This article outlines a roadmap to achieving and maintaining excellence in an ultrasound (US) practice. We present constructive advice on how US practices can achieve and maintain quality, patient and referring physician satisfaction, and efficiency in the setting of rising examination volumes. Accreditation, sonographer and resident/fellow physician training, advanced practice sonographers, and Picture Archiving and Communication System/Artificial Intelligence in US are discussed. Advice for how to begin offering new US examinations, begin a practice at new US locations, improve quality assurance, and enhance marketing are covered.
Key points
- •
Excellence in ultrasound (US) practice can be achieved with attention to sonographer and physician training, and standardized facility-wide scanner-based protocols.
- •
Accreditation conveys a practice’s commitment to a national standard of excellence, establishing a framework for sonographer certification and US examination rigor.
- •
Advanced practice sonographers are helpful to provide high-quality, efficient care in busy US facilities.
- •
Strong information technology support is essential for operating a modern US practice, and AI promises to enhance workflow from image acquisition through interpretation.
- •
Offering novel sonographic examinations in existing facilities and providing US services at new practice locations are vital to enhancing the value of sonography across the care continuum.
Introduction
Ultrasound (US) continues to be a rapidly evolving modality with well-known benefits including portability, widespread availability, relatively low-cost, and lack of ionizing radiation associated with computed tomography (CT) and angiography. In the United States, an additional advantage is that US studies generally do not require insurance pre-authorization. Newer capabilities such as contrast-enhanced ultrasound (CEUS), and quantitative techniques such as elastography and fat quantification decrease the need for biopsy or more expensive noninvasive studies such as MRI with their associated longer wait times. In this article, we present practical advice on how US practices can achieve and maintain quality, patient and referring physician satisfaction, and efficiency in the setting of rising examination volumes. ,
Accreditation
Accreditation conveys commitment to a national standard of excellence and can increase provider and patient confidence in the quality of the US examinations performed. Additionally, specific sonographer certification and physician qualifications, as well as submission of high-quality images, inevitably set a high bar for the US practice to meet. Accreditation is offered by organizations including the American College of Radiology (ACR), American Institute of Ultrasound in Medicine (AIUM), and Intersocietal Accreditation Commission, each with their own benefits and specific requirements. A common theme is submission of complete US studies with requisite image acquisition parameters.
A single or small group of radiologist and sonographer leaders can serve as points of contact for the team, and can help identify, review, and save submission-worthy examinations. These examinations are generally reviewed for quality at multiple levels, with final authorization by a physician leader or the radiologist originally assigned to that case. The stepwise fashion allows for multiple checkpoints to detect problems prior to submission and review by the accrediting body. This also distributes the workload so that no one individual bears the considerable burden. The submission process is also valuable in informing the radiologists and sonographers as to the necessity of consistency, accuracy, and completeness in images and reports, as well as identifying any areas with incomplete imaging as judged by the accrediting organization, in order to achieve a national standard of excellence.
Training
Given the often-discussed “operator dependence” of US, physicians must feel comfortable in a sonographer’s ability to obtain requisite diagnostic images. As sonographers are the physician’s eyes, ears, and hands, they are essential for an efficient and accurate US practice. Our sonographers must meet departmental educational requirements (in part based on accreditation), including Registered Diagnostic Medical Sonographer, Registered Vascular Technologist, Registered Vascular Specialist, and American Registry of Radiologic Technologists in sonography or vascular sonography, or equivalent certifications, within a set number of years of hiring. Regardless of credentials, each sonographer is evaluated directly within our departments to identify any gaps in knowledge or areas of educational deficiency at hire, and a training plan is created, agreed upon, and implemented.
A detailed checkoff worksheet for each examination performed at a specific clinical site is used to review the sonographer’s capability to perform an examination appropriately at one of our institutions (MLR, MEL and FNT). Until they are confirmed, their examinations are “backscanned” by a more experienced sonographer and then reviewed by a sonologist or physician extender for quality and completeness. Aspects reviewed include quality of grayscale images, Doppler technique, and adherence to imaging protocols. Generally, 5 completed examinations that meet minimum standards (3 normal and 2 abnormal) are sufficient to allow independent scanning, acknowledging that more examinations may be required to show proficiency. If an experienced sonographer who commonly performs these examinations is hired, the required number of examinations may be reduced to 1 normal and 1 abnormal to show proficiency in local standards.
