Transabdominal Ultrasound
Overview of transabdominal ultrasound
Ultrasound provides a unique role in evaluating internal anatomy. The ability to visualize cross-sectional and sagittal anatomy and to clearly differentiate cystic structures from solid masses makes it a critical tool in assessing the pathologic changes in the abdomen prior to operative intervention. Ultrasonography is a safe, portable, and noninvasive technique without deleterious side effects.
Diagnostic ultrasound uses repetitive pulses of sound with high frequencies, which penetrate soft tissues once they are concentrated into a narrow, focused column. As these waves traverse the abdomen, they are partially reflected at tissue interfaces. The sectional anatomy that is displayed needs to be accurately conceptualized to interpret the images meaningfully. There are two standard orientations: longitudinal (eg, imaging the aorta along its length, so that it appears as two parallel lines) and transverse (eg, imaging the aorta across its width, so that it is visualized as a circle) both must be acquired to properly perform a transabdominal ultrasound.
Understanding gray scale imaging An ultrasound image comprises thousands of pixels. Each pixel is a particular shade of gray depending on the strength of the returning ultrasound signal. Tissues that are identified as strong reflectors will return ultrasound images that range from brilliant gray to white. Weak reflecting tissues will be seen as a dark shade of gray to black. Ultrasound examination is reported in terms of six categories of this gray scale imaging (Table 6-1).
Cyst On an ultrasound examination a cyst characteristically appears to be anechoic with thin walls. A complex cyst will appear anechoic with thickened wall, and may contain debris.
Calcification Posterior shadowing is associated with calculi. This refers to acoustic impedance between the calculus and the surrounding tissue or fluid (in the case of bile).
Solid structures It is important to remember that solid masses may present on ultrasonography as a range of gray shades. Hepatomas may appear heterogeneous, while metastatic tumors may appear hypoechoic or hyperechoic.
General instrumentation and technique
Transabdominal ultrasound should be performed with a multifrequency sector, curvilinear array or linear array transducer.1 Adequate penetration and resolution can be obtained using a 3.5-MHz transducer for the intra-abdominal cavity while a 5-MHz curved array transducer is optimal for evaluating the bowel and its mesentery. A higher-frequency probe (7.5 MHz) will provide higher-resolution images, but should be reserved for more superficial lesions of the abdominal wall given its lower depth of penetration.
With patients in the supine position, the entire abdominal cavity needs to be explored and evaluated for other pathology or concomitant disease. The dependent portions of the abdomen should be examined carefully for fluid, which might suggest a perforated viscus. The transducer should first be placed in the subxiphoid region and tilted toward the pericardium. It is then placed in the right midaxillary line and swept subcostally to inspect the liver, right kidney, diaphragm, subhepatic region and Morison pouch. Following this, the left kidney, spleen, and diaphragm are evaluated from the left anterior, middle, and posterior axillary lines. With the patient in reverse Trendelenburg position and the transducer oriented longitudinally, the epigastric region and right paramedian region are evaluated for pneumoperitoneum, which would appear as a hyperechoic line inferior to the abdominal wall. Free air might also be seen between the liver and abdominal wall with the patient in the left lateral decubitus position. Following a systematic assessment of all parts of the abdomen, attention should be focused on the area where the pain is most severe. If the view of the bowel is obscured by air, the technique of graded compression can be utilized to displace the interposing material. Applying continuous pressure to the patient’s abdominal wall reduces artifact and improves the overall image.1
Indications for transabdominal ultrasound
Acute abdomen Due to its ease of use, low risk, and relatively low cost, ultrasound has become a safe, accessible alternative to CT, MRI, and other minimally invasive approaches to the evaluation of patients with abdominal pain. Transabdominal ultrasound findings often complement the physical examination and can help guide further diagnostic studies or operative interventions. Hernias, acute cholecystitis, appendicitis, bowel obstruction, intestinal ischemia, and diverticulitis are among the many conditions presenting with acute abdominal pain that can be evaluated constructively utilizing ultrasonography.1
Ultrasonography in the setting of an acute abdomen is conducted with the patient supine. The technique is no different to standard ultrasonography. However, the objective is not to delineate the areas of suspicion or confirm diagnosis; rather it is to evaluate the abdominal cavity for other pathologic changes and thus assist in establishing a differential diagnosis. The survey commences with visualization of the liver and gallbladder, followed by the common bile duct. The retroperitoneum, right and left kidneys, the stomach, duodenum and pancreas, and upper abdominal organs are imaged in an orderly fashion.
The evaluation is completed by imaging the pelvis and searching for the presence of intra-abdominal fluid in the pouch of Douglas. The next steps focus on examining the area of reported pain and are therefore of major interest. In situations where a perforated viscus is suspected, it is important to turn the patient into the left decubitus position and thus be able to identify intraperitoneal air between the liver and the abdominal wall. A diagnostic tap with aspiration under ultrasound guidance is recommended in all cases of suspected perforation with evidence of intra-abdominal fluid.
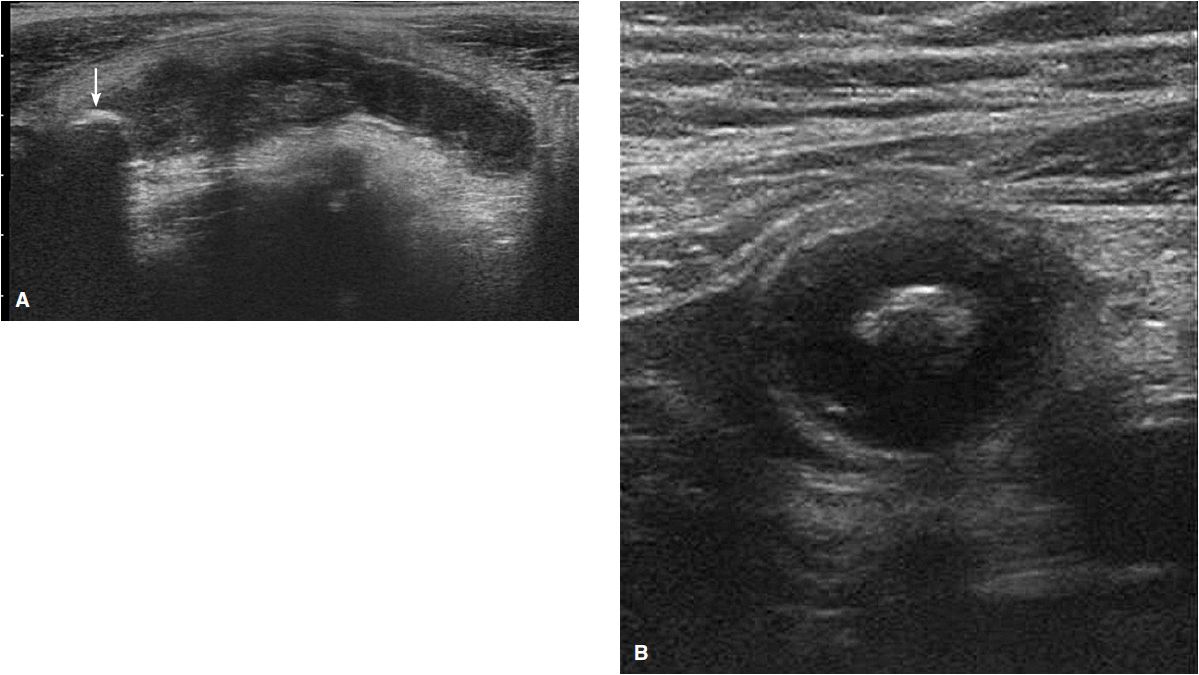
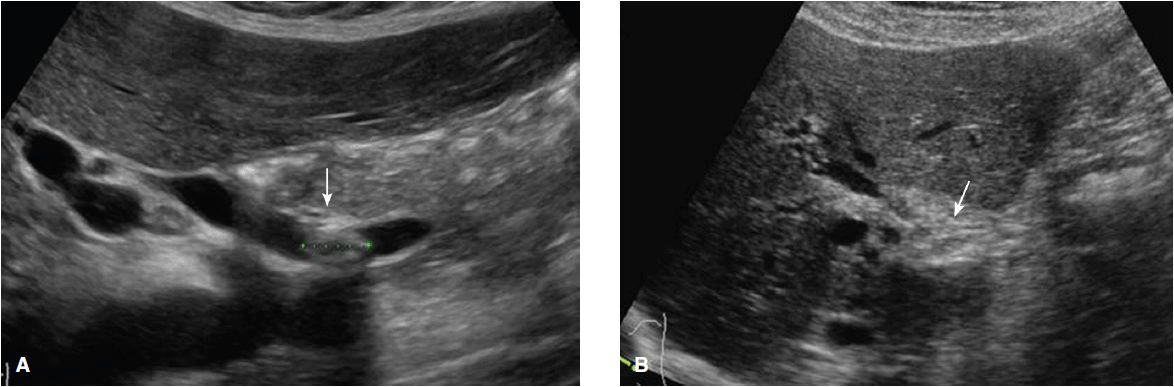
Acute appendicitis In 1986, Puylaert first described the use of ultrasound in the diagnosis of acute appendicitis.2 He utilized a technique referred to as graded compression that starts by placing the probe over the area of interest and then gradually increasing the pressure applied, thus compressing the cecum and bowel to better visualize the appendix. An inflamed appendix is imaged more easily than the normal appendix because of its larger size and its distension with fluid. It appears as a blind-ended tubular structure with a laminated wall arising from the base of the cecum; it is notably noncompressible and aperistaltic with a diameter greater than 6 mm.3 The “target sign” is a characteristic feature in ultrasonography (Figure 6-1). Puylaert reported a sensitivity of 89% and specificity of 100% for this technique.2
Figure 6-1. (A) Longitudinal view of acute appendicitis with thickened, noncompressible hypervascularized appendix and fecolith (arrow). (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=187&case=4773) ID: /32589-Afbeelding2.jpg; (B) Transverse view of a fluid-filled appendix and a large fecolith at the base with a “target sign” appearance. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=187&case=4774) ID: /32594-Afbeelding2.jpg
Appendicoliths appear as bright echogenic foci with distal acoustic shadowing. Lim and Quillin describe the use of color Doppler in detecting an inflamed appendix.4,5 The inflamed, thick-walled, noncompressible appendix, which is fixed in position by compression with the transducer, will be visualized as circumferential, colored rings, in contrast to the normal intestine which is thin walled and compliant with frequent peristalsis and therefore transmits minimum or no signals. Doppler signals disappear when gangrene or perforation is present. Although CT scanning has been purported as the imaging modality of choice for patients with possible acute appendicitis, critical analysis of CT utilization for this purpose has not been proven to have a clear and absolute advantage over ultrasonography in the acute setting of appendicitis.6,7,8
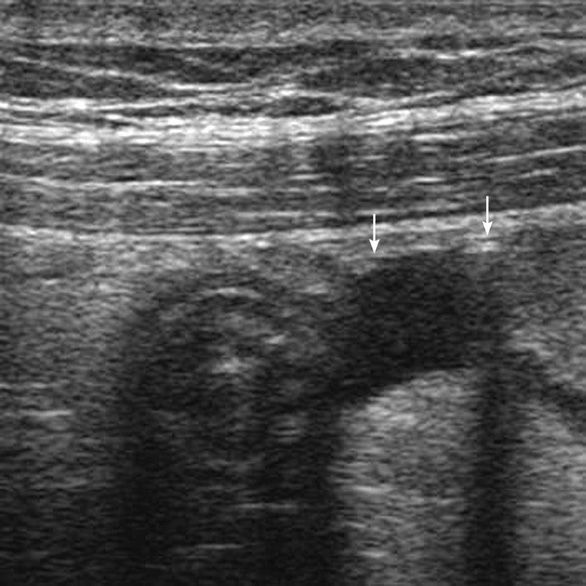
Small bowel obstruction Ultrasonography has been reported in one study as being more accurate in supporting the diagnosis of an ileus or of intestinal obstruction than plain flat and upright radiographic films.9 Examination for possible intestinal obstruction begins with systematic longitudinal and transverse scans of the abdominal cavity. In the longitudinal view, the bowel appears as a multilayered sandwich-like structure with a serpentine array of bowel loops. The lumen is between 3 and 5 mm and is easily compressible during graded compression. The sonographic hallmark for diagnostic purposes is seen in the transverse view with the “target” appearance of the bowel and enlarged transverse diameter of the small bowel between 10 and 20 mm, while that of the colon is 30 mm.
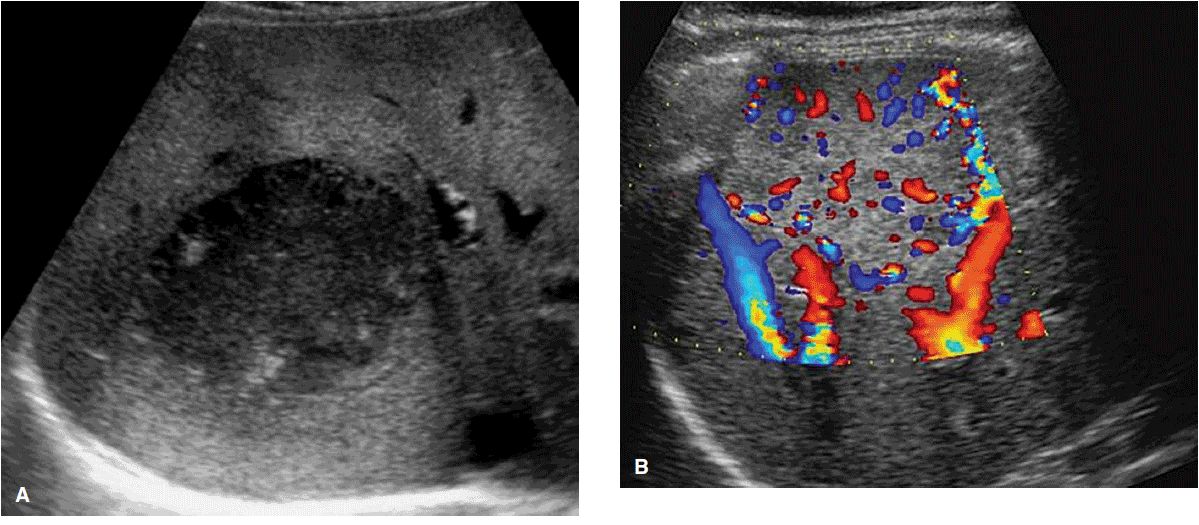
An obstructed bowel appears distended, fluid-filled with thickened walls; there is an absence of peristalsis. Computed tomography is superior to ultrasonography at delineating the cause and location of an intestinal obstruction. Ultrasonography, however, is considered the method of choice for diagnosing intussusception. The findings on imagining are characterized by segmental pathologic target phenomena consisting of multiple concentric rings with demonstration of mechanical obstruction (Figure 6-2).10,11
Figure 6-2. Small bowel intussusception with multiple concentric rings in transverse section. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=185&case=4968) ID: /34565-Afbeelding3.jpg
The value of ultrasonography in the difficult diagnoses of mesenteric infarction is unclear. The images demonstrate hyperperistaltic bowel with mucosal edema, which are nonspecific findings. As the ischemia progresses, the bowel wall may appear thicker than 6 mm. Phillips and colleagues have reported the successful use of color Doppler imaging in certain cases of small bowel infarction of the proximal superior mesenteric artery or thrombosis of the superior mesenteric vein.12
Hernias and abdominal wall masses Transabdominal ultrasound can be used to identify and distinguish between hernias, seromas, abscesses, and other abdominal wall masses. Moreover, it can be used to guide aspiration or biopsy of such lesions with high accuracy and minimal morbidity or risk to the patient.
Abdominal aortic aneurysm Abdominal aortic aneurysm should be considered in any patient who presents with abdominal pain of unknown etiology. In patients who are unstable, CT scan is too time-consuming and may delay definitive treatment. Bedside transabdominal ultrasound can rapidly and accurately detect the presence and size of a ruptured or nonruptured AAA with a sensitivity that approaches 100%.1
With the patient lying supine, a 3.5 MHz convex transducer should be used to identify the aorta below the xiphoid. The normal aorta should be an anechoic tubular structure with reflective walls that follows the curve of the lumbar spine and tapers off slightly at the inferior portion. The transducer should then be swept caudally toward the umbilicus in a transverse orientation to obtain measurements above and below the takeoff of the renal arteries. By orienting the transducer longitudinally, anteroposterior (AP) measurements can be obtained and the aorta assessed for the presence of a mural thrombus (Figure 6-3).
Figure 6-3. Transverse view of aortic aneurysm with intramural hemorrhage and dissecting thrombus. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=205&case=616) ID: /3336.jpg
Ultrasonography can also be used to detect the presence of an aortic dissection. In the presence of an aortic dissection, a channel of blood will track down inside the tunica media and appear as a thin echogenic septum within the true lumen. An intimal flap can sometimes be seen on longitudinal view and the vascular channels delineated using color Doppler flow.
Intra-abdominal sepsis and ascites In patients that present with signs of sepsis, it is often difficult to elicit a complete history or obtain a reliable physical examination. In this situation, ultrasound can be used to examine the dependent portions of the abdomen for free fluid and bowel edema that would suggest peritonitis (Figure 6-4). It can also be used to look for reverberation artifacts in the epigastric region and right upper quadrant, which might indicate presence of pneumoperitoneum.
Figure 6-4. Inflamed, thickened small bowel with free fluid (arrow) and air in the peritoneal cavity. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=194&case=3085) ID: /16168.jpg
Solid organ injury Ultrasound has become an indispensable tool in the emergency room setting and care for the patient with acute trauma. First introduced into practice in the 1970s in European trauma rooms, it was adopted into routine use by North American emergency teams in the 1990s. The focused assessment with sonography for trauma (FAST) is a limited ultrasound assessment with the sole objective of identifying the presence of free intraperitoneal or pericardial fluid. It is quick, can be performed at the bedside, and offers the option of repeat serial scans that may aid in the follow-up of a trauma patient who is managed nonoperatively. Ultrasound is less sensitive than DPL in detecting intraperitoneal blood and in estimating the blood volume that is free in the peritoneal cavity, but it does not involve any invasive intervention, which is required for DPL.
The accepted practice in emergency rooms is to screen all patients with blunt trauma and possible solid organ injury or hemoperitoneum with rapid ultrasound assessment (FAST). The patient may be monitored with repeat scans or taken for emergency surgical exploration depending on the findings and the clinical status of the patient.
Gallbladder and biliary tract pathology Transabdominal ultrasound is the initial diagnostic method of choice in cases of suspected cholecystitis and choledocholithiasis as the finding of cholelithiasis and bile duct stones will help guide further management. The normal gallbladder is typically an anechoic, oval-shaped, thin-walled structure that lies just under the right lobe of the liver, lateral to the portal vein. Occasionally it is enveloped within the liver parenchyma or is located more inferiorly toward the right iliac fossa. It is best visualized when the patient has been fasting. In the sagittal orientation, the probe should be swept horizontally from the right edge of the liver along its inferior surface toward the portal vein until the gallbladder comes into view. Gallstones should produce acoustic shadows that differ from shadows caused by loops of bowel by their lack of echogenic streaks.
The cystic duct can be seen running posteromedially from the medial side of the gallbladder neck toward the common bile duct. The corkscrew-shaped spiral valve of Heister is located at the most superior aspect of the duct. The common bile duct can be seen anterolateral to the portal vein. Unlike the branches of the portal vein, the intrahepatic bile ducts arising from the CBD have brightly echogenic walls. The CBD should be imaged in the transverse plane and traced through the head of the pancreas to the medial aspect of the duodenum. A curvilinear transducer with large footprint can help to minimize shadowing from overlying bowel gas and help to better visualize the duct.
The use of ultrasound in assisting in the diagnosis of gallbladder disease is well established. The patient is usually required to fast and is maintained in the supine position. The gallbladder is approached with the probe in the right lateral longitudinal and intercostal planes. Gallstones will appear as round, mobile echogenic foci within the lumen of the gallbladder. Stones larger than 1 mm will often cast a posterior shadow. The typical findings of acute cholecystitis include gallbladder wall thickening greater than 4 mm, hypoechogenic thickening of the tissues around the gallbladder, pericholecystic fluid, and localized pain while imaging the gallbladder with mild compression which is referred to as a “sonographic Murphy sign” (Figure 6-5).13,14 The presence of gallbladder wall stranding or layering echogenic gas within the lumen are suggestive of gangrenous and emphysematous cholecystitis, respectively. Chronic cholecystitis can be distinguished from acute cholecystitis by the pattern of mural calcification on ultra-sonography (porcelain gallbladder) with or without obliteration of the gallbladder lumen.
Figure 6-5. (A) Gallbladder filled with sludge and echogenic stones with posterior shadowing. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=154&case=3705) ID: /20500.jpg; (B) Inflamed gallbladder with pericholecystic fluid (arrow) and stone in the gallbladder neck. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=161&case=6224) ID: /47219-Afbeelding2.jpg;
Ultrasound can also be utilized to detect other pathologic findings in the gallbladder and biliary tree, including adenomyomatosis, polyps, malignant neoplasms, and choledocholithiasis with biliary obstruction. Adenomyomatosis is a benign condition due to hyperplasia and invagination of the epithelium and muscular layers of the gallbladder. It most typically presents as small echogenic intramural diverticula or as a polypoid lesion located in the gallbladder fundus. Gallbladder carcinoma can appear as diffuse wall thickening (especially if greater than 1 cm) or a heterogeneous, vascular mass that obscures the normal plane between the gallbladder and liver.
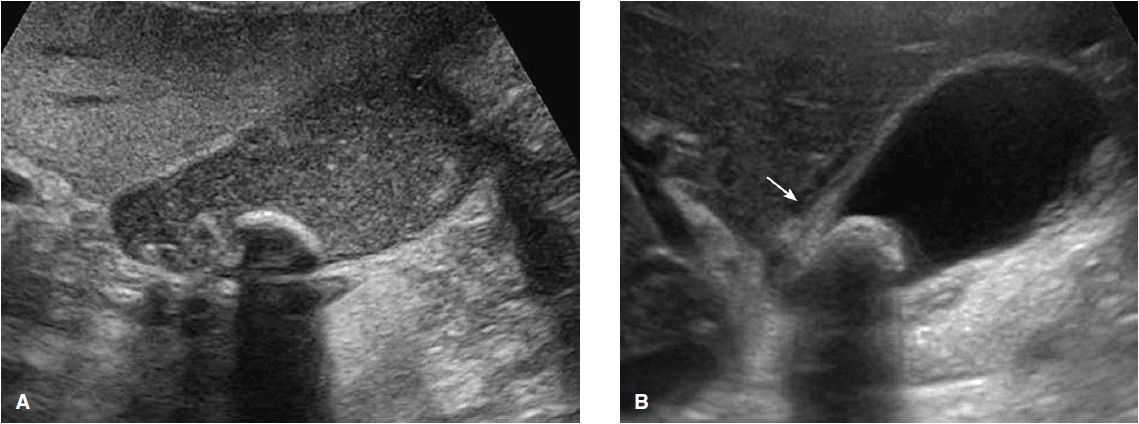
Ultrasonography has a sensitivity of 75% for the detection of stones within the common bile duct.15 The normal extrahepatic bile duct should be less than 6 mm at the level of the crossing right hepatic artery. A dilated duct in the presence of obstructive symptoms is highly suggestive of choledocholithiasis and can be confirmed by the presence of echogenic stones with distal acoustic shadows on ultrasonography. Dilated common bile ducts within the porta hepatis with tapering of the CBD and surrounding mass are suggestive of a cholangiocarcinoma. This intra- or extrahepatic malignancy can either spread outward from the CBD (exophytic), be contained within the wall of the duct (infiltrative), or appear as a polyp-like mass within the duct (polypoid) (Figure 6-6).
Figure 6-6. (A) Longitudinal view of stones in the distal common bile duct. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=154&case=5664) ID: /41318-Afbeelding1.jpg; (B) Cholangiocarcinoma with an intraductal mass (arrow) and dilated intrahepatic ducts. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=156&case=3421) ID: /18694.jpg
Liver pathology The normal liver has a homogeneous pattern that is more echogenic than the renal cortex, but less echogenic than the spleen. It is anatomically divided into eight segments based on the branching of the portal structures and hepatic veins that appear as sonolucent tubular structures within the liver parenchyma. The three hepatic veins typically run in an oblique direction from the upper end of the IVC to the right, middle, and left portions of the liver.
The liver is best evaluated with the patients turned slightly on their left side, which allows the liver to slide downward into a better view. The patient should hold his or her breath, which depresses the diaphragm. The probe is placed in a sagittal orientation in the right anterior axillary line and swept horizontally from right to left until the far edge of the left lobe is visualized. The probe is then rotated and oriented axially under the right ribs and angled upward until the top of the liver comes into view. It is then swept vertically from the cranial to caudal direction. If the liver is obscured by the lower ribs, the probe can be rotated until it lies along the intercostal space. In order to visualize the hepatic veins, the probe should be oriented axially under the xiphoid and tilted cranially to bring the junction of the IVC with the right atrium into view. The hepatic veins should then be visualized running into the IVC.
The portal vein runs in a horizontal orientation from the inferior surface of the liver along the right lobe. The portal vein has a more reflective wall than the hepatic veins and is therefore more echogenic. It is best visualized by placing the probe in the midclavicular line, where it is rotated counter-clockwise from the sagittal orientation until it points toward the right shoulder, and is then tilted medially toward the aorta. The portal vein can then be followed down to where it joins the superior mesenteric and splenic veins.
Transabdominal ultrasound is often used to detect and localize benign or malignant neoplasms, metastases, cysts, hemangiomas and abscesses within the liver (Figure 6-7). Hepatic adenomas typically appear as well-demarcated, isolated lesions with variable echogenicity on ultrasound. Focal nodular hyperplasia is difficult to distinguish from an adenoma, but is more often isoechoic with characteristic “spoke wheel” or “stellate” vascularity on color Doppler. Hepatic metastases have a variable appearance depending on their origin and there are no features that routinely distinguish them from primary hepatocellular carcinoma. Tumors arising from the gastrointestinal tract are more likely to be multifocal, hyperechoic, and have a hypoechoic rim creating a “bull’s-eye” or “target” appearance on ultrasound. Hepatocellular carcinoma is more often hypoechoic in relation to the surrounding liver parenchyma, with posterior echo enhancement or “halo” effect. Portal or hepatic vein invasion is also more suggestive of hepatocellular carcinoma than metastatic disease.
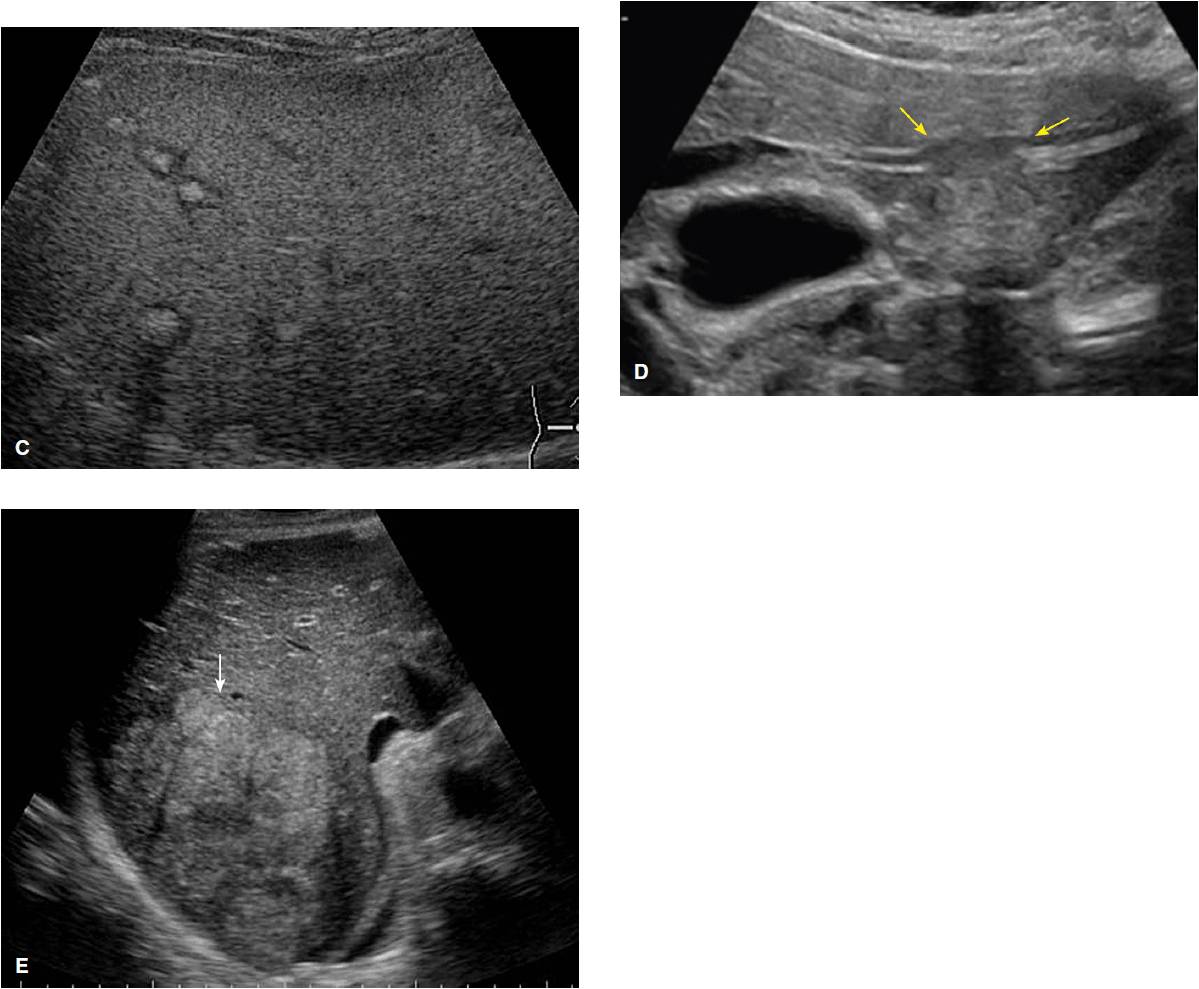
Figure 6-7. (A) Amebic liver abscess. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=141&case=3082) ID:/16124.jpg; (B) Large focal nodular hyperplasia characterized by isoechoic mass and color Doppler demonstrating “spoke wheel” vascularity. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=129&case=3141) ID: /16595.jpg; (C) Multiple hyperechoic calcified liver metastases with hypoechoic halo in a patient with breast carcinoma. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=144&case=8) ID:/129.jpg; (D) Liver metastasis with invasion and stenosis of a left portal vein. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=144&case=3597) ID: /19900.jpg; (E) Large hepatocellular carcinoma (arrow) in a cirrhotic, nonhomogenous liver. (Used with permission from www.ultrasoundcases.info/Slide-View.aspx?cat=142&case=3144) ID: /16631.jpg
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree