Etiology
%
Motor vehicle accidents
38.2
Homicide
13.3
Drowning
13.2
Burn
9.1
Suicide
5.4
Suffocation
4.5
Other
16.3
In children, the area more frequently affected by trauma is the skull [7, 8], then the associated thoracic–abdominal injuries [1–3, 7, 8]. Since multiple injuries are common among children, the emergency physician has to assess all the organs of an injured child, independent of the real mechanism of the trauma.
Even if the principles of polytrauma management are identical both in children and in adults, the optimal pediatric patient care requires a specific understanding of some important anatomical, physiological, and psychological differences that play a significant role in the assessment and management of a pediatric patient [9]. A comprehensive outline of the anatomical differences and of their implications in a polytrauma patient is listed in Table 1.2.
Table 1.2
Anatomic differences in adults and children and implications for pediatric trauma management
The child’s body size allows for a greater distribution of traumatic injuries; therefore, multiple trauma is common |
The child’s greater relative body surface area also causes greater heat loss |
The child’s internal organs are more susceptible to injury based on more anterior placement of the liver and spleen and less protective musculature and subcutaneous tissue mass |
The child’s kidney is less well protected and more mobile, making it very susceptible to deceleration injury |
The pancreas is less protected by the abdominal muscles and fat and is therefore more susceptible to injury from impact against the spine |
The child’s head-to-body ratio is greater, the brain less myelinated, and cranial bones thinner, resulting in more serious head injury |
In general, the body of a child has higher elasticity, so that even severe internal injuries may occur without any recognizable external signs. Children are particularly at risk of severe injuries since, proportionally to weight–height ratio, they have bigger and more adjacent solid organs, less subcutaneous fat, and less muscular protection than adults.
Besides, in relation to the adverse ratio head–body and the larger body surface in relation to weight, each force will be more widely distributed making the most significant probability that multiple lesions may occur. The imbalance between the large body surface and the weight leads the child to a greater amount of heat loss in relation to a higher evaporation.
All these factors prove that the energy level and the caloric requirement of a polytrauma child are much larger than that of an adult. Physiologically, each child responds to the trauma in a different way depending on the age and severity of the injury, but each procedure relative to free water and electrolyte maintenance is to be amplified.
Unlike adults, children have a great ability to maintain their blood pressure despite a significant and acute blood loss (from 25 to 30 %). Small changes in heart rate, arterial pressure, and perfusion of the extremities may indicate an imminent presentation of cardiorespiratory failure and, therefore, should not be neglected. Finally, children do not have the ability to better manage an environment that is not their usual, and, for this reason, they are excessively irritable, making their health status assessment even more difficult.
Recent data have shown that 25 % of children involved in road accidents will show signs of post-traumatic stress disorder following the discharge [10]. The pediatric patient needs a calm, sometimes unconventional, approach in such a way as to reduce their state of anxiety.
1.2 Primary Survey
The primary objective of management of a young trauma patient is to identify and address immediate life-threatening injuries.
The initial assessment and the arrangement of possible resuscitation procedures can and should be rapid (5–10 min); it is convenient to follow the logical sequence A–B–C–D–E (airway–breathing–circulation–disability–exposure), remembering that an airway obstruction is potentially deadly faster than a respiratory problem which, in turn, can turn fatal faster than a circulatory problem, etc. (Fig. 1.1).
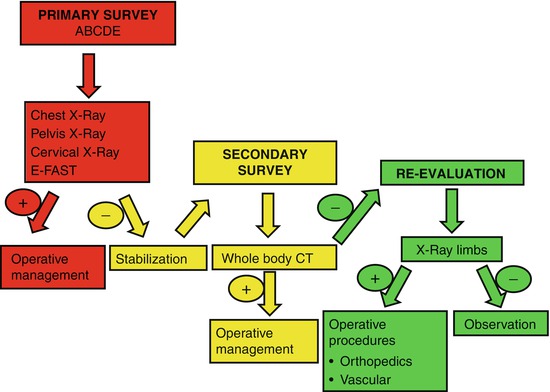
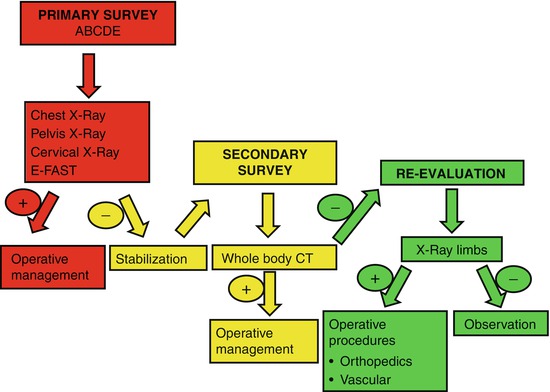
Fig. 1.1
Flow chart
1.2.1 Airway: Airway and Cervical Spine Protection
Ensuring airway patency is the first essential step for the resuscitation of polytrauma children: in fact, an acute airway obstruction is the leading cause of death in pediatric trauma.
Clinical signs of partial or complete airway obstruction are, for example, stridor, dysphonia, wheezes, high or too low respiratory rate, but also – indirectly – altered state of consciousness (restlessness, stupor, coma).
The first fundamental maneuver of the opening of the airway is the jaw-thrust maneuver which allows to maintain the alignment of the cervical spine; at the same time, high oxygen concentration should be administered immediately and a cervical collar should be placed. In children, the dimensional proportion between the head and body, with the typical prominent occiput, requires almost always to raise slightly the trunk in order to allow the cervical spine to stay in-line.
The airway patency may be impaired by the hypotonia of the tongue, hypopharyngeal muscles, as well as by secretions, blood, vomit, foreign bodies, and direct injuries of the facial bones/skull or of the airways.
The final maneuver of “stabilization” of the airway is represented by tracheal intubation to be performed only by skilled care providers.
Basic indications for tracheal intubation are:
Airway protection from aspiration of blood and vomitus
Airway obstruction or risk of obstruction due to trauma and burns of the face and/or of the neck
Insufficient oxygenation despite a high Fi02
Shock
Severe impairment of the levels of consciousness (GCS <9)
1.2.2 Breathing: Ventilation and Oxygenation
A consequential step immediately following the verification and obtainment of a patent airway is monitoring the effectiveness of respiration – spontaneous ventilation.
An efficient respiratory activity depends on the anatomical integrity of the rib cage and the pulmonary parenchyma, in addition, of course, to an efficient neural drive.
As in adult patients, it is absolutely necessary to seek and rule out clinically life-threatening conditions such as tension pneumothorax and open pneumothorax, using the classic cornerstones of physical examination: inspection, palpation, auscultation, respiratory rate observation, and Sp02.
Tension pneumothorax still represents a dangerous and unrecognized “killer,” responsible for many preventable trauma deaths.
In children and even more in infants, any impairment in diaphragmatic excursion may significantly decrease ventilation. This occurs, for example, in the presence of gastric dilatation due to air ingestion (crying) or involuntary insufflations during ventilation with mask. Therefore, it is always convenient to take into account the decompression of the stomach using a G-tube.
In presence of severe impairment, ventilation is to be assisted with bag-valve mask (BVM) unit or tracheal intubation.
1.2.3 Circulation: Circulation and Hemorrhage Control
Assessment of the pediatric trauma patient’s circulation must take into account the peculiar stress and hypovolemia response; thanks to a significant release of catecholamine, the trauma child can compensate for blood loss increasing the heart rate and the systemic resistance; as a result, differently than adults, arterial hypotension is a late sign of shock and it often leads to imminent cardiac arrest.
Assessment of trauma child’s cardiovascular status is to be based on a combination of parameters, such as consciousness level, skin appearance (paleness, sweating, mottled skin), capillary refill time (normal <2 s), decrease of peripheral pulse rate compared with the central one, and dieresis (as soon as possible).
The lower arterial blood pressure values, considered acceptable in relation to age, are [11]:
Newborns, from 0 to 28 days old: 60 mmHg
Infants, from 1 to 12 months old: 70 mmHg
Children, from 1 to 10 years old: 70 mmHg + (2 mmHg per each year)
It is always required to identify the presence of any source of external bleeding with a systemic approach, by applying direct pressure; in children, in particular, the bleeding from the skull can be very massive and hemodynamically significant; in the presence of uncontrolled bleeding from the limbs, it required the immediate use of pneumatic tourniquets of proper fit.
All the polytrauma pediatric patients should be connected to a multiparameter monitor in order to have a continuous reassessment of the respiratory and circulatory parameters.
It is essential to obtain, as soon as possible, one or, preferably, two vascular access for the replacement of fluids and the delivery of medications. When a vascular access is unavailable within few minutes, it is suggested the installation of an intra-bone passage in the tibial, femoral, or humeral site (Fig. 1.2) [12].
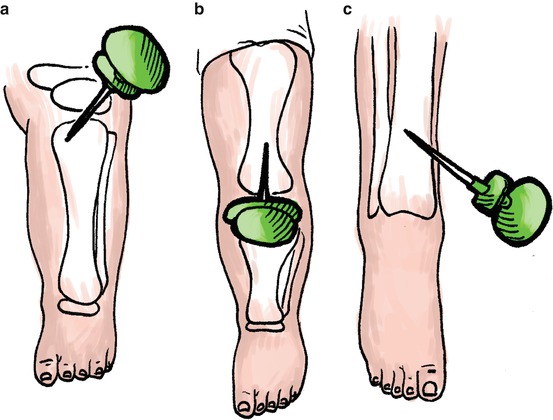
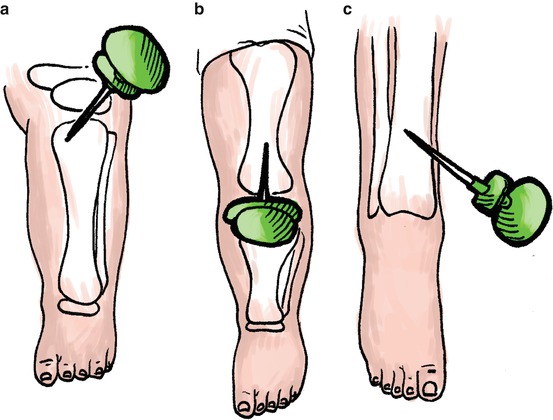
Fig. 1.2
Intra-osseous vascular access (a) Proximal tibiae site, (b) Femoral site, (c) Distal tibial site
In case of hypovolemic shock in a pediatric patient, the infusion plan involves the administration of a rapid 20 ml/kg bolus of crystalloids that can be repeated up to three times to a total of 60 ml/kg. If hemodynamic stability is not achieved, then further 10 ml/kg bolus of red blood cell concentrate is to be given. As in adults, also in children, the administration of colloids is highly controversial.
It is beyond the present study a detailed survey of the infusion strategies and the relative clinical target in different traumatic situations (head trauma and/or closed and/or penetrating trauma). However, it is important to remember that a careless volemic expansion, above all if performed without heating the fluids, can cause harmful coagulation impairment, from hemodilution and hypothermia.
As in adults, a shock condition in trauma children is to be attributed to hemorrhage, until proven otherwise; in relation to the context, of course, different and concurrent causes should be assessed, such as myocardial dysfunction after contusion due to thoracic trauma or medullary impairment with neurogenic shock (hypotension without increase of heart rate or vasoconstriction) due to head and neck injuries.
1.2.4 Disability: Neurological Assessment
Primary survey is to be completed assessing level of consciousness, papillary size and reaction, and possible lateralizing signs.
The level of consciousness can be examined using the Glasgow Coma Scale (GCS) (Table 1.3) or the simplest score AVPU (Table 1.4).
Table 1.3
Glasgow Coma Scale
Eyes (1–4 points) | Verbal (1–5 points) | Motor (1–6 points) |
|---|---|---|
4. Opens eyes by himself | 5. Oriented (normal) | 6. Obeys commands |
3. Opens eyes in response to voice | 4. Confused (disoriented) | 5. Localizes pain |
2. Opens eyes in response to pain | 3. Says inappropriate words | 4. Withdraws from painful stimulus |
1. Does not open eyes | 2. Makes meaningless sounds | 3. Decorticate posturing with painful stimulus |
1. Makes no sounds | 2. Decerebrate posturing with painful stimulus | |
1. Makes no movements |
Table 1.4
AVPU system
A = alert |
V = response to verbal stimuli |
P = responds to painful stimuli |
U = unresponsive |
A modified version of the GCS, the Pediatric Coma Scale (PCS) (Table 1.5), has been studied for preschool children.
Table 1.5
Pediatric Coma Scale (PCS)
Eyes (1–4 points) | Verbal (1–5 points) | Motor (1–6 points) |
|---|---|---|
4. Opens eyes spontaneously | 5. Coos and or babbles | 6. Infant moves spontaneously or purposefully |
3. Opens eyes in response to speech | 4. Cries but consolable, inappropriate interactions | 5. Infant withdraws from touch |
2. Opens eyes in response to painful stimuli | 3. Inconsistently inconsolable, moaning | 4. Infant withdraws from pain |
1. Does not open eyes | 2. Inconsolable, agitated | 3. Abnormal flexion to pain for an infant (decorticate response) |
1. No verbal response | 2. Extension to pain (decerebrate response) | |
1. No motor response |
Among the causes of neurological alterations in a pediatric trauma patient, it is necessary to consider a possible reduced intake of O2 (respiratory or cardiocirculatory causes) and hypoglycemia (easily exhaustible glycogen stores).
1.2.5 Exposure: Exposure and Thermal Protection
In the last stage of the primary survey, the trauma patient should be completely undressed (rapid external examination) and soon after protected from the risk of thermal dispersion (convective warming system, isothermal blanket).
1.3 Secondary Survey
The secondary survey is the phase of assessment and definitive treatment of the trauma patient.
It is undertaken only after the primary survey has been completed, in condition of total stability of the vital parameters.
It is necessary to act with order, from head to toe.
1.3.1 The Role of Radiology in the Management of Pediatric Polytrauma
Emergency radiology plays a crucial and vital role for the diagnostic iter of a polytrauma child, but it cannot take the place of a detailed history and a thorough physical examination.
Several imaging techniques are available, each one with its own advantages and its limits (Table 1.6), and the radiologist must be prepared to promptly decide which method to use so as to collect a lot of useful information for physicians and surgeons to develop an appropriate treatment and/or surgical plan.
Imaging modality | Advantages | Disadvantages |
|---|---|---|
X-ray | Very accessible | 2D images |
Rapid | Artifact from superimposed structures | |
Low cost | Limited use for soft tissues | |
Ionizing radiation (negligible dose) | ||
Ultrasound | Generally accessible | Operator dependence |
No ionizing radiation | Limited by body habitus | |
Low cost | Potentially painful | |
Dynamic image capture | Inconclusive results | |
Procedural guidance | ||
Bedside test | ||
Computed tomography | Generally accessible | Ionizing radiation |
Rapid | Contrast-induced nephropathy | |
High specificity/sensitivity | Intermediate cost | |
3D images | Contrast allergy | |
Magnetic resonance | No ionizing radiation | High cost |
High sensitivity/specificity | Limited availability | |
No contrast nephropathy | Long study duration | |
May require sedation for children or cause claustrophobia |
Radiological examinations may determine waste of valuable time in the polytrauma management. For this reason, in emergency management, the sensitivity of a radiological investigation is more important than its specificity, with the major aim of excluding any morbid conditions which would require a prompt curative treatment.
In the diagnostic evaluation of a polytrauma patient, the path to follow is completely different depending on whether the patient is in clinical condition of hemodynamic stability or instability.
As a matter of fact, in hemodynamically stable patients or in patients stabilized after primary resuscitation, a whole-body CT scan can be performed for a thorough and detailed exam of all the body parts, both visceral and somatic; on the contrary, in hemodynamically unstable patients, CT scan cannot be performed due to lack of time, and, therefore, lifesaving radiological and ultrasound investigations should have been already performed in the emergency setting, during the primary survey stage [13].
Upon arrival of polytrauma patients at the emergency setting, the radiologist plays a key role in the primary survey, and in this scenario, radiological and ultrasound examinations play a definite role, capable of providing a first effective diagnostic confirmation of some potentially life-threatening clinical situations.
Imaging tests to be performed during this stage are chest X-ray on AP view, cervical spine X-ray on LL view, pelvis X-ray on AP view, and E-FAST scan (extended focused assessment with sonography for trauma) with the patient lying in a supine position while the resuscitators try to monitor and stabilize the pediatric patient’s vital signs. The whole-body CT, as already said, on the contrary, a diagnostic aid of the secondary survey, is performed only after the achievement of the hemodynamic stability so as to meet a detailed and complete evaluation of all the body.
This chapter, therefore, will treat in detail only those semiotic elements relating to the investigations with diagnostic aids of the primary survey stage; the technique of whole-body CT scan will be only mentioned. The CT semiotic elements of the injuries of each organ and the whole body will be treated separately in the other specific chapters.
1.3.1.1 Chest X-Ray (CXR)
The CXR study on AP view, at bedside, of the polytrauma patient in the emergency room can be performed in the primary survey of an unstable trauma patient, in the presence of:
(a)
Respiratory failure (hypoxemia, dyspnea)
(b)
Hemodynamic instability
(c)




After pleural decompression or pleural drainage insertion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree