Fig. 24.1
Laparoscopic ultrasound probe. Notice that the angle of the probe can be adjusted to allow for easier positioning during laparoscopy. The ultrasound sensor is highlighted in the inset [1]
Oncology
Ultrasound can have tremendous utility during pediatric oncological surgery. Lesions within the liver parenchyma and their relationship to the hepatic vasculature can be identified. This will dictate many of the important decisions one must make for hepatic tumors, specifically whether or not the tumor is resectable, and if so, which vessels will need to be taken to get an adequate resection. The pretreatment extent of disease (PRETEXT) is the staging system currently used to guide therapy for hepatoblastoma (Fig. 24.3). Defining the PRETEXT stage is based on knowing the liver sectors which are defined by the portal and hepatic vein branches. The PRETEXT stage also contains modifiers which identify how close the tumor is to the hepatic veins, inferior vena cava (IVC), or portal vein branches [7, 8]. Understanding these relationships is critical to planning your resection. In the operating room, identifying this relationship will define which vessels need to be taken to get an adequate resection. Once you understand which vessels need to be taken for the tumor resection, you will know whether a standard left or right hepatic lobectomy will be sufficient, or if a trisegmentectomy or central hepatectomy are required. It is also important to note that intraoperative ultrasound may provide more up to date information than preoperative imaging. It may also more clearly identify some of the anatomic relationships of the tumor, which may actually lead to performing a different operation than was planned pre-operatively (Figs. 24.4 and 24.5) [9].
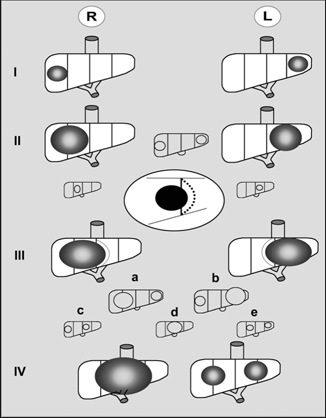
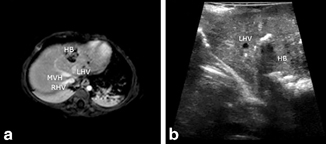
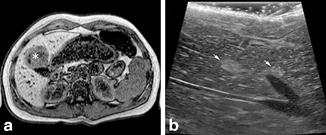
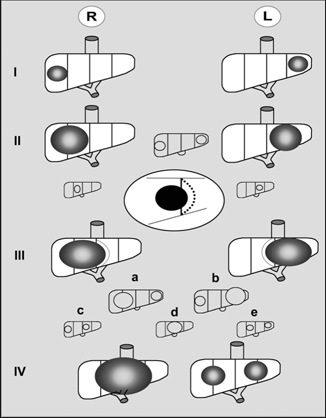
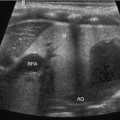
Fig. 24.3
PRETEXT stages. The liver is divided into four sectors defined by the hepatic veins. PRETEXT stage is defined by the number of uninvolved sectors. (1) PRETEXT 1 tumors have three contiguous uninvolved sectors. (2) PRETEXT 2 tumors have two contiguous uninvolved sectors. (3) PRETEXT 3 tumors have one contiguous uninvolved sector. (4) PRETEXT 4 tumors have no uninvolved sectors [7]
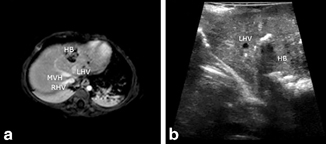
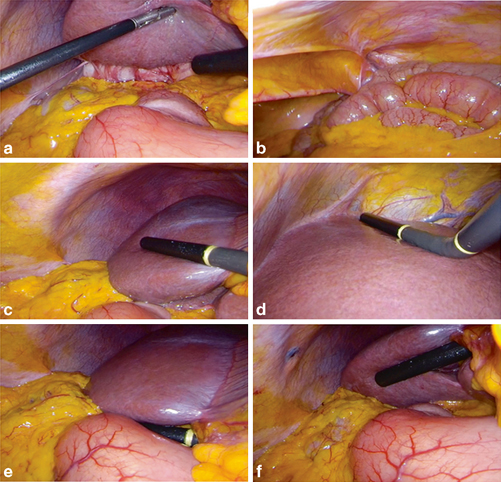
Fig. 24.4
Findings on intraoperative ultrasound. a Preoperative MRI showed extension of hepatoblastoma into segment IVa. b Intraoperative ultrasound showed tumor extending near but not beyond the left hepatic vein, meaning there was no segment IVa involvement. This allowed an adequate resection with a left lateral segmentectomy as opposed to the original plan for a left hemihepatectomy [9]
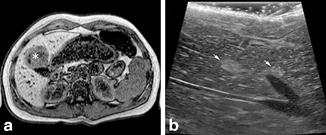
Fig. 24.5
Findings on intraoperative ultrasound. a Single adenoma (asterisk) identified on preoperative MRI. b Intraoperative ultrasound identified multiple additional adenomas (arrows). This patient was diagnosed with diffuse adenomatosis and will require biannual ultrasound surveillance [9]
For Wilms’ tumor , the role of ultrasound to identify tumor thrombus in the renal vein and IVC has already been well established [10]. Intravascular extension of tumor thrombus occurs in 4–11 % of children with Wilms’ tumor [11, 12]. Intraoperative ultrasound can be used to confirm the extent of tumor thrombus in the operating room, or alternatively to confirm the lack of tumor thrombus before ligating and transecting the renal vein. This point is important, because accidental encounter of renal vein tumor thrombus during vessel ligation and transection will upstage the patient to a local stage III tumor, which necessitates flank radiation and the addition of doxorubicin and its inherent risk for cardiac toxicity. Conversely, the presence of intravascular extension does not affect the prognosis if it is successfully resected [13]. Identifying tumor thrombus while ligating the renal vein has been previously reported, and can be avoided with the intraoperative use of ultrasound [14].
In bilateral Wilms, partial nephrectomy is the treatment option [15, 16]. Sparing some of each kidney often allows retention of adequate renal function to avoid dialysis. Obtaining appropriate margins is important and these margins are not always obvious from visual inspection. Intraoperative ultrasound can guide resection margins for the partial nephrectomy and is becoming the standard of care today (Fig. 24.6).


Fig. 24.6
Intraoperative renal ultrasound showing Wilms’ tumor for margin planning
Foreign Body
Fluoroscopy has proven to be an invaluable adjunct in the localization of radiopaque foreign bodies and is utilized extremely often for this purpose. In the case of foreign bodies that cannot be seen on X-ray, surgeons are often forced to rely on palpation to locate the object. The lack of imaging guidance can make these cases extremely challenging and certainly decrease the success rate of foreign body removal. Ultrasound is an excellent tool in this situation, as the foreign body will typically have a different echogenicity than the soft-tissue and will therefore be easily visible on ultrasound (Fig. 24.7a and b). If planning to use ultrasound intraoperatively to locate a foreign body, it is best to have a preoperative ultrasound to confirm that the foreign body can be visualized. Once that is confirmed, the ultrasound will be very valuable in the operating room. Wooden splinters are notoriously difficult to find, and cannot be identified with fluoroscopy. Ultrasound is typically able to identify wooden splinters and has been used to aid in their removal [17–19].
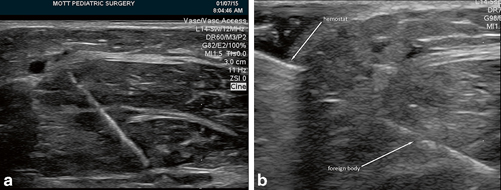
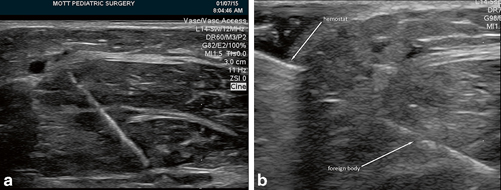
Fig. 24.7
Foreign body in soft tissue. a Foreign body seen in intraoperative ultrasound. b Ultrasound guidance of instrument (hemostat) to foreign body
Supprelin implants are subdermal implants utilized for long-term delivery of the gonadotropin-releasing hormone analog histrelin in patients with central precocious puberty. These implants allow hormone delivery without the need for frequent intramuscular injections and are the preferred method for patients and families. The implants need to be removed and replaced at regular intervals. Removal can be challenging as the implants are soft and colorless, and implant fracture is not an uncommon event. Ultrasound can be used in this situation to find the fractured implant and assist in its removal [20].
Extracorporeal Membrane Oxygenation (ECMO) Cannula Placement
Percutaneous placement of ECMO cannulas has become more common, in part due to the excellent visualization afforded by echocardiogram. Proper positioning of the cannula is critical to maintain good flows on the ECMO circuit. Cardiac ultrasound is used to identify the position of the cannula and guide its placement. Ultrasound guidance can be used for placement of a single double-lumen cannula for veno-venous ECMO such as the Avalon cannula (Fig. 24.8a) as well as for placement of a single lumen venous cannula that will be used for either veno-venous or arterio-venous ECMO (Fig. 24.8b




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree