Functions
• General somatic efferent (GSE). Somatic motor innervation to the lateral rectus (LR) muscle.
Anatomy
• The abducens nucleus is in the dorsal pontine tegmentum at the level of the lower pons, just ventral to the fourth ventricle (separated from floor of the fourth ventricle by genu of facial nerve) (Figs. 6.1, 7.1).
• Fascicles course ventrally through the pons and through the medial lemniscus (ML) medial to facial nerve fascicles to emerge at the pontomedullary junction just lateral to the pyramid (Fig. 6.2). The cisternal segment ascends in the prepontine cistern through the subarachnoid space of the posterior fossa and traverses Dorello’s canal, extending over the petrous apex and beneath Grüber’s (petroclinoid) ligament to enter the cavernous sinus. The petroclinoid ligament is a fibrous band connecting the lateral margin of the dorsum sellae to the upper border of the petrous part of the temporal bone. Dorello’s canal is a fibroosseous channel bounded by the apex of the petrous bone inferolaterally, the petroclinoid ligament superiorly and the dorsum sella medially. Once in the cavernous sinus, cranial nerve (CN) VI travels just lateral to the internal carotid artery (ICA) and medial to CN V1 (Fig. 6.3), then enters the orbit at the medial end of the superior orbital fissure (SOF), traverses the annulus of Zinn (tendinous ring), and innervates the LR muscle. Note that unlike the other CNs (III, IV, V1, V2) which lie between the two leaves of dura that make up the lateral wall of the cavernous sinus, CN VI actually lies within the cavernous sinus adjacent to the ICA (Fig. 6.3).
• LR muscle functions to abduct the eye (Fig. 6.4).
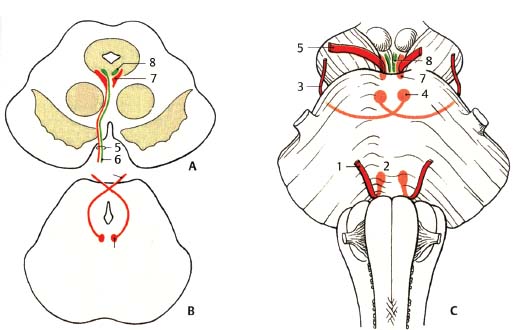
Fig. 6.1 Comparison of nuclear regions and exits of oculomotor, trochlear, and abducens nerves. (A) Midbrain at the level of the superior colliculus. (B) Midbrain at the level of the inferior colliculus. (C) Ventral view of brainstem. (1, abducens nerve; 2, abducens nucleus; 3, trochlear nerve; 4, trochlear nucleus; 5, oculomotor nerve; 6, visceromotor [parasympathetic] fibers; 7, oculomotor nucleus; 8, Edinger-Westphal nucleus.)
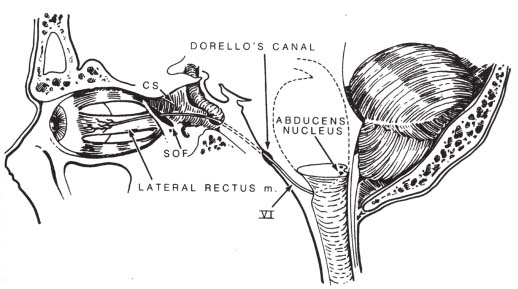
Fig. 6.2 Sagittal view of the abducens nerve from nuclear origin in the lower pontine tegmentum to its end point in the lateral rectus muscle (see text). (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
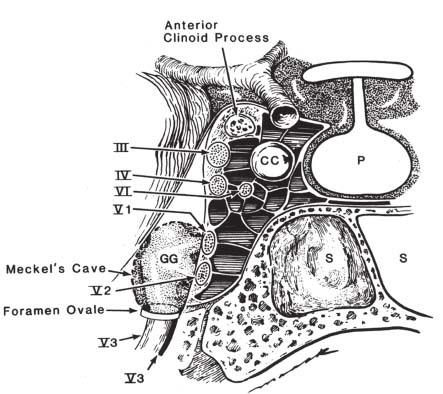
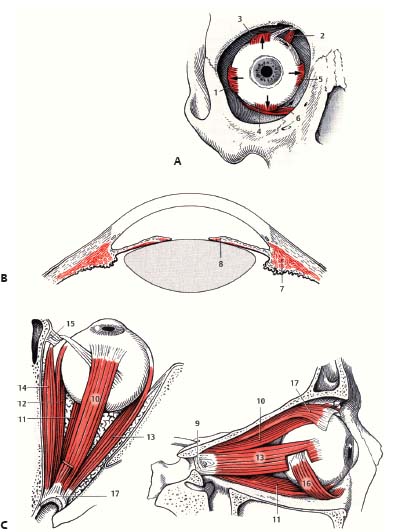
Fig. 6.4 Schematic of extraocular and intraocular muscles. (A) Anterior view. (1, LR muscle; 2, SO muscle; 3, SR muscle; 4, IR muscle; 5, MR muscle; 6, IO muscle.) (B) Intraocular muscles. (7, ciliary muscle; 8, sphincter pupillae muscle.) (C) Superior (left) and lateral (right) views. (9, common annular tendon [annulus of Zinn]; 10, SR muscle; 11, IR muscle; 12, MR muscle; 13, LR muscle; 14, SO muscle; 15, trochlea; 16, IO muscle; 17, LPS muscle.)
Abducens Nerve: Normal Images (Figs. 6.5, 6.6, 6.7)
Abducens Nerve Lesions
• Lesions of the abducens nerve cause impaired ipsilateral lateral gaze. Therefore, patients with unilateral abducens palsy complain of horizontal diplopia, worst in the direction of the paretic LR muscle.
• Unlike a peripheral CN VI lesion, a nuclear CN VI lesion impairs ipsilateral gaze of both eyes. This is due to the fact that the abducens nuclear complex contains interneurons projecting via the medial longitudinal fasciculus (MLF) to the contralateral oculomotor nucleus (innervating the contralateral MR muscle). Therefore, a right-sided lesion of the abducens nucleus impairs rightward gaze of both eyes, whereas a right-sided lesion of the abducens nerve impairs rightward gaze of the right eye only (and hence horizontal diplopia with image separation worst on far rightward gaze). This is the only cranial nerve in which lesion of the root fibers and nucleus do not produce the same effect.
• Rare congenital lesions of CN VI include Mobius syndrome (a genetic disorder caused by absence or underdevelopment of CNs VI and VII, characterized by horizontal gaze palsy associated with facial diplegia) and Duane retraction syndrome (congenital unilateral horizontal abduction deficit due to absence of the abducens nerve on one side, characterized by gaze palsy with globe retraction).
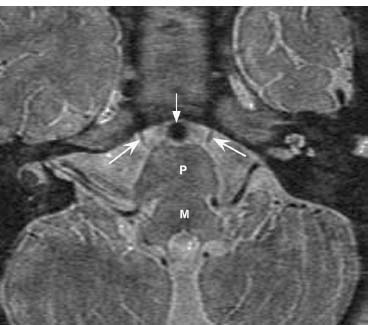
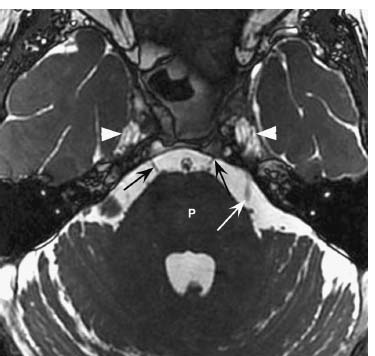
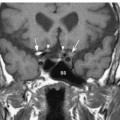
Fig. 6.6 Axial fast imaging employing steady-state acquisition (FIESTA) sequence shows in fine detail the cisternal segments of CN VI (black arrows) at the level of the mid pons (P) and fourth ventricle, as CN VI courses toward Dorello’s canal. The left CN V (white arrow) is faintly seen. Note the normal CSF within Meckel’s cave bilaterally (arrowheads).
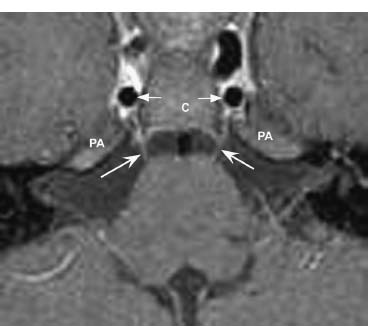
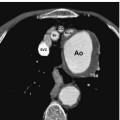
Fig. 6.7 Axial postcontrast T1-weighted image shows faint normal enhancement of CN VI. On this image, the nerves (concave arrows) are seen extending over the medial aspect of the petrous apices (PA) as they head for Dorello’s canal. Note the cavernous carotid artery flow voids (straight arrows) within the cavernous sinus lateral to the clivus (C).
Types
Brainstem Lesions (Abducens Nuclear Lesions)
• Produce a conjugate (both eyes involved) horizontal gaze palsy toward the side of the lesion
• Often associated with other neurologic signs of injury to the pons (usually ipsilateral peripheral CN VII palsy)
Fascicular Lesions
• Result in an ipsilateral abduction deficit
• Also associated with damage to nearby pontine structures (anterior paramedian pontine lesions)
• Paramedian pontine lesions (including nuclear and fascicular lesions) may be caused by
 ischemia,
ischemia,
 inflammation,
inflammation,
 demyelination (e.g., multiple sclerosis [MS]),
demyelination (e.g., multiple sclerosis [MS]),
 compressive mass lesion (tumor, abscess, cavernous vascular malformation).
compressive mass lesion (tumor, abscess, cavernous vascular malformation).
• Millard-Gublersyndrome. Unilateral lesion of ventrocaudal pons affecting corticospinal tract, CN VI fascicles and CN VII with contralateral hemiplegia, ipsilateral LR paresis, and facial paresis
Lesions of the Cisternal Segment (in Prepontine Cistern)
• Result in isolated abduction deficits
• Associated with contralateral hemiparesis if corticospinal tract involved by extrinsic compression
• Causes include the following:
 Ischemia (e.g., ischemic abducens neuropathy from diabetes)
Ischemia (e.g., ischemic abducens neuropathy from diabetes)
 Neoplasm (e.g., cerebellopontine angle tumors, clival meningioma, clival chordoma, chondrosarcoma, schwannoma, nasopharyngeal carcinoma)
Neoplasm (e.g., cerebellopontine angle tumors, clival meningioma, clival chordoma, chondrosarcoma, schwannoma, nasopharyngeal carcinoma)
 Vascular (e.g., dolichoectatic basilar arteries, aneurysms)
Vascular (e.g., dolichoectatic basilar arteries, aneurysms)
 Trauma (nerve stretching and/or compression)
Trauma (nerve stretching and/or compression)
 Inflammation (e.g., meningitis with secondary neuritis)
Inflammation (e.g., meningitis with secondary neuritis)
 Demyelinating disease (Miller-Fisher variant of Guillain-Barré syndrome includes ophthalmoplegia, ataxia, and areflexia)
Demyelinating disease (Miller-Fisher variant of Guillain-Barré syndrome includes ophthalmoplegia, ataxia, and areflexia)
 Changes in intracranial pressure (ICP). CN VI palsies are noted both with increased ICP but also with decreased ICP (e.g., from intracranial hypotension related to a dural cerebrospinal fluid [CSF] leak). Therefore an ipsilateral CN VI palsy often turns out to be a “false localizing sign” in the absence of localizing pathology.
Changes in intracranial pressure (ICP). CN VI palsies are noted both with increased ICP but also with decreased ICP (e.g., from intracranial hypotension related to a dural cerebrospinal fluid [CSF] leak). Therefore an ipsilateral CN VI palsy often turns out to be a “false localizing sign” in the absence of localizing pathology.
 Radiation injury
Radiation injury
Lesions at the Petrous Apex and Dorello’s Canal
• Concomitant involvement of CN V is frequent.
• Causes include the following:
 Infectious lesions.
Infectious lesions.
• Skull base osteomyelitis.
• Petrous apicitis.
• Gradenigo syndrome. Inflammation of the petrous apex (petrous apicitis) leads to damage to the trigeminal (CN V) and abducens (CN VI) nerves with facial pain/numbness and ipsilateral lateral rectus palsy.
 Trauma (e.g., skull base fracture involving clivus and petrous apex).
Trauma (e.g., skull base fracture involving clivus and petrous apex).
 Neoplasms (e.g., meningiomas, schwannomas, chordomas, chondrosarcomas, nasopharyngeal carcinomas, metastases).
Neoplasms (e.g., meningiomas, schwannomas, chordomas, chondrosarcomas, nasopharyngeal carcinomas, metastases).
 Inflammatory lesions (e.g., cholesterol granuloma, cholesteatoma, mucocele).
Inflammatory lesions (e.g., cholesterol granuloma, cholesteatoma, mucocele).
 Intrapetrous carotid artery aneurysms are rare but may cause CN VI palsy.
Intrapetrous carotid artery aneurysms are rare but may cause CN VI palsy.
Lesions in the Cavernous Sinus/Superior Orbital Fissure
• Concomitant Horner syndrome suggests cavernous lesion (because sympathetic fibers travel with the cavernous portion of the ICA).
• Neoplasm (e.g., meningioma, lymphoma, metastasis).
• Vascular (carotid-cavernous fistula, giant ICA aneurysm).
• Inflammatory (e.g., sarcoidosis, Tolosa-Hunt syndrome).
• Infection (e.g., bacterial or fungal sphenoid sinusitis with extension to the cavernous sinus).
• Pituitary apoplexy (acute enlargement of the pituitary gland leads to acute cavernous sinus compression).
• Radiation injury (e.g., following radiosurgery for cavernous sinus meningiomas).
Lesions of the Orbit
• Lesions of the orbit do not typically lead to a palsy of CN VI.
• Other conditions of the orbit may present with an isolated abduction deficit (e.g., thyroid orbitopathy, myasthenia gravis). In thyroid orbitopathy, inflammatory infiltration and interstitial edema result in increased fatty mass and muscle enlargement, leading to mechanical restriction of the globe. In myasthenia gravis, weakness of extraocular muscles may present as diplopia, often accompanied by ptosis due to weakness of the levator palpebrae superioris (LPS) muscle; indeed in ~20% of patients weakness remains confined to the extraocular and eyelid muscles (ocular myasthenia).
Treatment
• Correction of diplopia following CN VI injury may require prism therapy and/or strabismus surgery. Correction should not be undertaken until recovery is complete. Occasionally, botulinum toxin is injected into the contralateral medial rectus muscle to minimize diplopia.
Abducens Nerve: Pathologic Images
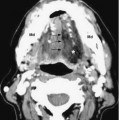
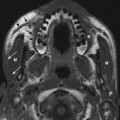
A 28-year-old female presents with horizontal diplopia and is found to have a left CN VI palsy (Figs. 6.8, 6.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree