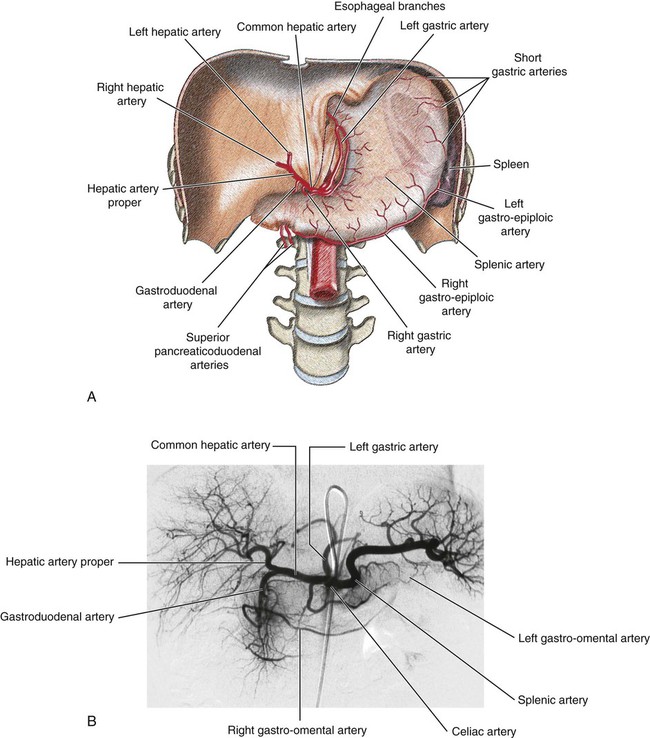
Nadia J. Khati, Morvarid Alaghmand, Michael J. Manzano and Anthony C. Venbrux The celiac axis arises from the ventral surface of the aorta at the level of the T12-L1 disc space. It immediately divides into three branches—the left gastric artery, splenic artery, and common hepatic artery—and supplies the liver, spleen, stomach, and pancreas (Fig. 52-1). Both the splenic and left gastric artery can arise directly from the aorta as separate branches, but in over 95% of patients, the common hepatic artery arises from the celiac trunk. • Pancreatic branches. As the hepatic artery passes along, it gives off small branches to supply the neck, body, and tail of the pancreas. • Short gastric arteries, which supply blood to the fundus of the stomach • Left gastroepiploic artery (terminal branch of the splenic artery), which runs along the greater curvature of the stomach and anastomoses with the right gastroepiploic artery • The hepatic proper, which ascends toward the liver and is located on the left side of the bile duct and anterior to the portal vein. It gives off two branches: the right and left hepatic arteries. • Gastroduodenal artery, which descends posterior to the superior part of the duodenum. At the lower part of the superior duodenum, the gastroduodenal artery divides into the right gastroepiploic (which supplies both surfaces of the stomach and the greater curvature) and the superior pancreaticoduodenal arteries. The second branch divides into anterior and posterior branches and supplies the head of the pancreas and the duodenum. Other branches of the common hepatic artery include the supraduodenal and right gastric arteries. Anastomoses in the stomach include:
Alimentary Tract Vasculature
Arterial Supply
Celiac Trunk
Alimentary Tract Vasculature