Acute interstitial pneumonia (AIP) is a severe acute disease of unknown etiology that usually occurs in a previously healthy individual and produces histologic findings of diffuse alveolar damage. The clinical, radiologic, and pathologic manifestations are identical to those of acute respiratory distress syndrome (ARDS); the only distinction is that no etiology is found. AIP is essentially idiopathic ARDS.
Prevalence and Epidemiology
AIP is rare, has no sex predominance, and has no association with cigarette smoking. The average age at presentation is 50 to 60 years (range, 7–83 years).
Clinical Presentation
A prodromal illness associated with symptoms suggestive of a viral upper respiratory tract infection is commonly present, with fever, chills, myalgias, and arthralgias. This is followed by dry cough and rapidly progressive and severe dyspnea. Approximately two-thirds of patients have symptoms for less than 1 week, and one-third have symptoms for 60 days before diagnosis.
Pathophysiology
Pathology
The histologic findings are those of diffuse alveolar damage ( Fig. 30.1 ). The acute, exudative phase shows edema, hyaline membranes, acute interstitial inflammation, and intraalveolar hemorrhage. The organizing (proliferative) phase shows loose organizing fibrosis and type II pneumocyte hyperplasia. Patients who survive more than 2 weeks may progress to the chronic phase with fibrosis that may be associated with extensive architectural remodeling resulting in honeycomb formation in severely fibrotic lung or, occasionally, development of cystic changes. There are no histologic features that distinguish diffuse alveolar damage in the setting of AIP from diffuse alveolar damage of known causes.

Lung Function
The main functional abnormalities are restrictive ventilatory defect (decrease in total lung capacity and vital capacity) and impaired gas exchange leading to progressive hypoxemic respiratory failure.
Manifestations of the Disease
Radiography
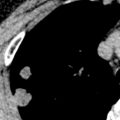
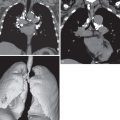
The radiographic manifestations are similar to those of ARDS and consist of bilateral airspace consolidation with air bronchograms ( Figs. 30.2 and 30.3 ). The consolidation is often initially patchy but tends to become rapidly confluent and diffuse, although it may have upper or lower lung zone predominance. The lung volumes are usually decreased.


Computed Tomography
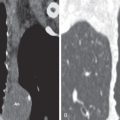
The earliest manifestations of AIP on high-resolution CT consist mainly of patchy or diffuse bilateral ground-glass opacities ( Figs. 30.4 and 30.5 ). Most patients have smooth septal thickening and intralobular lines superimposed on the ground-glass opacity resulting in a “crazy paving” pattern (see Figs. 30.4 and 30.5 ). Focal sparing of lung lobules frequently results in a geographic appearance ( Fig. 30.6 ; see Figs. 30.4 and 30.5 ). Consolidation is present in most patients (see Figs. 30.3 and 30.6 ). It may be patchy or confluent and tends to involve mainly the dependent lung. In 10% to 20% of cases the consolidation has a peripheral distribution.