Radiology trainees are trained in an apprenticeship fashion, sitting alongside the attending and in proximity to the physician extenders so that they may benefit from all educational opportunities. They are trained in protocols and then expected to provide feedback to sonographers. In their early educational setting, the resident reviews of sonographer studies are closely monitored by faculty. Often the resident will ask for extender guidance; however, the nearby faculty may also “jump in” to the conversation if they sense that the resident is uncertain about an image or examination parameter. For the new faculty who are unfamiliar with local protocols, there is a brief observation period, and subsequently the extenders are readily available to explain the nuances of specific image requirements or parameters specific to a particular institution. This enables faculty from institutions less familiar with complex sonographic scenarios to rapidly ramp up to speed.
Advanced practice sonographers
Many medical specialties have benefitted from adding advanced practice providers to their ranks, including physician assistants and nurse practitioners, extending the breadth of what a single physician may be able to accomplish on their own. Similarly, in US, the concept of a “sonographic physician’s extender” has emerged, albeit without a formal training program or certificate despite discussions within societies like the Society of Diagnostic Medical Sonography and AIUM. , Nevertheless, individual organizations have taken steps to elevate staff sonographers to roles that capitalize on their experience and dedication, enhancing their contribution to a busy US department beyond the limits of US examination performance. These roles, known by various titles such as US or Sonographer Practitioner, Sonographer Radiologist Assistant, Advanced Practice Sonographer (APS), or simply “super tech” or “quality assurance tech,” will be referred to as APS throughout this article.
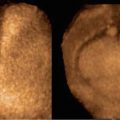
An APS can fulfill several roles within an US department, including: reviewing examinations for completeness, accuracy, and obtaining additional imaging as required before patients leave; serving as a scribe to create detailed sonographer notes or draft dictations for radiologists; assisting with advanced US applications including creating 3-dimensional (3D) reconstructions, performing musculoskeletal examinations, or functioning as the second pair of hands for a CEUS examination; reviewing examinations for site accreditation; and performing sonographer quality assurance. They can also participate in sonographer onboarding and training, assist with training on new technologies, and contribute to resident and fellow education. An APS may also facilitate US-related research and the development of new techniques or protocols. By performing these tasks, subspecialty US radiologists may not be physically needed at every site where high-level US or complex examinations are performed, allowing for greater flexibility in scheduling and site coverage.
US facilities interested in establishing APS positions must develop their own job description and requirements. Details that should be covered include years of experience since training (eg, minimum of 5, 8, or 10 years), number and type of registries held (covering all areas of the practice), and competencies in a variety of techniques (eg, elastography; musculoskeletal or obstetric US). Strong communication skills, teaching aptitude, and the ability to serve as liaison between sonographers and radiologists are essential qualities for prospective candidates. Although there may be theoretic concerns regarding interpersonal relationships between staff sonographers and an APS, this has not been reported in the literature, and in our experience, the sonographers value the APSs as a resource for education and more consistent workflow. Importantly, an APS is a great career opportunity for those with the passion and desire to advance beyond their position as a staff sonographer, allowing an experienced sonographer to continue working in clinically oriented activities, as opposed to seeking a purely administrative career path.
Budget allocation for APS salaries typically depends on their primary roles and responsibilities within the professional practice or imaging department administration. Some professional practices may cover the entire salary, allowing the APS to primarily work with radiologists in quality and report drafting tasks. Alternatively, imaging service lines may fund APS positions when administrative duties such as quality assurance, education, and accreditation are also included. Some institutions may adopt a cost-sharing model between professional and technical practices, tailoring responsibilities to meet both the radiologist and the imaging service line needs. While some institutions may establish specific full-time APS positions distinct from staff sonographers, others may integrate APS responsibilities into existing sonographer roles.
Ideally, an APS would have the depth and breadth of knowledge and experience to function at the level of a radiology senior resident or fellow, able to correlate US findings with other modalities such as CT or MRI, and review the electronic medical record for relevant medical or surgical history, medications, or specific risk factors. An APS can triage phone calls, and can be assigned the task of calling an ordering provider to collect pertinent information or even report critical results, under specific delegation from their supervising radiologist. An APS may also assist with complex or time-consuming examinations, such as those performed in the operating room or neonatal intensive care unit.
Previous studies have shown a very low significant discrepancy rate between an APS’s draft dictation and a radiologist’s final report. However, an APS cannot function independently as there is no national or even state-level registry or certification at this time. An APS is unlikely to obtain provider credentials within a hospital or organization, and therefore is unable to perform independent billable services. Therefore, all activities must be directly supervised by a radiologist, and no APS draft report may be viewable outside of the radiology department.
Regardless, the value of an APS to the modern US department is substantial. As techniques and technologies become more numerous and advanced, and the number of US-focused radiologists decreases relative to the number of US examinations being performed, an APS can be a critical and necessary solution to maintaining consistent and high-quality care. One author (DF) calculated that when looking at the time saved, 1 APS is equivalent to nearly one-third of a full-time radiologist, with his team of 4 APSs having drafted over 10,000 reports in 6 months, highlighting their significant contribution to departmental efficiency and productivity.
Picture archiving and communication system/artificial intelligence
Information Technology in the Ultrasound Facility
Information Technology (IT) plays a pivotal role in all phases of contemporary US. (Scanner-specific technologies such as advanced beamforming and image processing found in modern US platforms are beyond the scope of this discussion.) To understand how to best leverage IT in a US facility, it is instructive to consider the steps from when the patient’s examination is ordered and scheduled to when their sonogram is interpreted and a report is entered into the Electronic Health Record. Table 1 summarizes considerations for pre-scan preparation, image capture, and post scan activities. Additional considerations are as follows.
| Phase | Capability | What It Does | Advantages |
|---|---|---|---|
| Pre-scan | Scheduling software | Schedules US examinations based on available resources, patient/referrer preferences, and needs, and enables protocoling in advance | Boosts efficiency and satisfaction |
| DICOM modality worklist | Enters order/examination type and other information into scanner | Improves efficiency and reduces patient identification errors | |
| Display images from PACS on scanner | Enables viewing of prior imaging examinations before scanning | Facilitates localizing small lesions on US | |
| Scan | Annotation | Automatic labeling for protocol images and ad hoc labeling for non-protocol captures | Boosts efficiency |
| Transmission | Automatic sending images to PACS via a secure network, wirelessly for bedside examinations | Enables contemporaneous review by a physician, including for remote studies, lessening the need for re-scanning | |
| Post scan | Offline review workstation | Allows the sonographer to re-arrange images, change annotations, generate images from 3-D volumes, and selectively re-measure | Speeds image interpretation |
Image Storage and Export
All general-purpose Picture Archiving and Communication Systems (PACS) enable presentation of both static US images and cinematic (cine) clips for review, in addition to displaying prior sonograms and other imaging studies for comparison. Retrieval should be accomplished with minimal delay. Some departments may further benefit from a dedicated US PACS that offers functions such as simultaneous display of multiple clips (usually displayed in the chronologic order in which they were acquired), US-specific measurements, and tagging images for teaching or research. These systems are typically implemented in conjunction with a facility’s main PACS, and may leverage a single archive to avoid duplication of storage. Regardless, the software should allow static images or clips to be exported in common file formats without the patient’s name or other Protected Health Information.
Image Interpretation and Reporting
IT needs at this stage largely depend on how sonograms are read. Regardless, ready access to online informational databases and rapid access to ambulatory and inpatient notes, operative reports, and pathology results are essential to improve examination interpretation. If possible, these resources should be viewable on a monitor separate from the one used to display US images.
In many US facilities, particularly those associated with radiology departments and imaging centers, reports are generated using voice dictation software. These systems have progressed considerably over the past several decades, and now enable creation of structured reports that can later be mined for teaching, research, or quality control. Also, software that collects and organizes DICOM-SR (Structured Report) elements from the scanner enables automatic transfer of obstetric, vascular, and other US measurements into the structured report, decreasing reporting time and eliminating errors introduced by entering numbers manually. Some systems also apply quality checks during the reporting process. For example, they can automatically flag right/left or gender-related inconsistencies. These capabilities increase productivity by reducing the need to make corrections after the fact.
Artificial Intelligence
Available applications based on machine learning, deep learning, radiomics, and generative artificial intelligence (AI) in medical imaging have grown exponentially in recent years. Most current AI packages are deployed on PACS or other workstations, though some may be integrated into the US scanner itself.
While US has lagged somewhat because of the way sonograms are performed and reported, this is changing rapidly, and platforms that apply AI are beginning to move from proof-of-concept to clinical use in thyroid, liver, ovarian, breast, and vascular sonography. For example, AI software can provide decision support in categorizing nodules based on the ACR TI-RADS (Thyroid Imaging Reporting and Data System), or assist with ovarian follicle tracking in infertility patients, potentially boosting efficiency and accuracy. As well, generative AI is being used to create US reports, and large language models are being applied to mine the discrete data from free text dictations. Increasingly, AI is being used to optimize US scans in real time, including automatically adjusting grayscale or Doppler settings, or identifying and measuring common anatomic structures—these features may both improve a sonographer’s efficiency, and decrease inter-operator variability. Eventually, AI may be able to call the operator’s attention to abnormalities while a scan is being performed, reducing the likelihood of missing or not adequately imaging pathology. Several issues remain unresolved in AI applications. For example, how will AI be accepted and trusted if its inner workings are not well-understood by patients or physicians? Will inexperienced readers come to rely on the technology too much, and who will be liable if a physician does not accept AI’s conclusion, or accepts a spurious result, potentially leading to a poor patient outcome? Despite these challenges, the future of AI in augmenting US workflow and interpretation is bright.
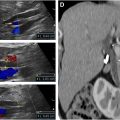
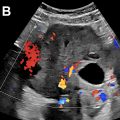
Offering new ultrasound examinations
Developing new US services are an integral component of keeping up with the latest technology and techniques, and can allow a site to even lead a rapidly developing field. US examinations these authors have brought to their respective US departments include CEUS, hemodialysis access and other innovative vascular studies, advanced 3D techniques, elastography, and fat quantification, among others. Importantly, potential referring services should be consulted regarding their interest in any new examination. After a thorough literature review and consulting other expert US departments, the team can establish an imaging protocol and determine the criteria used to evaluate the findings. Generally, at least 2 radiologists should be enthusiastic and knowledgeable about the new examination and interpretation. Thereafter, 2 to 3 sonographers should be identified as “experts” and teaching sessions provided. These sonographers can oversee the performance of the first few critical cases. Afterward, these experts can facilitate training of additional sonographers as needed, to further expand the new service.
Additional considerations include any special patient instructions such as any need to fast, who will place an intravenous line (in the case of CEUS), as well as average length of study. Scheduling review may include limiting new examinations to certain sites while experience is accumulating, or only on certain days when specific individuals are present and available. Where the examination will take place (inpatient vs outpatient), and whether it can be performed at multiple sites are also important considerations. We usually begin a new examination at one location, and then train additional personnel with the ultimate goal of performing a study enterprise-wide (liver elastography, for example). Other examinations that require local on-site expertise, such as availability of musculoskeletal radiologist experts, may still limit some US examinations to a particular site.
How the referring clinician will order the examination should be considered—in the case of an electronic ordering systems, the creation of a unique order, possibly with key words, order entry questions, and/or imbedded information may help passively educate ordering providers. In addition, knowing how an examination will be billed needs to be planned (ie, what Current Procedural Terminology [CPT] code(s) should be linked to the order).
Once the initial team is comfortable with the new technique, formal patient examinations can be scheduled, and the protocol can be refined. An active case review and quality assurance process should be implemented, and informative cases set aside. Thereafter, educational sessions should take place between physicians and sonographers to widen the pool of personnel that can perform and interpret the examination. Marketing and discussion with potential referring clinicians should continue to increase the number of patients referred.
Expanding to new ultrasound locations (clinic/hospital/freestanding emergency room)
The growth and expansion of a medical organization is invariably accompanied by increased imaging. During this growth, an imaging department should strive to provide consistent and high-quality imaging no matter where a patient may present. A patient undergoing imaging at a small, remote community center should receive the same quality service as a patient receiving care at an organization’s flagship hospital or central imaging site.
Adding a new site typically involves the prospective construction of a new location or acquisition and incorporation of an existing site. Both scenarios involve their own unique benefits and challenges. For instance, when an organization builds a new site, leaders can plan to purchase identical equipment and implement policies and protocols from existing sites—this facilitates uniformity and consistency. Alternatively, the acquisition of a new site may involve incorporating sonographers with variable levels of training or comfort with an organization’s preferred imaging protocols and workflow, as well as variability in scanner models and technological capabilities, which may prohibit certain services, such as liver elastography or 3D pelvic US. Administrators should strive to homogenize technology as much as is practical and feasible, allowing an organization to provide the same services at all locations, not only simplifying patient scheduling but making it more convenient for patients.
A robust sonographer onboarding and quality assurance program is of paramount importance to providing consistent and high-quality imaging across an enterprise. This may include training new sonographers at more central sites with more direct oversite before deploying them to new or remote sites. Completing a competency process where certain examinations are reviewed by a technical supervisor, APS, or radiologist may help ensure sonographers are ready for more independent work, as discussed in the training section aforementioned. Regardless, a central, easily-accessible database of imaging protocols and policies is essential—this “source of truth” can be referenced at any time from any site, and can be easily updated without having each site maintain their own protocol directory or binder, which risks becoming out-of-date.
Communication tools including PACS or institution-based messaging systems are useful for quick and efficient communication between sites. In addition, video chat tools that facilitate communication between a remote sonographer and their supervising radiologist or APS, some even available on the US systems themselves, may allow a radiologist’s real-time live review of an imaging study, ultimately improving patient care by ensuring protocol completeness.
Quality assurance
Ultrasound Performance and Review
The quality of an US study relies heavily on the sonographer’s experience, technical expertise, and attenuation to detail to a greater degree than for technologists in other imaging modalities. A QA program is a key to ensuring that studies are of consistent, reproducible quality. Physician or physician extender review of the US study prior to the patient leaving the US department is an important quality check. Most radiologists read USs from the PACS workstation regardless of the location where the US was performed.
Scanning Protocols
Standardized US scanning protocols list the required images (and often orientation, labeling, etc) and can reduce variability between sonographers. Facilities should create protocols customized to the needs of their practice. Protocols themselves should undergo periodic review and updates, can include example images of anatomy and pathology, and list diagnostic criteria (if applicable). These protocols should be stored in an easily-accessible location (preferably electronic, such as within an institution’s intranet site), such that sonographers at different locations have immediate access to latest updates. The AIUM and ACR practice parameters, and Society of Radiologists in Ultrasound (SRU) consensus documents provide an excellent basis for scanning protocols.
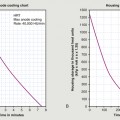
Scanner-based Protocols
Most equipment manufacturers now allow for protocols to be programmed directly into the scanner, allowing the device to guide a sonographer through the requisite images, automatically labeling images and launching features such as color or spectral Doppler at the appropriate point in the protocol. This can be particularly useful for examinations that may not be as common, in which images may be inadvertently forgotten. These “on-cart” protocols make it easier for new sonographers to perform US examinations at the expected level for the department and national accrediting standards. Image-based protocols may also decrease the length of time it takes to perform the examination, as standard protocol images are already labeled as per facility requirements. Protocols also make physician review easier as specific images are located in the same point in the examination, making dictation and comparison with prior studies easier.
Infection Control
Outbreaks of infection have resulted from contaminated transducers and US gel. Facilities should develop infection control procedures based on Center for Disease Control and Prevention and Joint Commission guidelines. These should include handwashing, use of gloves, and policies for cleaning US equipment ( Table 2 ). The date/time of disinfection for every transducer should be documented. To prevent reinfection, there should be policies regarding storage and separation of clean from dirty transducers. Special protocols are required for interventional procedures ( Table 3 ).