SONOGRAM ABBREVIATIONS
A Ascites
Ao Aorta
CA Celiac axis
CBD Common bile duct
CHD Common hepatic duct
Du Duodenum
GB Gallbladder
HA Hepatic artery
HV Hepatic vein
IMV Inferior mesenteric vein
IVC Inferior vena cava
K Kidney
L Liver
LHV Left hepatic vein
LLS Left lateral segment
LMS Left medial segment
LPV Left portal vein
MHV Middle hepatic vein
MPV Main portal vein
P Pancreas
PV Portal vein
RAS Right anterior segment
RPS Right posterior segment
RPV Right portal vein
S Spine
SMA Superior mesenteric artery
SMV Superior mesenteric vein
SA Splenic artery
SV Splenic vein
KEY WORDS
Alkaline Phosphatase. Enzyme that catalyses the cleavage of inorganic phosphate. Elevated with biliary obstruction.
ALT. Alanine aminotransferase. Enzyme involved in protein metabolism. Increased in alcoholic hepatitis, jaundice, and cirrhosis. Formerly called serum glutamic-pyruvic transaminase (SGPT).
Ampulla of Vater. The point at which the common bile duct and pancreatic ducts enter the duodenum.
AST. Aspartate aminotransferase. Enzyme involved in synthesis of amino acids. Elevated in acute hepatitis and cirrhosis. Formerly called serum glutamic oxaloacetic transaminase (SGOT)
Biliary Atresia. Progressive obliteration of the extrahepatic and proximal intrahepatic bile ducts, as well as the gallbladder. Usually diagnosed within the first 2 weeks of life.
Bilirubin. Yellowish pigment in bile formed by red blood cell breakdown. Increases with hepatic disorders in which metabolism is impaired, such as cirrhosis or hepatitis. Also increases with obstructive disease such as gallstones. Bilirubin is classified as direct or indirect. Direct (conjugated) bilirubin is excreted in urine, whereas indirect (unconjugated) is not. Most laboratories report total and direct bilirubin. Indirect is calculated by subtracting the direct value from the total.
Cavernous Transformation of the Portal Vein. The extrahepatic portal vein becomes thrombosed and is replaced by numerous collateral veins in the porta hepatis.
Cholangiocarcinoma. A malignant neoplasm arising from the bile ducts.
Choledochal Cyst. Congenital dilatation of the common bile duct. Usually found in children but may not be diagnosed until adulthood.
Choledocholithiasis. Stones in the biliary tree.
Cirrhosis. Progressive hepatocellular disease. Common causes include excessive alcohol or drug use and viral infection, although there are many other etiologies. May result in fibrosis, jaundice, portal hypertension, and liver failure.
Collaterals. Also called varices. Dilated veins that occur with portal hypertension. Seen principally in the region of the porta hepatis, pancreas, and splenic hilum.
Common Bile Duct. Portion of the biliary duct formed by the confluence of the common hepatic duct and the cystic duct.
Common Hepatic Duct. Portion of the biliary duct formed by the confluence of the right and left hepatic ducts.
Coronary Vein. Vein that arises from the splenic vein in the midline and courses superior and to the left. Becomes dilated in the setting of portal hypertension.
Courvoisier Gallbladder. Enlarged, palpable gallbladder. Results from distal obstruction of the common bile duct (CBD) secondary to a pancreatic head mass.
Cystic Duct. Drains the gallbladder. Joins the common hepatic duct to form the CBD.
Fatty Infiltration. Infiltration of hepatocytes by lipids. Eventually results in fat cells being surrounded by fibrous material. Common causes include hepatitis, diabetes, metabolic disorders, and pregnancy. May be focal or diffuse.
GGT. Gamma glutamyl transferase. Biliary enzyme that increases with obstructive jaundice and liver disease.
Glisson’s Capsule. Fibrous membrane that surrounds the liver, as well as the portal triads within the liver.
Glycogen Storage Disease. Disease process in which large quantities of glycogen are abnormally deposited within the liver, resulting in fatty infiltration and tumors.
Hemolytic Anemia. Anemia resulting from destruction of red blood cells. Either congenital or acquired from a variety of causes including various infections.
Hepatitis. Inflammation of the liver due to viral infection or less commonly, autoimmune disease. May be acute or may become chronic after an acute episode.
Hepatocellular Disease. Diffuse disease affecting the liver parenchyma such as cirrhosis, fatty infiltration, or hepatitis.
Hepatofugal. Portal vein flow away from the liver. This pattern can be seen in patients with severe portal hypertension.
Hepatopetal. Normal portal vein flow, toward the liver.
Jaundice (Icterus). Yellow pigmentation of the skin due to excessive bilirubin accumulation. Usually secondary to liver or biliary disease.
Klatskin Tumor. A type of cholangiocarcinoma, an adenocarcinoma of the common hepatic duct bifurcation.
LDH. Lactic dehydrogenase. Enzyme that catalyses the formation and removal of lactate. Elevated with liver disease.
Porta Hepatis. Transverse fissure on the visceral surface of the liver in which the CBD, proper hepatic artery, and main portal vein (MPV) run alongside each other as they leave or enter the liver.
Portal Hypertension. Increased portal venous pressure usually secondary to liver disease (most commonly cirrhosis); leads to dilatation of the portal vein with splenic and superior mesenteric vein enlargement, splenomegaly, and formation of collaterals. Can also be caused by portal or splenic vein thrombosis.
Portal Triad. Portal vein, hepatic artery, biliary duct.
Primary Biliary Cirrhosis. Autoimmune disease resulting in irreversible destruction of the liver and bile ducts.
Regenerating Nodule. Regenerating areas of hepatocytes surrounded by fibrotic septa.
Sphincter of Oddi. Annular sheath of muscle contracting around the ampulla of Vater.
Varices. Dilated veins.
RELEVANT LABORATORY VALUES*
*Reference ranges for individual laboratories may vary slightly.
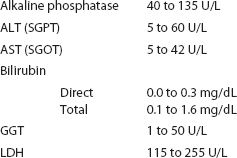
INCREASED LABORATORY VALUES DIFFERENTIAL
THE CLINICAL PROBLEM
There are three basic mechanisms by which jaundice occurs: red blood cell destruction, hepatocellular disease, or obstruction of the intrahepatic or extrahepatic bile ducts.
RED BLOOD CELL DESTRUCTION
Destruction of red blood cells in hemolytic anemias results in jaundice. In this setting, red cells are destroyed so rapidly that an elevated bilirubin results. Hemolytic anemias are caused by infection, certain medications, autoimmune disorders, and inherited conditions. The spleen and the liver, the principal sites of red blood cell removal, may become enlarged.
HEPATOCELLULAR DISEASE
Hepatocellular disease causes impaired hepatic cell function and cell death, which leads to a buildup of bilirubin and elevates the serum enzymes AST, ALT, and GGT. Alcoholic liver disease is the most common form; it progresses from alcoholic hepatitis to fatty infiltration of the liver to cirrhosis. Other common causes of hepatocellular disease include hepatitis, metabolic disorders, and malaria.
OBSTRUCTION OF INTRAHEPATIC OR EXTRAHEPATIC BILE DUCTS
Bile ducts dilate proximal to the site of obstruction. Unlike hemolytic anemia or hepatocellular disease, obstruction of the biliary system is treated surgically.
When bile excretion is blocked, urine and serum bilirubin, serum cholesterol, and serum alkaline phosphatase are elevated. Severe nonobstructive liver disease can also elevate these enzymes.
Common causes of bile duct obstruction include gallstones and choledocholithiasis, pancreatic tumors, or tumors in the bile ducts, such as Klatskin tumors. Primary sclerosing cholangitis and biliary strictures will also result in obstruction. In the infant and small child, two other important obstructive processes occur. Biliary atresia is the most common type of biliary obstructive disease in this age group. It is a progressive obliteration of the extrahepatic bile ducts and often the gallbladder. The proximal aspects of the intrahepatic bile ducts may also be involved. Symptoms usually present between 2 and 6 weeks after birth. Treatment includes surgically created drainage of bile into the intestine if the obstruction is extrahepatic. With intrahepatic obstruction, liver transplant is the only treatment option.
A choledochal cyst is a segmental dilatation of either the intra- or extrahepatic bile ducts. This is a congenital anomaly that can result in biliary dilation proximal to the cyst formation. Usually diagnosed in childhood, this condition may also be discovered later in life, and is treated surgically.
Ultrasound is often able to ascertain the cause of jaundice, allowing the clinician to determine the appropriate treatment method.
Anatomy
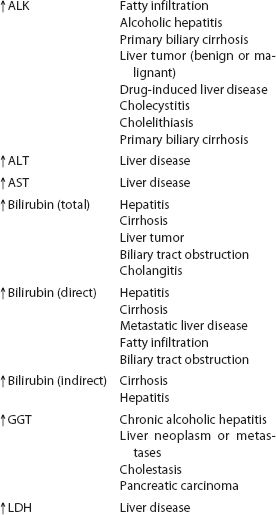
Diagnosis of biliary obstruction requires a thorough knowledge of the normal anatomy of the liver and biliary system, as well as vascular structures within the liver (Fig. 10-1).
LIVER ANATOMY
Liver anatomy may be described anatomically, based on external markings, or segmentally based on internal lobar divisions. From an anatomic standpoint, the liver can be divided into right, left, and caudate lobes. The right lobe is separated from the left lobe by the main lobar fissure. The right lobe is divided into anterior and posterior segments by the right intersegmental fissure. The left lobe is divided into medial and lateral segments by the left intersegmental fissure. The caudate lobe is bordered posteriorly by the inferior vena cava (IVC), anteriorly and superiorly by the left medial lobe of the liver, and inferiorly by the MPV.
Segmentally, the middle hepatic vein divides the liver into left and right lobes. The left hepatic vein divides the left lobe into medial and lateral segments, and the right hepatic vein divides the right lobe into anterior and posterior segments.
BILIARY TREE
Normally, only a small segment of the biliary tree is seen by ultrasound within the liver—the common hepatic duct, which is formed by the confluence of the left and right hepatic ducts. As the duct crosses the portal vein and exits the liver, it is still considered the common hepatic duct until it merges with the cystic duct. At this point, it becomes the CBD. The cystic duct’s precise location is often difficult to visualize by ultrasound, however. Sonographically, the common hepatic duct lies within the porta hepatis, anterior to the right hepatic artery (RHA) and undivided right portal vein (Fig. 10-2). After joining the cystic duct, the CBD normally descends anterior and lateral to the MPV. The proper hepatic artery can be seen anterior and medial to the MPV (Fig. 10-3).
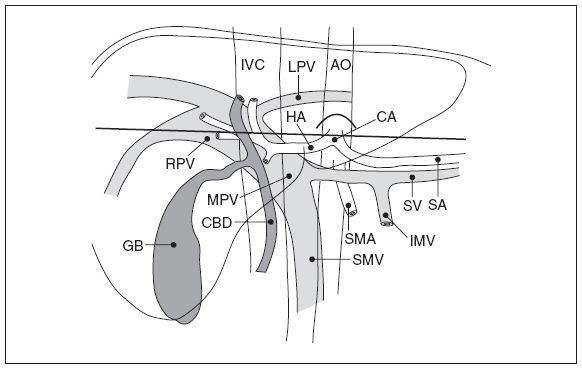
Figure 10-1. ![]() Diagram of the relationships between the biliary system and vascularity within the liver.
Diagram of the relationships between the biliary system and vascularity within the liver.
The normal diameter for the common hepatic duct and CBD varies within the literature. Additionally, recent reports have expressed concern that increased bile duct size associated with increased age and increased bile duct size after cholecystectomy, both historically thought to be normal findings, may not be. Although the bile ducts may enlarge slightly with age or status post cholecystectomy, any measurement above 6 to 7 mm in young patients and 8.5 mm in the elderly should be considered abnormal and followed accordingly.
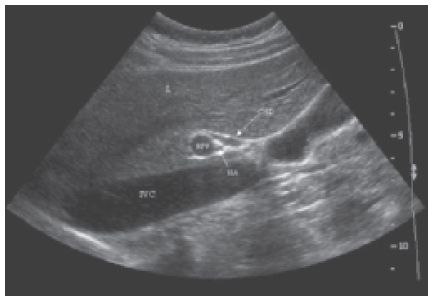
Figure 10-2. ![]() Longitudinal image of the liver, showing the relationship of the common hepatic duct to the right hepatic artery and undivided right portal vein.
Longitudinal image of the liver, showing the relationship of the common hepatic duct to the right hepatic artery and undivided right portal vein.
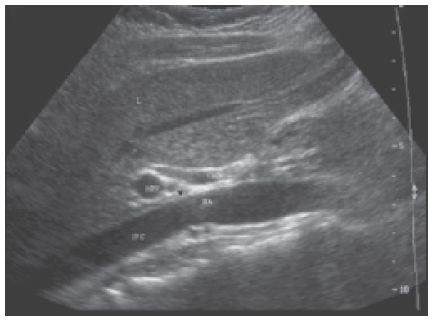
Figure 10-3. ![]() Longitudinal image of the liver showing the relationship of the common bile duct to the main portal vein and the proper hepatic artery.
Longitudinal image of the liver showing the relationship of the common bile duct to the main portal vein and the proper hepatic artery.
The portal veins, hepatic arteries, and bile ducts run in triads that are surrounded by Glisson capsule. This fibrous structure results in the walls of the portal veins appearing hyperechoic on ultrasound (Fig. 10-4). The MPV arises from the confluence of the splenic and superior mesenteric veins. As it enters the liver, it branches into the undivided right and left portal veins. The right branch then bifurcates within the right lobe of the liver into anterior and posterior segments. The left portal vein courses leftward within the left lobe. Smaller branches may occasionally be visualized. The portal veins run centrally, within the segments of the liver. Normal portal vein flow is hepatopetal.
HEPATIC VEINS
Hepatic veins (Fig. 10-5) are easily differentiated from portal veins because they are not surrounded by an echogenic wall. Hepatic veins course between the lobes and segments of the liver and drain into the IVC (Fig. 10-6).
HEPATIC ARTERIES
The common hepatic artery takes off from the celiac axis and courses over the anterior, superior edge of the pancreas. It gives rise to the gastroduodenal artery, the supraduodenal artery, and the right gastric artery. At this point, it is termed the proper hepatic artery and runs cephalad into the porta hepatis. It courses anterior to the MPV and to the left of the CBD. Once the proper hepatic artery enters the liver, it bifurcates into left and right branches. The RHA crosses between the common hepatic duct and the right portal vein. It may double back on itself (Fig. 10-7). Hepatic arteries can be a source of confusion in the region of the porta hepatis because they can be mistaken for a bile duct. Color or pulsed Doppler will easily make the distinction by showing flow if the vessel is hepatic artery. Hepatic artery flow is hepatopetal.
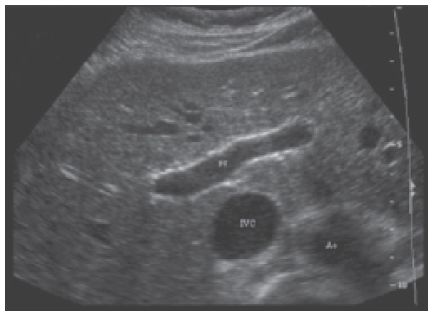
Figure 10-4. ![]() Transverse image of the liver showing the echogenic walls that surround the normal portal veins.
Transverse image of the liver showing the echogenic walls that surround the normal portal veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


