a definite history of trauma has a low GCS at presentation but yet a ‘normal’ brain CT or just multiple small punctate haemorrhages. MRI is a more reliable modality to detect this type of axonal damage instead of CT that is often negative for lesions [41].
DAI can be distinguished in non-haemorrhagic or haemorrhagic lesions.
Non-haemorrhagic ones can be depicted on FLAIR and diffusion-weighted sequences as a small parenchymal subcortical hyperintensity alteration [42] (Fig. 2.5).