ACUTE AND SUBACUTE MANDIBULAR AND DENTAL INFECTIONS AND NONINFECTIOUS INFLAMMATORY CONDITIONS
KEY POINTS
- Imaging beyond plain films should be used in patients who are suspected of disease that has spread beyond the dental arches. This is typical done with computed tomography.
- Advanced imaging with computed tomography is critical in identifying complications such as spreading infections that occasionally might be life threatening and underlying associated osteomyelitis.
- Imaging can identify underlying causative or alternative conditions that may significantly affect medical and surgical decision making.
INTRODUCTION
Etiology
The vast majority of mandibular infections are of odontogenic origin. Likewise, the vast majority of head and neck abscesses outside of the orbit and temporal bone have the mandibular dentition as a source. Tooth-related infections that result in facial abscess are much less commonly related to the teeth of the maxillary alveolus. However, maxillary tooth-related infections do precipitate maxillary sinus sequelae, facial swelling with orbital extensions, endoantral syndrome, and possibly even cavernous sinus thrombosis.
Some of the mandibular tooth infections arise from within the dental pulp, leading to periapical inflammatory disease, or from periodontal disease. Periapical inflammatory disease in teeth, depending on the virulence of the organisms involved and the host immune response, results in apical lucencies (rarefying osteitis), including periapical abscess, granuloma, and cyst. Usually, if unattended to or untreated (Figs. 97.1 and 97.2), periapical inflammatory disease expands into the body of the mandible and produces subsequent complications. From there, the process can erode through the cortices into the subperiosteal layer and/or surrounding soft tissues resulting in osteomyelitis, cellulitis, or jaw trismus and eventually spreading into floor of the mouth and fascial spaces as an abscess and sometimes the skin as a fistula (Fig. 97.3).
These are mainly bacterial infections, both anaerobic and aerobic, although fungal disease is possible. Dental infections run a full range of relatively indolent processes to fulminate in necrotizing fasciitis (Figs. 13.1, 13.2, and 13.6).
The noninfectious inflammatory disease that tends to involve the mandible is Langerhans cell histiocytosis (LCH).
Prevalence and Epidemiology
These infections are sporadic infections that occur primarily in immune-competent adults and older children. The infections tend to be more aggressive in diabetics and in more severely immune-compromised patients.
Clinical Presentation
Patients with uncomplicated mandibular and dental infections present with jaw pain, perhaps more generalized facial pain, and possibly fever. Acute spreading bacterial infection with an abscess becomes much more likely when the maxillary or mandibular dental pain progresses rapidly and on physical examination when there is clinical evidence of facial cellulitis.
PATHOPHYSIOLOGY
Anatomy
The anatomy of the maxilla (Chapter 78) and mandible (Chapters 78 and 96) and related dentition (Chapter 96) must be completely understood. In addition, the spreading infections with related abscesses require detailed knowledge of the relationship of the mandible and maxilla and their subperiosteal space to the floor of the mouth (Chapter 196) and masticator (Chapter 145) and submandibular spaces (Chapter 175) primarily and then all of the other potentially interconnected deep spaces of the suprahyoid and infrahyoid neck (Chapters 142 and 149).
Pathology and Patterns of Disease
Dental Infections
The pathophysiology of dental and other infection including possibly related osteomyelitis is described in general in Chapters 13 and 14 (Figs. 13.1, 13.2, and 13.6). These infections must sometimes be differentiated from osteonecrosis (most commonly radiation induced), bisphosphonate osteonecrosis (BON), and neuralgia-inducing cavitary osteonecrosis (NICO) discussed in Chapters 14 and 43 (Figs. 14.1, 14.19, and 43.6).
Pyogenic dental infections that progress to the point where advanced imaging is indicated should be considered akin to an abscess or empyema since it is essentially a collection of pus under pressure even when confined to the periapical region. It is this fundamental situation that creates the potential for the periapical or periodontal infection to spread beyond the maxilla and mandible (Figs. 97.1–97.3). The pressure and local toxicity of the pyogenic material encourages bone resorption with eventual buccal or lingual cortical breakthrough and then subperiosteal accumulation of pus. Eventually, the pus will breach the periosteum and spread in adjacent and then more remote spaces (Figs. 13.1, 13.2, 13.6, 97.1, and 97.3). Since pressure is a driving force of these destructive and dissecting collections of pus, relieving this pressure by draining the causative dental abscess as soon as possible is the essential strategy aimed at the treatment and prevention of what can become life-threatening spread of the infection. This strategy usually begins and ends with extraction of the offending tooth but often requires more extensive drainage. The spread pattern is directed first by the point where the pus leaves its bony confines (Figs. 13.1, 13.2, 13.6, 97.1, and 97.3). The point of penetration has a relationship first with the subperiosteal space and then with the facial boundaries of the masticator, buccal, and/or submandibular spaces. The pus may travel some distance in the subperiosteal space before it breaks out; thus, the initial space involved may not necessarily be the one most contiguous with the bony defect (Fig. 97.4). Also, remote subperiosteal spread may be a mechanism for involvement of more than one space being involved at initial presentation. Imaging provides the map for the drainage procedure (Figs. 13.1, 13.2, 13.6, and 97.5).



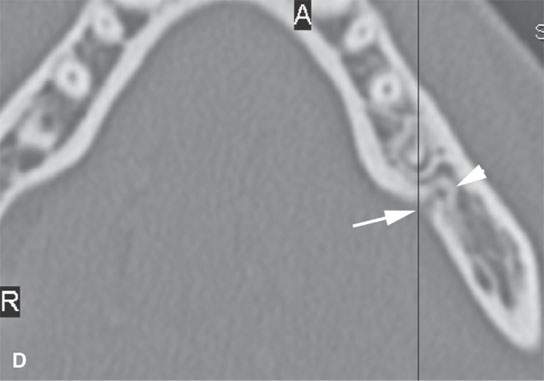
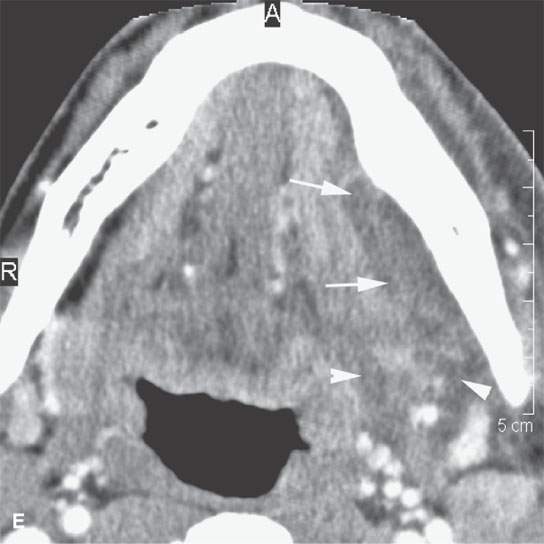
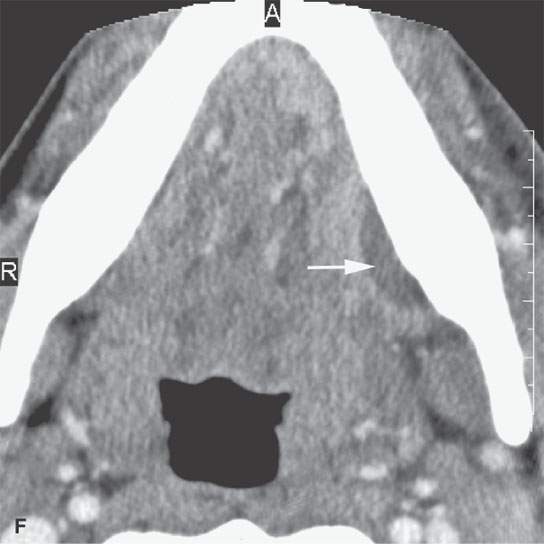
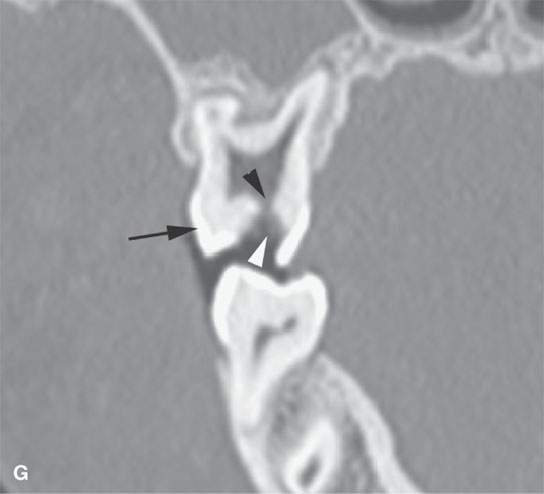
FIGURE 97.1. Contrast-enhanced computed tomography of a patient with endodontal disease demonstrating the pathophysiology of how such disease can result in spreading abscess beyond the mandible. A: Gross endodontal disease (arrowhead) penetrating into the pulp cavity. There is secondary periapical change (arrowheads) related to the spread of disease through and possibly around the tooth. B: Oblique reformation showing the periapical disease penetrating the cortical surface of the mandible (arrow). C: Coronal reformation showing this tract of infectious disease penetrating inferiorly and medially (arrow). D: Axial view showing the defect in the lingual plate of the mandible (arrow) communicating with the periapical changes (arrowhead). E: A secondary subperiosteal abscess (arrow) resulted from this periapical infection. In this image, the abscess is fairly mature. F: A section somewhat lower showing spreading phlegmon beginning to organize into a submandibular space abscess (arrows) and less well organized more posteriorly (arrowheads). The more posterior disease is spreading into the parapharyngeal space and on its way to the deep neck. G: An image from a different patient showing earlier endodontal disease. The crown of this tooth (black arrow) is eroded by a cavity (white arrowhead) that penetrates the dentin to enter the pulp cavity (black arrowhead).
With acute infections resulting from a nonvital pulp that was exposed to dental caries, no notable radiographic features may be seen in the periapical region. A marginal widening of the apical periodontal ligament space sometimes may be noted (Fig. 97.1A). With irreversible pulpitis, the patient presents with lingering pain in response to cold. Endodontic assessment is carried out, and appropriate endodontic interventional procedures are instituted to remove the necrotic pulp and infected material, followed by obturation of the root canal system. Pressure relief through the root canal system usually alleviates the severe pain associated with this condition.
More indolent infections such as those that are partially treated, due to unusual organisms such as actinomycosis, or due to fungi may produce tracts from the point of bone breakout to deep spaces and perhaps a sinus tract to the skin. In an immune-competent patient, it is unusual for a fungal infection to produce extensive soft tissue fluid collections (Figs. 13.1, 13.2, 13.6, and 97.3).
The most important acute complication of these infections is airway compromise (Fig. 97.5A–D). Also important is the potential that the infection is potentially very aggressive or that it might threaten vital structures such as the orbit and eye (Fig. 97.6). Osteomyelitis is a potential subacute or delayed complication of dental infections. In more indolent infections, a well-established osteomyelitis can actually be the source of a spreading abscess. The presence of osteomyelitis will alter therapy (Figs. 14.12, 14.14–14.16, 4.19–14.21, and 97.7A–F). Osteomyelitis must be differentiated from osteonecrosis (most commonly radiation induced ORN), BON, and NICO (Figs. 14.1, 14.12, 43.6, and 97.7G–K and Chapters 14 and 43); this is usually accomplished by a combination of the clinical setting and imaging findings.1–3 Osteomyelitis may complicate ORN, BON, and NICO (Fig. 97.7F–I).
Noninfectious Inflammatory Diseases
The mandibular involvement in LCH reflects it being a systemic disease that involves histiocytes populating bone3 (Fig. 97.8). Mandibular sarcoidosis is a rare and isolated manifestation, but skeletal involvement with sarcoidosis reflects its systemic nature.4 Sarcoidosis and LCH are infiltrating marrow space processes.5 Wegener granulomatosis (WG) typically involves the bone secondarily from a gingival starting point.6
All produce potentially aggressive-appearing bone loss and may involve surrounding soft tissues but will not result in abscess unless secondarily infected. These diseases may mimic both osteomyelitis and the primarily nonodontogenic aggressive tumors described in Chapter 100. Upper jaw involvement is more likely to have its origin in the nasal cavity and maxillary sinus (Chapter 87) than within the alveolus. and the patterns of disease will reflect that origin.
Pathologically Altered Function
The pain involved in jaw lesions will to some extent affect chewing and swallowing, especially when infection has spread to the masticator space to cause trismus. Severe spreading infections may threaten the airway.
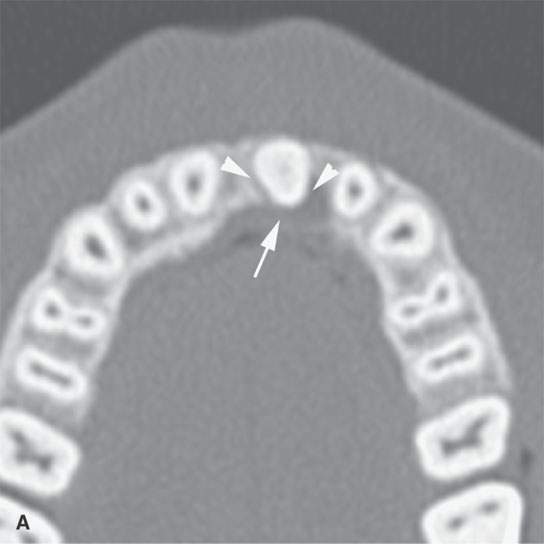
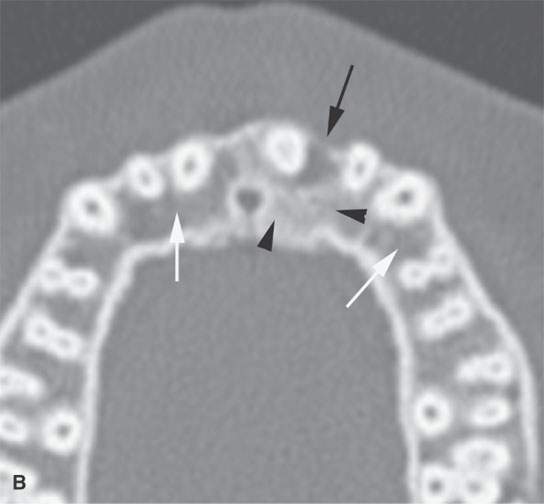

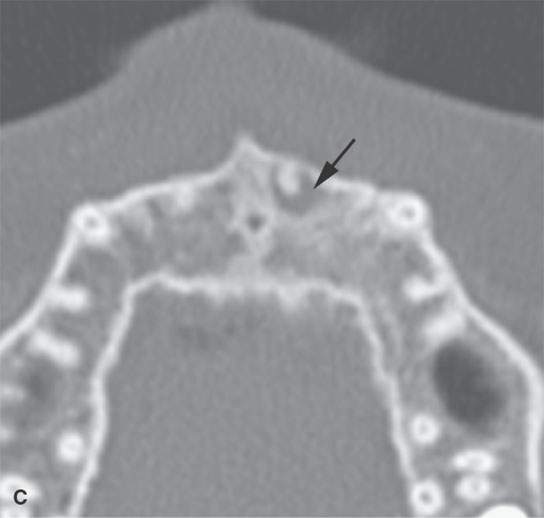
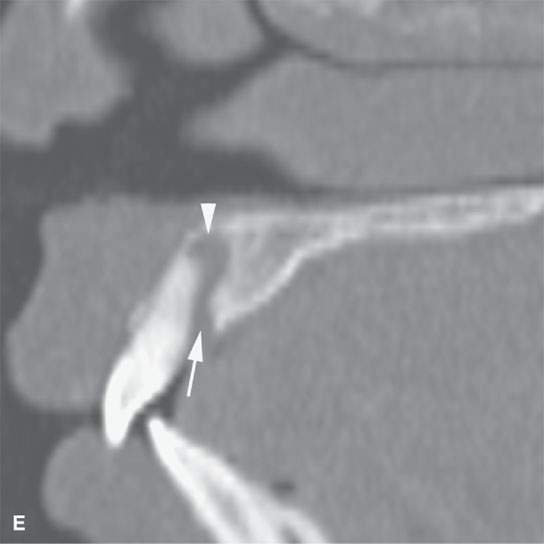
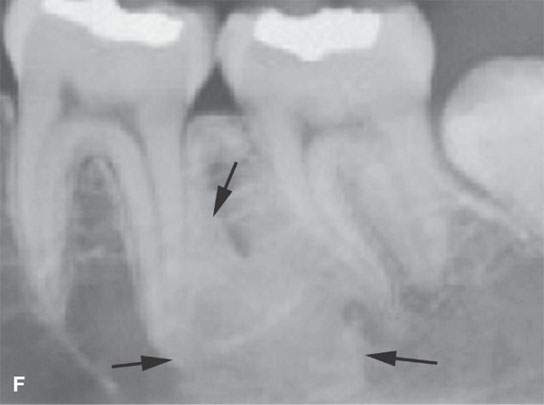
FIGURE 97.2. A patient to demonstrate spread patterns of advanced periodontal disease. Computed tomography was done because of facial pain in the region of the upper lip. A: Periodontal disease laterally (arrowheads) eroding the bone over the buccal surface of the maxilla. B: The periodontal disease has expanded laterally (black arrow) between the central and lateral incisor. There is an adjacent reactive sclerosis of bone (arrowheads). That sclerosis should be compared to the normal space of the maxilla (white arrows). C: Periodontal disease (arrowhead) spreading toward the tooth root (arrow). D: Coronal reformations of those axial images showing the periodontal disease spreading posteriorly to surround the root apex region (arrows). E: Sagittal reformations showing the periodontal and periapical disease from the lingual surface (arrow) to the bone of the premaxilla superiorly (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree