Etiology
Adenomyosis is defined pathologically when endometrial glands and stroma are found in the myometrium, distant from the endometrial cavity itself. This ectopic endometrial tissue has the ability to induce hypertrophy of the surrounding myometrium. This process can be focal or diffuse and thus accounts for the variability in the ultrasound appearances noted. The endometrium-myometrium junctional zone is jagged and fuzzy because the endometrial mucosa essentially invades the underlying myometrium, thus blurring the interface between these two, typically distinct zones. (This may be focal or global.)
Ultrasound Findings
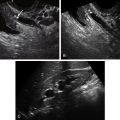
Generalized Adenomyosis
The uterus is typically enlarged and globular with heterogeneous myometrium, which is typically wider on one side than the other. The heterogeneous myometrium often contains myometrial cysts, which likely represent areas of glandular dilatation or hemorrhage caused by repeated bleeding. These cysts are also frequently seen in a subendometrial location.
Adenomyoma
An adenomyoma appears as a focal, somewhat circumscribed island of heterogeneity in the myometrium, suggesting a fibroid, but typically without clear borders. When the borders are sharp, one cannot distinguish an adenomyoma from a fibroid. The adenomyoma may project into the cavity in the form of a broad-based polyp (polypoid adenomyoma).
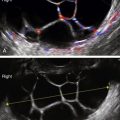
Three-dimensional (3-D) ultrasound is helpful to demonstrate the multitude of linear hyperechoic bands emanating from the endometrium into the myometrium, producing the shaggy outline of the endometrial cavity on 3-D coronal view of the uterus.
Although magnetic resonance imaging (MRI) has been useful for diagnosing adenomyosis, it is unnecessary because ultrasound has similar accuracy. A comparison between ultrasound and MRI was reported using 23 articles (involving 2312 women). Transvaginal ultrasound had a sensitivity and specificity of 72% and 81%, respectively, whereas MRI had a sensitivity and specificity of 77% and 89%, respectively.
Doppler evaluation of adenomyosis usually does not add to the diagnosis because the amount of vascularity is variable and nonspecific.
Differential Diagnosis
If the area of adenomyosis is focal, it may be confused with a fibroid or a polyp if it projects into the endometrial cavity. Because of the lucencies and heterogeneities in the myometrium, uterine malignancy (though very rare) is sometimes considered. The clue to the correct diagnosis is the asymmetry of the width of the myometrium comparing the posterior to the anterior aspect on longitudinal view as well as the shaggy appearance of the endometrial echo in a patient with chronic pain and abnormal bleeding.
Clinical Aspects and Recommendations
Historically, heavy menstrual bleeding (menorrhagia) and painful menstruation (dysmenorrhea) are the major symptoms of adenomyosis and are said to occur in approximately 60% and 25% of women, respectively. It has also been implicated in some cases of chronic pelvic pain. In the past, symptoms typically developed in women in the fourth and fifth decade of life (perimenopausally); however, this probably reflects the fact that in the past the diagnosis of adenomyosis historically was made at the time of hysterectomy and not with sophisticated imaging techniques as are currently available. In fact the obvious presence of endometrial glands and stroma contained within the myometrium in a large number of asymptomatic women should cause clinicians to rethink whether adenomyosis is truly a “disease” or whether in some cases it may be co-existing and not causal of the patient’s symptoms. The exact percentage of patients who will have classic findings of adenomyosis on sophisticated ultrasound studies and yet be totally asymptomatic is unknown.
When present, the menorrhagia is probably related to the increased endometrial surface area of the enlarged uterus. Dysmenorrhea may be caused by the cyclic bleeding and swelling of the endometrial tissue confined within the myometrium.
Definitive treatment for adenomyosis is hysterectomy. Because disease is confined to the uterus, ovarian conservation can be considered unless there are other reasons for their removal. As there is no true plane separating the adenomyotic tissue from normal myometrium, surgical excision as in myomectomy is not appropriate. Various medical (nonsurgical) approaches have been employed, including oral contraceptive pills for treatment of the dysmenorrhea and menorrhagia, progestin only therapy, and more recently levonorgestrel-releasing intrauterine devices (IUDs).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree