CHAPTER 52 Acute Coronary Syndrome
Acute coronary syndrome (ACS) is usually diagnosed in the emergency department based on history, physical examination, abnormalities on ECG, and elevations of cardiac serum biomarkers. According to the American Heart Association (AHA) and American College of Cardiology (ACC), high-risk patients recognized as having ACS should undergo early invasive coronary angiography and angiographically directed revascularization.1 The ultimate goal is to reperfuse and salvage any viable myocardium immediately. Other imaging modalities play minimal role in the evaluation of these patients. ACS is just one of many possible diagnoses when patients present to the emergency department with acute chest pain, however. Other considerations range from acute life-threatening conditions, such as pulmonary embolism, tension pneumothorax, or aortic dissection, to conditions with less morbidity and mortality, such as gastroesophageal reflux or costochondritis.
Acute chest pain accounts for approximately 6 million emergency department visits annually, and is the second most common reason for patients to present to the emergency department in the United States.2 Although most emergency department physicians and cardiologists have a low threshold for diagnosing ACS, 2% to 5% of patients are misdiagnosed and discharged inappropriately.3 In these patients, the mortality rate is 1.7 to 1.9 times greater than in patients who are hospitalized. Most patients who are inappropriately discharged with ACS have a nondiagnostic initial assessment. Various noninvasive imaging modalities are available to evaluate patients with acute, but indeterminate, chest pain in the emergency department.
PREVALENCE AND EPIDEMIOLOGY
In the most recent National Hospital Discharge Survey by the National Center for Health Statistics, there were approximately 1.4 million unique hospitalizations because of ACS in the United States in 2005.4 ACS is a major cause of morbidity and mortality in Western countries. The prevalence of ACS increases with age and predominates in men among patients younger than 70 years. In patients older than 70 years, the incidence occurs with equal frequency in men and women. Other risk factors that predispose patients to ACS include diabetes mellitus, smoking, hypertension, hypercholesterolemia, hyperlipidemia, a prior cerebrovascular event, inherited metabolic or connective tissue disorder, cocaine or amphetamine use, and occupational stress.
MANIFESTATIONS OF DISEASE
Imaging Technique and Findings
Radiography
Conventional chest radiography is the imaging modality used initially for screening noncardiac etiologies of acute chest pain, including pneumonia, pneumothorax, or rib fractures. Chest pain of cardiac origin also can be indirectly evaluated using chest radiography. Coronary arterial stenosis may be hinted by coronary artery calcification, which is seen in the “coronary triangle”—the mid-upper portion of the left cardiac silhouette on the frontal chest radiograph. In addition, circumferential calcifications may be seen within the expected location of myocardial wall, suggesting prior MI (Fig. 52-1). On the lateral chest radiograph, “tram-track” hyperdensities along the aortic arch correspond to atherosclerotic calcifications in the aorta, which can be independently correlated with coronary heart disease.5
Atherosclerotic calcifications overlying the borders of the heart may also indicate previous episodes of MI.6,7 Specifically, hyperdensity or calcifications of the left heart border, often curvilinear, may signify prior infarction of the left ventricular anterolateral wall. Focal outpouching of the left heart border may also represent postinfarct myocardial pseudoaneurysm or aneurysm.8
Ultrasonography
In risk stratifying and evaluating patients who present to the emergency department with acute chest pain, stress echocardiography is a versatile imaging modality. The prognostic information obtained is equivalent to radionuclide perfusion imaging and may be used to exclude ACS.9,10 Stress echocardiography provides functional and anatomic information by evaluating baseline ventricular function (e.g., ejection fraction, wall motion), valvular function, aortic root morphology, and pericardial anatomy. If a study shows reduction in ejection fraction or wall motion abnormality, especially as an interval change from previous assessment, the findings suggest myocardial ischemia.
Computed Tomography
In recent years, CT has become a noninvasive alternative to invasive coronary angiography in addition to its long-standing role in more general evaluation of the thorax. As the number of detectors has increased from 4 to 320, and gantry rotation speeds have increased, the spatial and temporal resolution for cardiac imaging acquisition has dramatically improved. The current generation of multidetector CT scanners provides accurate anatomic assessment of the coronary vasculature, allowing visualization to at least the third generation of coronary vessels. Compared with invasive coronary angiography, multiple studies have found multidetector CT to have sensitivity of 83% to 99%, specificity of 86% to 98%, positive predictive value of 66% to 93%, and negative predictive value of 97% to 99% in the evaluation of significant coronary arterial stenosis.11
Cardiac multidetector CT approaches the capability of invasive coronary angiography, the gold standard, in its ability to evaluate coronary arterial stenosis. Multidetector CT has several additional capabilities that can be valuable to emergency department physicians and cardiologists (Figs. 52-2 to 52-5). Cardiac multidetector CT can be used to assess the quantity and composition of atherosclerotic plaques and, potentially, to differentiate stable from unstable plaques.12,13 Cardiac multidetector CT also can evaluate myocardial function by assessing left ventricular wall motion and ejection fraction on the basis of images obtained throughout the different phases of the cardiac cycle.14 Dynamic imaging can be performed to assess perfusion of the myocardium.

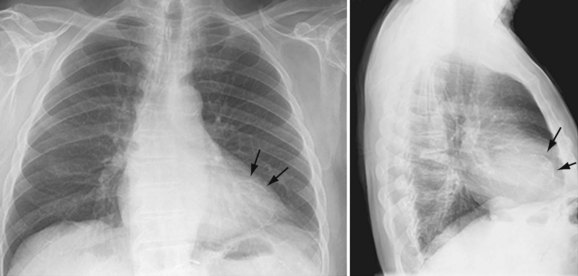
 FIGURE 52-1
FIGURE 52-1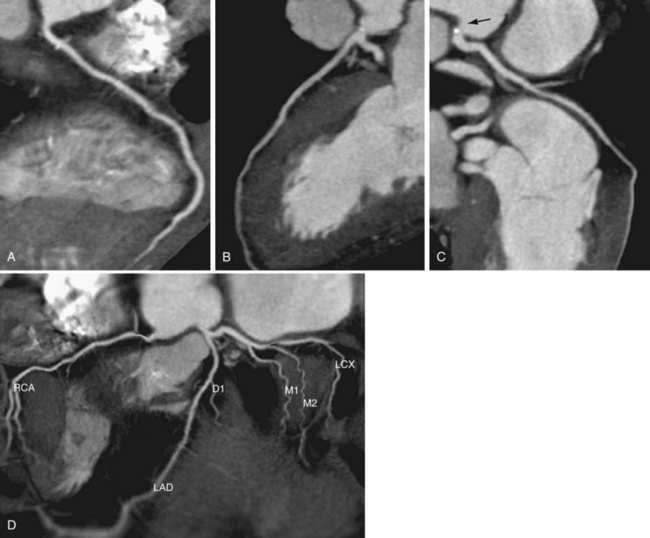
 FIGURE 52-2
FIGURE 52-2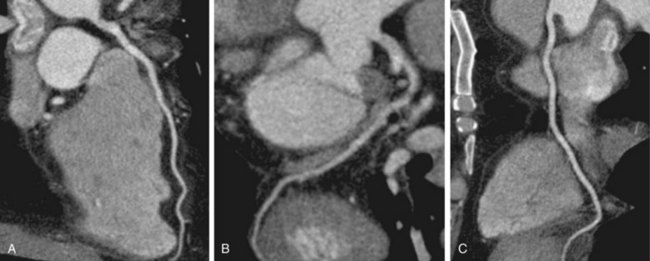
 FIGURE 52-3
FIGURE 52-3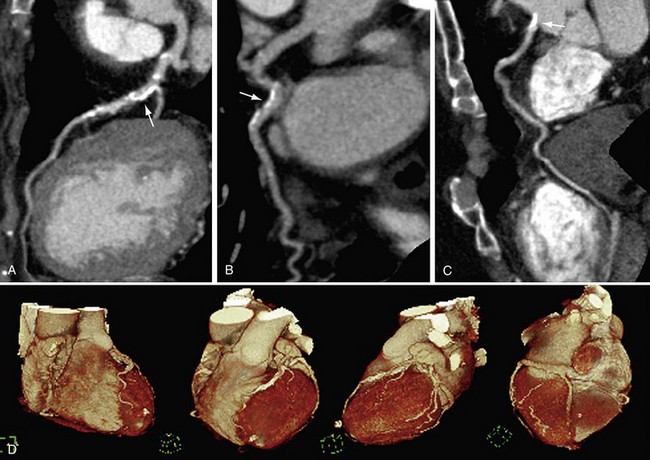
 FIGURE 52-4
FIGURE 52-4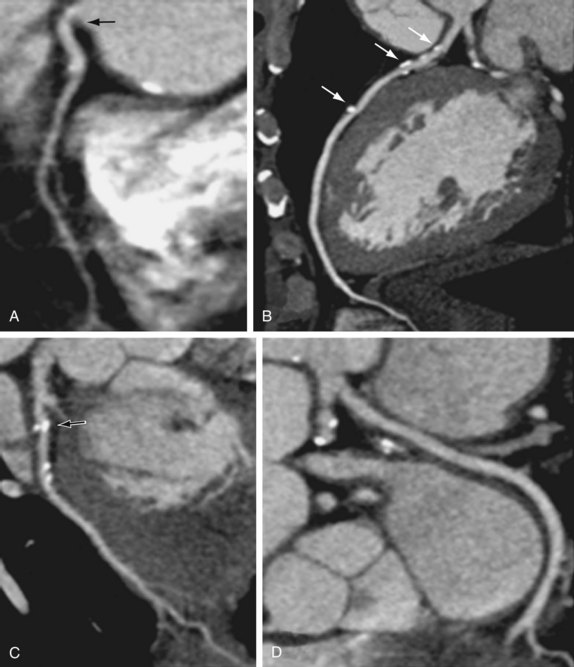
 FIGURE 52-5
FIGURE 52-5

