Figure 5-1. Normal ACJ. Schematic drawing of an anterior view of the right shoulder. The normal ACJ contains a variable intra-articular disk that ranges from [A] complete [B] to meniscoid-like appearance.
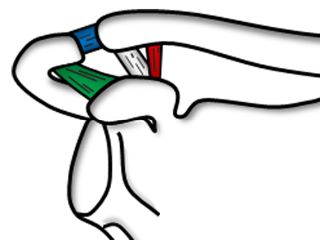
Figure 5-2. ACJ supporting ligaments. Schematic drawing of an anterior view of the right shoulder. The coracoclavicular ligament is composed of the conoid (red) and trapezoid (gray) ligaments. Blue= intrinsic acromioclavicular ligaments. Green= coracoacromial ligament.
The intrinsic acromioclavicular ligaments provide 90% of the constraint to horizontal motion of the ACJ and are the greatest restraint to joint displacement in the anterior and posterior directions.9 A cadaveric study has shown that the intrinsic superior ligament accounts for 56% of resistance against posteriorly directed force, with the posterior ligament accounting for 25%.10 In contrast to the intrinsic ligaments, the coracoclavicular ligament is vital to vertical stability of the joint.11 The conoid ligament plays a key role in constraining anterior and superior displacement of the clavicle, while the trapezoid is a critical stabilizer in axial compression toward the acromion process.12 The coracoclavicular ligament is also critical by attaching the clavicle to the scapula because the clavicle itself is widely movable during shoulder flexion and abduction; by linking scapulohumeral motion to scapulothoracic motion, the coracoclavicular ligament allows the scapula to rotate downward as the clavicle rotates upward, a phenomenon commonly referred to as synchronous scapuloclavicular motion, thus restricting movement at the ACJ.3
1.1. Sonographic Technique
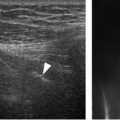
The ACJ is best assessed on long-axis images using high-frequency linear-array probes. Standard protocol includes both static and dynamic evaluation.13 Static images are obtained having the arm relaxed along the body or with the forearm supinated on the thigh, while dynamic provocative stress testing is completed during active forward flexion of the shoulder with pronated forearm. The joint is assessed for bone contours, interosseous distance, and distension of the articular capsule. The adjacent articular surfaces of both the acromion and clavicle have a smooth, rounded configuration at the margins of the joint (figure 5-3). The joint slopes inferomedially, so clavicle is usually identified in a slightly higher position when compared to the acromion, but this finding is variable.14 A minimal submillimetric change in ACJ alignment is expected during provocative manoeuvers and should not be confused with pathology. Although several biometric measurements are available,15 we do not rely on mathematical criteria to define pathology and consider numbers only as adjuvants when assessing ACJ for disease.16 The whole acromion process must be scanned, not only the distal aspect, because an os acromiale-clavicle joint may simulate the ACJ (see figure 7-2). Meticulous technique is also necessary in trauma setting since distal clavicle fractures may likewise mimic the appearance of an abnormal ACJ (figure 5-4).
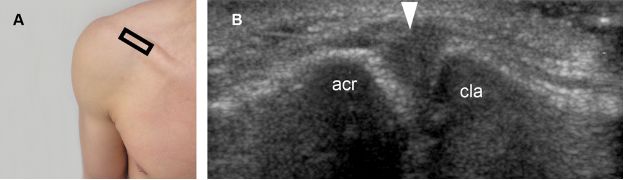
Figure 5-3. Normal ACJ. [A] Positioning of the probe. [B] Corresponding long-axis 12-5 MHz US image shows normal acromion (acr), clavicle (cla), and joint capsule (arrowhead).
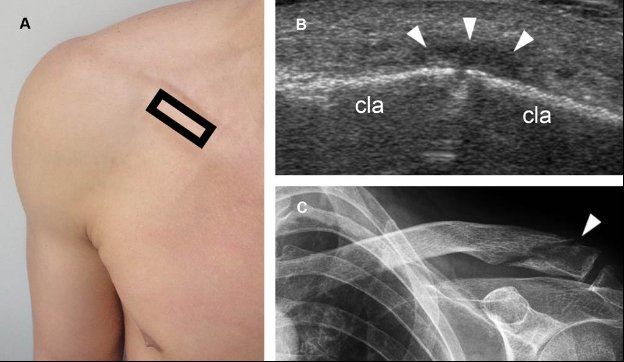
Figure 5-4. Distal clavicle fracture. [A] Positioning of the probe. [B] Corresponding long-axis 12-5 MHz US image shows cortical disruption of the clavicle (cla) associated with localized periosteal reaction (arrowheads). This finding may mimic an abnormal ACJ to the inexperienced examiner. [C] Corresponding radiography confirms distal clavicle fracture (arrowhead).
1.2. Spectrum of Findings
The most common findings are joint space narrowing and marginal osteophytes secondary to osteoarthritis. If there is widening of the ACJ, considerations include inflammation and trauma. Distal clavicle resection may mimic widening of the ACJ, but a careful clinical history usually suffices to reach the correct diagnosis (figure 5-5). Isolated distension of the articular capsule with no concomitant widening of the joint space or marginal cortical irregularities may correspond to the geyser sign, a finding related to communication between the glenohumeral joint, the subacromial-subdeltoid bursa, and the ACJ secondary to a full-thickness tear of the rotator cuff (see figure 1-61).
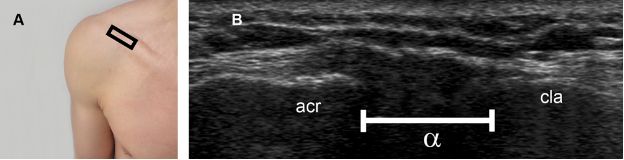
Figure 5-5. Distal clavicle resection. [A] Positioning of the probe. [B] Corresponding long-axis 12-5 MHz US image shows abnormal interosseous space (α) secondary to distal clavicle resection. Acr= acromion. Cla= clavicle.
1.2.1. Degenerative and Inflammatory Joint Disease
Osteoarthritis is only one of the many terms used interchangeably to refer to degenerative joint disease.17 It is the most prevalent musculoskeletal condition in developed countries and the most common cause of pain related to the ACJ, but may also be depicted in asymptomatic individuals.18-20 Sonographic findings include joint space narrowing, distended joint capsule, hyperemia, and marginal osteophytes (figure 5-6). The grading of the severity is rather subjective and made according to the degree to which the various features are present. However, the terminology used to describe these findings deserves special considerations. Whereas we have a legitimate responsibility to report what we see, we also have a responsibility to avoid unnecessary and counterproductive lexicon. The term osteoarthritis and its correlates may be unnecessarily emotive and compromises the management of patients with shoulder pain. The clinical significance of degenerative changes lies not in the changes themselves but in what precipitates them.21 Sometimes the causes are clinically significant, such as when the changes are a manifestation of a systemic, metabolic disorder. Clinical significance fades away when the changes are no more than a correlate of age in individuals with no history or clinical findings suggestive of ACJ disorder. In the latter situation, a simpler and accurate term is normal age changes. Degeneration of the ACJ is mostly a natural consequence of aging, starts as early as in the second decade, and become ubiquitous with advancing age.22
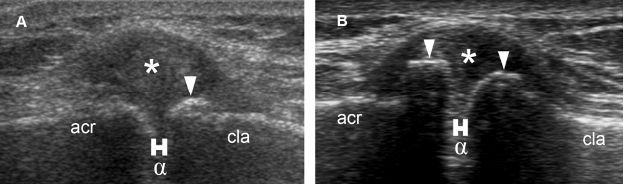
Figure 5-6. ACJ osteoarthritis. Long-axis 12-5 MHz US image shows [A] mild and [B] moderate osteoarthritic changes. Note joint space narrowing (α), distended joint capsule (asterisk), and marginal osteophytes (arrowheads). Acr= acromion. Cla= clavicle.
Widening of the ACJ and cortical irregularities of the distal clavicle and adjacent acromion outside the trauma setting should raise the suspicious for inflammatory conditions such as infection or rheumatoid arthritis. It is estimated that two-thirds of the patients with rheumatoid arthritis show involvement of the ACJ after 15 years. ACJ infection is more common in intravenous drug users. Osteolysis of the distal clavicle should be included in the differential diagnosis of degenerative and inflammatory joint disease when cortical erosions are present only at the clavicular margin of the joint (see section 1.2.3).
1.2.2. Ganglion
The ACJ ganglion is a common benign pseudocystic lesion filled with gelatinous material that communicates with the joint space.23-25 The wall of these lesions is composed of multidirectional strata of collagen and has no synovial membrane.
According to a review article published in 2010, forty-one cases of ACJ ganglion have been described, and most occurred in patients with an associated rotator cuff tear.26 However, available data from case reports is limited and most studies lack histopathological correlation or include overdistended ACJ in the definition of ganglion. In the following paragraphs, we only consider ganglion as a synonymous with lesions eccentrically located in relation to the joint space.
The pathogenesis of ACJ ganglion is enigmatic, and three proposed mechanisms derive from the observation of lesions located elsewhere in the body. In the first proposed mechanism, joint abnormalities lead to altered biomechanics, weaken the joint capsule, and eventually cause leakage of intra-articular fluid into the periarticular tissue. Intra- and extra-articular fluids communicate via a pedicle, which contains a one-way valve mechanism. Such a one-way valve is thought to result from a number of microcysts that communicate with the primary ganglion and are present in the tissue surrounding the tortuous pedicle lumen.27 Subsequent reaction between extra-articular fluid and the periarticular tissue encapsulates fluid and forms the wall of the ganglion.28 In the second proposed mechanism, the ganglion results from an extra-articular degenerative process and the gelatinous material represents the final end-product of a myxoid change in collagen or connective tissue that subsequently forms a pedicle and communicates to the joint.28 Lastly, in the third proposed mechanism, joint stress stimulate hyaluronan secretion by the mesenchymal cells located adjacent to the joint capsule. These cells are widely distributed in adult connective tissues and are also responsible for the formation of joint capsules and bursae.29 The accumulation of fluid eventually induces the formation of a pseudocapsule lined by collagen from compression of surrounding tissues. As none of these mechanisms individually explain all of the known features of ACJ ganglia, their origin is thought to be multifactorial and defined on a case-by-case analysis.
ACJ ganglion typically presents as a painless enlarging mass depicted as anechoic lesion adjacent to the ACJ (figure 5-7). Atypical findings such as thick walls and septations are not uncommon. Internal low-level echoes represent artifact, hemorrhage, or the relative proportion of the constituents of mucin that may change with the age of the ganglion.30,31 Acoustic enhancement is described but particularly difficult to demonstrate because most lesions are small and located close to the bone.
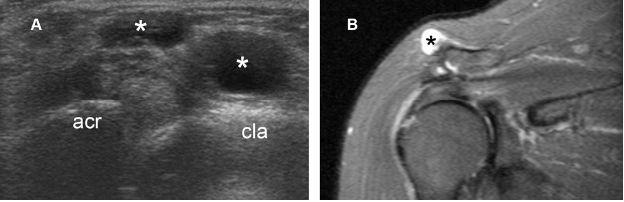
Figure 5-7. ACJ ganglion. [A] Long-axis 12-5 MHz US image shows a multiloculated ganglion (asterisks) adjacent to the ACJ. [B] Corresponding coronal oblique STIR MRI confirms sonographic finding. Acr= acromion. Cla= clavicle.
The differential diagnosis of a palpable lump located over the ACJ includes osteophytes (figure 5-8), synovial cysts, and supra-acromial bursitis. Synovial cysts are a simple herniation of the joint capsule and distinguished from ganglia on the basis of the presence of a synovial membrane, but these terms are loosely applied because imaging findings are similar and secondary changes in the capsule may make histologic differentiation difficult, if not impossible.32 Both ganglia and synovial cysts may communicate with the ACJ and this finding does not help in differentiating between these two lesions. However, this information should always be reported to the referring physician because failure to resect such a communication invariably leads to recurrence.33-35 On daily practice, we liberally use the term ganglion as a descriptive, not histopathological diagnosis. It should be emphasized that since ganglia has no epithelial lining, these lesions are actually pseudocysts, not true cysts.
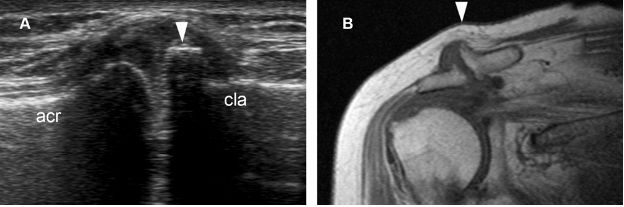
Figure 5-8. ACJ osteophyte. [A] Long-axis 12-5 MHz US image shows an exuberant ACJ osteophyte (arrowhead). [B] Corresponding coronal oblique T1-weighted MRI confirms the exuberant osteophyte causing a palpable lump over the ACJ (arrowhead). Acr= acromion. Cla= clavicle.
Studies on the natural history of untreated ACJ ganglia are lacking. Anecdotal experience suggest that changes in volume are common and at least one case in the literature refers spontaneous resolution.36 Needle aspiration or surgical removal of these ganglia may be tricky and results in unpredictable outcomes without addressing the underlying pathological process.
1.2.3. Osteolysis of the Distal Clavicle
Osteolysis of the distal clavicle (ODC) is a rare but under-recognized condition that typically follows minor repetitive injuries such as in weight training. However, it may also occur several years after a single episode of trauma and should be included in the differential diagnosis when a patient experiences point tenderness over the ACJ beyond the acute phase of the injury. When secondary to chronic repetitive injuries, pain begins insidiously and may occur only with the precipitating activity. The etiology remains unclear, although osteochondral lesion followed by synovial invasion is a common hypothesized mechanism. Radiographic evaluation may be misleading if only standard anteroposterior views are obtained because the inferior portion of the distal clavicle is obscured by the spine of the scapula. Hence, in suspected ACJ disease, radiographic series should include an anteroposterior view at 10-15° cephalic angulation (Zanca view) to better delineate the joint.
US readily depicts resorption of the distal clavicle as irregular cortical erosions, whereas the acromion remains intact (figure 5-9). Associated findings may include distended joint capsule, soft-tissue swelling, and joint instability. Management of ODC is initially conservative and surgery typically reserved for refractory cases.
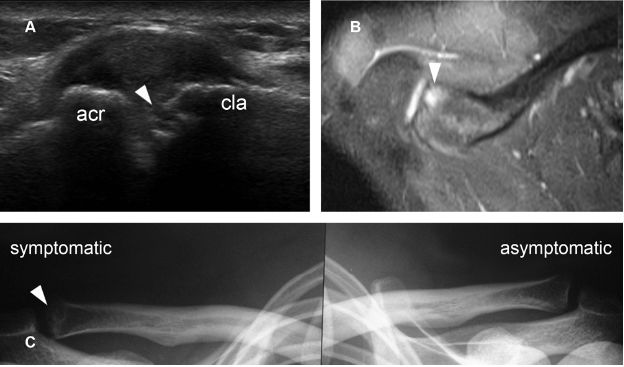
Figure 5-9. Osteolysis of the distal clavicle. [A] Long-axis 12-5 MHz US image shows irregular cortical erosion at the distal clavicle (arrowhead). [B] Corresponding axial STIR MRI shows abnormal signal intensity at the distal clavicle (arrowhead). [C] Corresponding radiography demonstrates ODC in the symptomatic side (arrowhead). Acr= acromion. Cla= clavicle.
1.2.4. Traumatic Dislocation
Traumatic ACJ dislocation has been described since the time of Hippocrates and results from a sprain or a tear in supporting structures.37 It usually develops from direct trauma and tends to occur in younger physically active individuals. Tossy originally classified ACJ dislocation into three types: mild, moderate, and severe.38 Subsequently, the Tossy classification was expanded by Rockwood to include subtypes of severe dislocation and became the most commonly used classification system to define management (figure 5-10).39
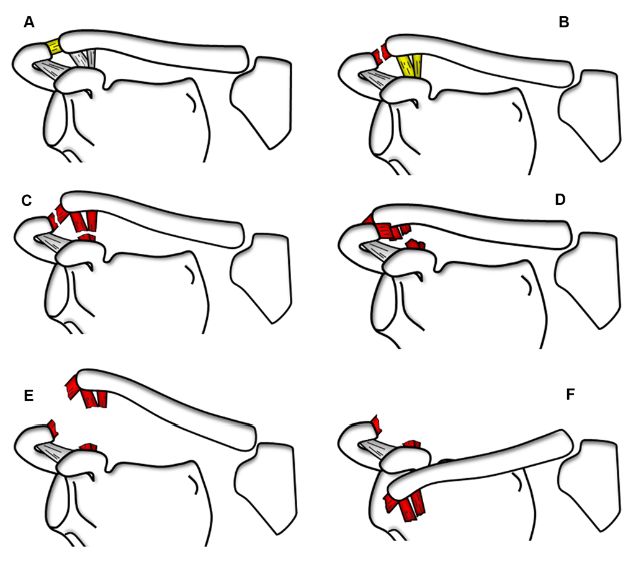
Figure 5-10. Rockwood classification of ACJ dislocations. Schematic drawing of an anterior view of the right shoulder. [A] Grade 1 dislocation. Partial tear of the acromioclavicular ligaments. [B] Grade 2 dislocation. Complete tear of the acromioclavicular ligaments and superior displacement of clavicle. [C] Grade 3 dislocation. Complete tear of the acromioclavicular and coracoclavicular ligaments plus superior displacement of clavicle and complete loss of contact between clavicle and acromion. [D] Grade 4 dislocation. Complete tear of the acromioclavicular and coracoclavicular ligaments plus posterior displacement of clavicle into or through the trapezius muscle. [E] Grade 5 dislocation. Complete tear of the acromioclavicular and coracoclavicular ligaments plus superior displacement of clavicle and complete detachment of deltoid and trapezius from distal clavicle. [F] Grade 6 dislocation. Complete tear of the acromioclavicular and coracoclavicular ligaments plus clavicle displaced inferior to acromion and coracoid process. See table 5-1 for details.
Investigation of suspected ACJ dislocation traditionally involves conventional radiographs because they are widely available and clearly demonstrate moderate and severe lesions, though it has limitations to diagnose mild injuries. In addition to conventional radiographs, weight-bearing views may be used to better differentiate between moderate and severe dislocations, but the evidence for this is controversial40 and some authors recommend that routine use of this technique be abandoned.41
US is also useful for diagnosis and classification of ACJ dislocation according to the well-established Rockwood system (table 5-1). The primary diagnostic criteria are capsular thickening, abnormal alignment of bony structures, and widening of the joint space. In order to objectively assess these findings, bilateral evaluation should be performed to provide a standard reference for the normal ACJ in the uninjured shoulder. The acromioclavicular index is helpful to evaluate joint space widening, and calculated by dividing the acromioclavicular distance on the contralateral asymptomatic side by that on affected side.38 It is important to recognize that the ACJ space is slightly wider anteriorly than posteriorly, and contralateral comparison should be made only at similar levels. In grade 1, or mild dislocation, the acromioclavicular index is close to 1.0, the intrinsic acromioclavicular ligaments are sprained, and the coracoclavicular ligament is intact (figure 5-11). In grade 2, or moderate dislocation, the acromioclavicular index is close to 0.5, the intrinsic acromioclavicular ligaments are completely torn, and the coracoclavicular ligament is intact or sprained (figure 5-12). Grades 3, 4, 5, and 6 have the acromioclavicular index close to 0.25 and are considered severe dislocations as both intrinsic acromioclavicular and coracoclavicular ligaments are completely torn (figure 5-13). The coracoclavicular index is utilized to differentiate between different subtypes of severe dislocation and obtained in a similar way to the method used to calculate the acromioclavicular index (i.e. by dividing the coracoclavicular distance on the contralateral asymptomatic side by that on affected side). In grade 3 dislocation, coracoclavicular index ranges between 0.8 and 0.5 (figure 5-14); in grade 4, coracoclavicular index may be 1.0 since clavicle is dislocated mainly posteriorly; in grade 5, coracoclavicular index is lower than 0.5 (figure 5-15); in type 6, coracoclavicular index is negative because clavicle is dislocated inferior to the coracoid process. Doppler US may be used to increase diagnostic confidence to detect low-grade injuries because it depicts reparative process to injured ligament (video 5-1). Detection of undissolved gas also increases diagnostic confidence as it is usually associated to ACJ distraction (see section 1.2.7).
Table 5-1. Rockwood classification of ACJ dislocations adapted for US. See text for details.
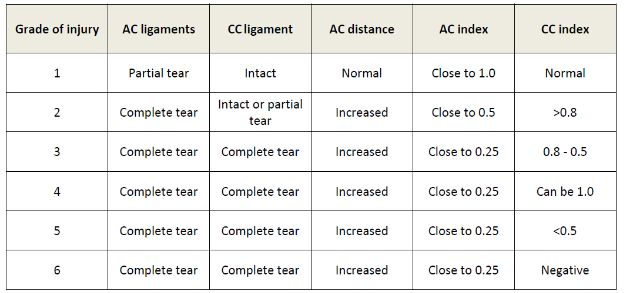
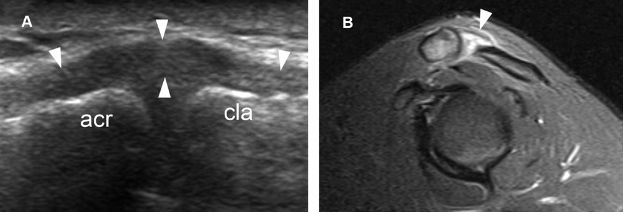
Figure 5-11. Grade 1 traumatic dislocation of the ACJ. [A] Long-axis 12-5 MHz US image shows capsular thickening secondary to sprain of the intrinsic superior acromioclavicular ligament (arrowheads). The intrinsic acromioclavicular ligaments cannot be differentiated from the joint capsule at US. [B] Corresponding sagittal STIR MRI confirms sonographic finding. Acr= acromion. Cla= clavicle.
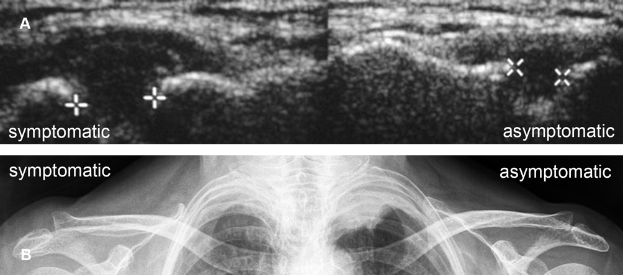
Figure 5-12. Grade 2 traumatic dislocation of the ACJ. [A] Comparative long-axis 12-5 MHz US image shows abnormal widening of the ACJ in the symptomatic side (cursors). The acromioclavicular index is estimated at 0.6. [B] Corresponding radiography confirms sonographic finding.
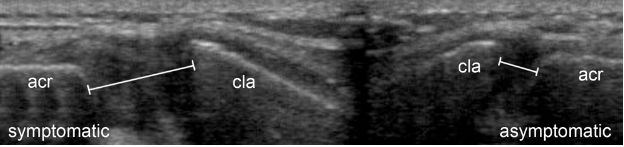
Figure 5-13. Severe traumatic dislocation of the ACJ. Comparative long-axis 12-5 MHz US image depicts abnormal widening of the ACJ and superior displacement of clavicle in the symptomatic side. The acromioclavicular index is estimated at 0.3. Acr= acromion. Cla= clavicle.
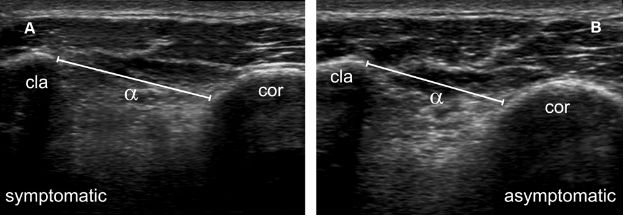
Figure 5-14. Grade 3 traumatic dislocation of the ACJ. [A,B] Comparative 12-5 MHz US image shows mild superior displacement of the clavicle in symptomatic side and coracoclavicular index (αB/αA) estimated at 0.8. Cla= clavicle. Cor= coracoid.
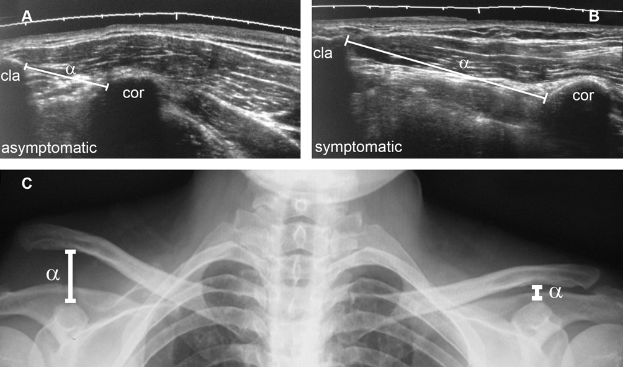
Figure 5-15. Grade 5 traumatic dislocation of the ACJ. [A,B] Comparative extended field of view 12-5 MHz US image shows superior displacement of the clavicle and 200% increase in coracoclavicular distance (α) in symptomatic side. [C] Corresponding radiography confirms superior displacement of the clavicle and coracoclavicular index estimated at 0.3.
Chronic sprains of the intrinsic acromioclavicular ligaments may show varying degrees of calcification (figure 5-16). Such calcifications may be demonstrated as intraligamentous during dynamic evaluation (video 5-2). This finding must be differentiated from small avulsion fractures of the distal clavicle, which are depicted occasionally as an associated finding (figure 5-17). Pleomorphic calcifications must also be differentiated from chondrocalcinosis (see section 1.2.6).
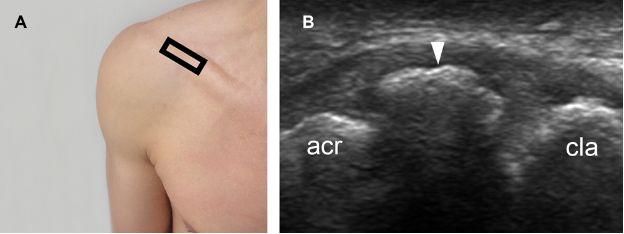
Figure 5-16. Chronic calcified lesion of the superior acromioclavicular ligament. [A] Positioning of the probe. [B] Corresponding long-axis 12-5 MHz US image shows an arciform calcification of the superior acromioclavicular ligament (arrowhead). Acr= acromion. Cla= clavicle.

Figure 5-17. Small avulsion fracture of the distal clavicle. [A] Long-axis 12-5 MHz US image shows a small avulsion fracture of the distal clavicle (arrowhead). [B] Corresponding radiography confirms sonographic finding (arrowhead). Acr= acromion. Cla= clavicle.
Most cases referred for US in acute trauma setting consist of minor (grade 1) injury with missed or overlooked findings on radiographs. Dynamic US is critical to detect such mild dislocations, especially because they may present as a normal joint in static images. The degree of bone displacement during dynamic evaluation is proportional to the severity of ligament injury, and mild dislocation (video 5-3) shows less instability than moderate (video 5-4) or severe dislocations (video 5-5).
Management for mild (grade 1) and moderate (grade 2) dislocations is usually conservative. Early surgical intervention for acute grade 4, 5, and 6 dislocations is indicated due to the significant morbidity associated with joint instability. The treatment of grade 3 lesions is controversial, although surgery is probably best reserved for those injuries that fail to respond adequately to conservative management.
1.2.5. Joint Instability
Although traumatic ACJ dislocation and joint instability often coexist, they are not synonyms because mild instability may also occur secondary to atraumatic degenerative or inflammatory joint disease.
1.2.6. Chondrocalcinosis
Chondrocalcinosis is a generic term referring to visible calcification within fibrocartilage or hyaline cartilage structures. Calcific deposits may comprise calcium pyrophosphate dihydrate crystal (most common), dicalcium phosphate dihydrate, calcium hydroxyapatite crystals, or a combination of these.42,43 Specific data on the prevalence ranges widely, depending on the demographics and methods used to detect the calcium deposits. However, it is well known that chondrocalcinosis is an age related disorder and occurs most often in elderly individuals.44,45 There is also a positive association between chondrocalcinosis and osteoarthritis, but chondrocalcinosis does not appear to be a risk factor for subsequent cartilage loss.47
The term chondrocalcinosis sometimes is misapplied as a synonym for calcium pyrophosphate deposition disease (CPPD), but, technically, it refers generically to the presence of calcific deposits. CPPD is only one of the many causes of chondrocalcinosis, and WHIP A DOG is a mnemonic commonly used to recall the differential diagnosis (table 5-2).46 Although not considered a primary diagnostic modality to evaluate cartilaginous abnormalities, US may depict chondrocalcinosis as echogenic foci within the cartilage with no acoustic shadow (figure 5-18). Management is directed to the underlying pathological process.
Table 5-2. Mnemonic commonly used to recall the differential diagnosis of chondrocalcinosis.
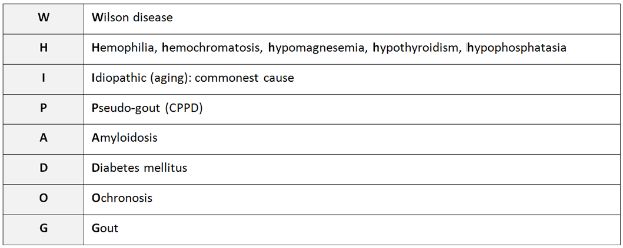

Figure 5-18. ACJ chondrocalcinosis. [A] Long-axis 12-5 MHz US image depicts echogenic foci within the cartilage with no acoustic shadowing (arrowheads). Note also normal superior acromioclavicular ligament (asterisks). [B] Corresponding radiography confirms ACJ chondrocalcinosis. Acr= acromion. Cla= clavicle.
1.2.7. Undissolved Gas and Vacuum Phenomenon
Undissolved gas is known to occur in joints placed under negative tension because viscosity of synovial fluid retards the flow of fluid into the widening gap, leading to vacuum phenomenon and attracting gases from surrounding tissues into the joint space.48 A second and rare cause are pyogenic infections, especially with gas-forming organisms.49,50 The undissolved gas is usually considered nitrogen or carbon dioxide and may persist in suspension in the synovial fluid.51,52 Spherical bubbles are unstable and have short lifetime because surface tension raises internal pressure in the bubble as described by Laplace law.53
Irrespective of the mechanism of formation, undissolved gas is readily depicted on radiographs as a radiolucent stripe. At US, it is detected as bright echogenic microfoci (figure 5-19). The acoustic mismatch between gas and surrounding tissues is so great that virtually all of the sound is reflected and bounces around generating multiple bright echo tails with different periods of occurrence and different strengths deep to the echo from the gas interface. This has been called a dirty shadow as opposed to the clean shadow deep to bone or other structures that absorb sound. In the absence of penetrating trauma or infection, undissolved gas is a reliable indicator of ACJ distraction in both static and dynamic evaluation (video 5-6).
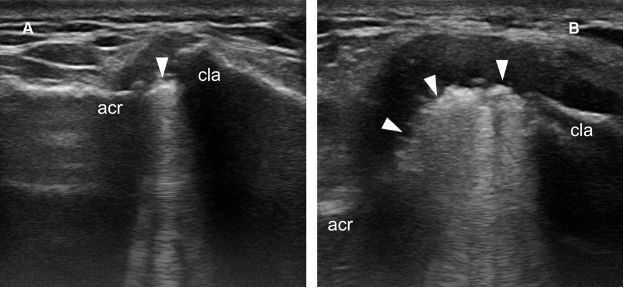
Figure 5-19. Undissolved gas within the ACJ. [A] Baseline long-axis 12-5 MHz US image shows echogenic foci casting dirty shadow within the ACJ (arrowhead). Note also superior migration of the clavicle suggesting dislocation of the ACJ. [B] Corresponding 12-5 MHz US image obtained during provocative manoeuver demonstrates widening of the joint space secondary to dislocation of the ACJ and more readily detectable gas within the joint space (arrowheads). Acr= acromion. Cla= clavicle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree