28
Anatomy of the Gastrointestinal Tract, Liver, and Biliary System
Familiarity with the normal and variant anatomy of the gastrointestinal (GI) tract, liver, and biliary system is essential for the interventional radiologist. Pathologic conditions may distort normal anatomy and make therapeutic interventions difficult or impossible. An understanding of variant vascular and ductal anatomy, as well as of the presence and location of collateral pathways is essential to both diagnosis and therapy.
 Arterial Anatomy
Arterial Anatomy
The arterial supply to the GI tract is by the three main ventral branches of the abdominal aorta (Fig. 28-1): the celiac artery, the superior mesenteric artery (SMA), and the inferior mesenteric artery (IMA). There is considerable variation in the branching pattern from these three main vessels. Furthermore, there are copious collateral pathways between the vascular territories.
Celiac artery
The celiac artery arises from the aorta at the level of the T12 vertebral body.1 Its branches supply the liver, gallbladder, stomach, proximal duodenum, pancreas, and spleen. The three major branches of the celiac artery are the left gastric artery (LGA), splenic artery, and common hepatic artery (Figs. 28-2 through 28-4).
Left gastric artery
The LGA is a branch of the celiac artery in 90% of all persons. It arises from the superior margin of the proximal celiac artery and courses vertically toward the lesser curvature of the stomach. The origin and orientation of the LGA sometimes make selective catheterization of the LGA difficult. Accessory LGA branches may arise from the left hepatic artery. The LGA arises directly from the aorta in 1 to 5% of all persons2–4 and supplies the lower esophagus, cardia, fundus, and body of the stomach.
Splenic artery
The splenic artery is the largest branch of the celiac artery and is tortuous in adults. It courses superior and anterior to the splenic vein and may arise directly from the aorta in 2% of persons.3 The splenic artery supplies the spleen, the pancreas, and the stomach.
Branches of the splenic artery include the posterior gastric artery, short gastric arteries, left gastroepiploic artery, and the superior and inferior terminal branches supplying the spleen. The splenic artery gives rise to three pancreatic branches: the dorsal pancreatic artery supplies the neck and body of the pancreas; the great pancreatic artery (arteria pancreatica magna) supplies the body of the pancreas; and the caudal pancreatic artery supplies the tail of the pancreas. The transverse pancreatic artery runs within the pancreas and originates from the left branch of the dorsal pancreatic artery. The transverse pancreatic artery anastomoses with the other pancreatic branches from the splenic artery.5
Common hepatic artery
The main branch of the common hepatic artery is the gastroduodenal artery (GDA). The superior pancreaticoduodenal artery arises from the GDA, which continues as the right gastroepiploic artery along the greater curvature of the stomach. The right gastroepiploic artery then forms an anastomosis with the left gastroepiploic artery. The left gastroepiploic artery arises from the distal splenic artery.
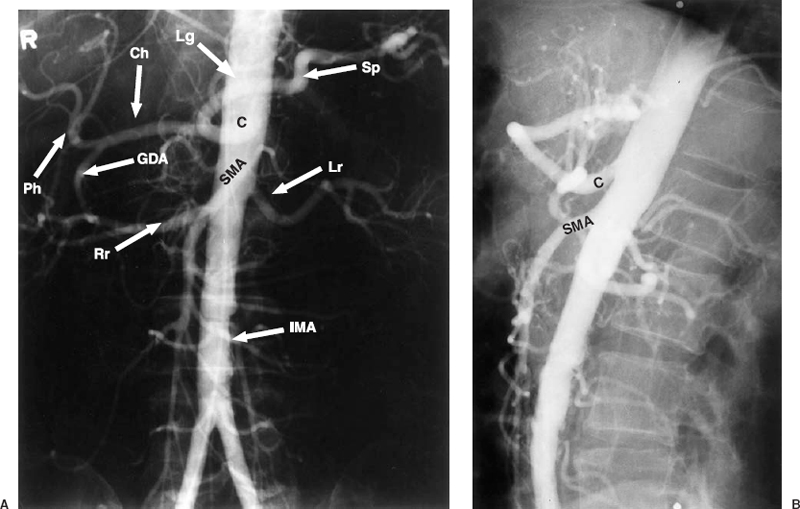
FIGURE 28-1. Abdominal aortogram. Frontal (A) and lateral (B) projections. C, celiac artery; SMA, superior mesenteric artery; IMA, inferior mesenteric artery; Sp, splenic artery; Ch, common hepatic artery; GDA, gastroduodenal artery; Ph, proper hepatic artery; Rr, right renal artery; Lr, left renal artery; Lg, left gastric artery.
The common hepatic artery courses to the right and becomes the proper hepatic artery after giving rise to the GDA. The right and left hepatic arteries arise from the proper hepatic artery,and the middle hepatic artery arises from either the left orright hepaticartery and supplies the medial segment of the left lobe of the liver.6
Cystic artery
The cystic artery is usually a branch of the right hepatic artery, but it may arise from the left or common hepatic artery (Fig. 28-5).3 This artery is inconsistently visualized on arteriography.
Right gastric artery
This small vessel arises from the proper hepatic or left hepatic artery in 80% of persons. In the remaining 20%, the right gastric artery arises from the GDA or from the right or middle hepatic artery.3 The right gastric artery forms an anastomosis with the left gastric artery along the
lesser curvature of the stomach. This vessel usually is not visualized on arteriography.
Hepatic Arterial Variants
There is considerable anatomic variation in the arterial supply to the liver.3,6 The most common variations include the following:
- 1. The left hepatic artery arises from the LGA (10–30%) and also may be referred to as the aberrant left hepatic branch.
- 2. The accessory left hepatic artery arises from the LGA (8%).
- 3. The replaced right hepatic artery arises from the SMA (14–20%) and also may be referred to as the aberrant right hepatic branch. It runs behind the pancreas and the portal vein.
- 4. The accessory right hepatic artery (partial replacement) arises from the SMA (6%).
- 5. The replaced common hepatic artery (Fig. 28-6), arises from the SMA with no hepatic artery branches originating from the celiac artery (2.5%).7
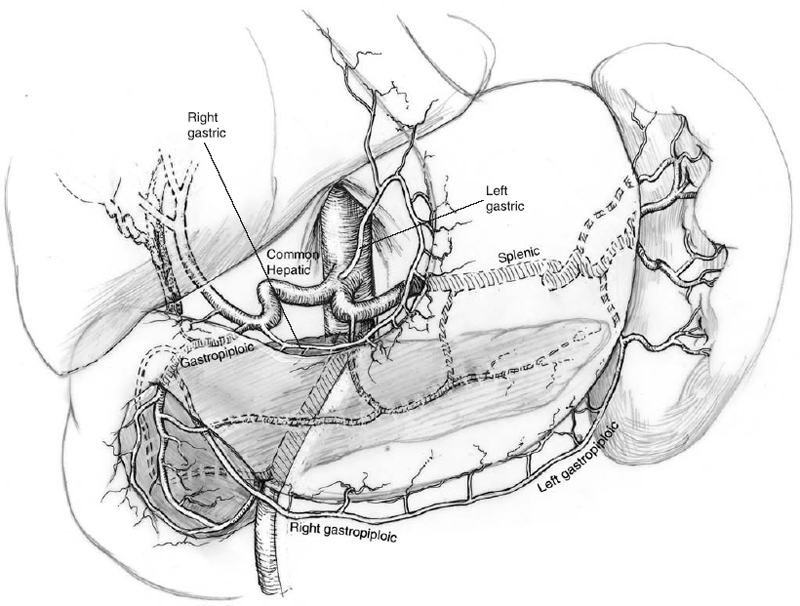
FIGURE 28-2. Branches of the celiac artery.
The presence of a replaced hepatic artery branch is an important variant that may affect arterial anastomoses during liver transplant surgery, dissection during liver resection, portocaval shunt surgery, or pancreaticoduodenectomy (Whipple procedure). Variant anatomy, such as an LGA branch arising from the left hepatic artery or a replaced hepatic artery branch, must be recognized in cases of percutaneous transarterial tumor chemoembolization. Failure to recognize these variants may result in inadequate embolization or unintentional embolization of the vessels supplying the bowel. During papaverine infusion into the SMA in a patient with a replaced hepatic artery branch, the catheter tip must be positioned distal to the replaced hepatic artery branch for an effective infusion.
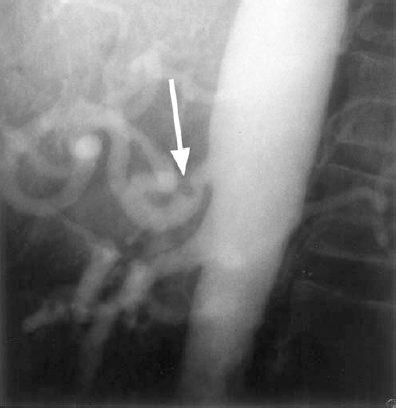
FIGURE 28-3. Celiac axis compression. Lateral abdominal aortogram shows a smooth narrowing of the superior aspect of the celiac artery that resulted from crural fibers of the diaphragm (median arcuate ligament).16 This finding is common and should not be considered a pathologic condition in asymptomatic persons. It remains unresolved whether compression of the celiac axis by the median arcuate ligament, as an isolated finding, can result in clinically significant mesenteric ischemia.17
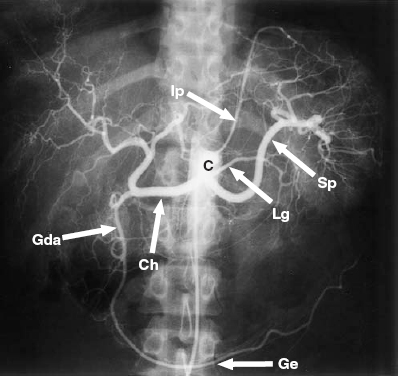
FIGURE 28-4. Celiac arteriogram. C, celiac trunk; Sp, splenic artery; Lg, left gastric artery; Ch, common hepatic. Gda, gastroduodenal artery; Ge, gastroepiploic artery; Ip, inferior phrenic artery.
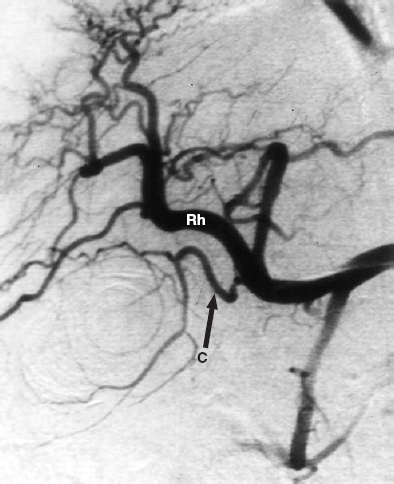
FIGURE 28-5. The cystic artery, © typically arises from the right hepatic (RH) artery.
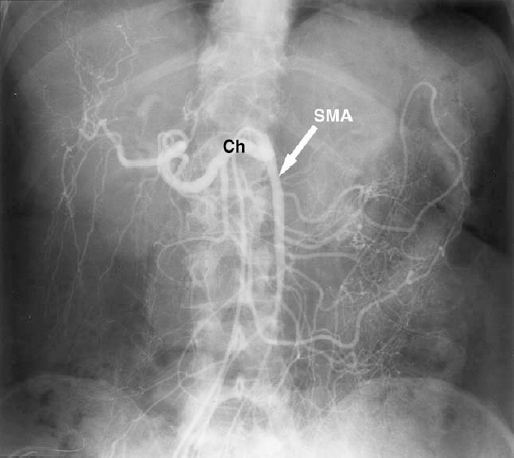
FIGURE 28-6. Replaced common hepatic artery. Superior mesenteric artery (SMA) injection shows the common hepatic artery origin from the proximal SMA. Ch, common hepatic artery.
Inferior phrenic artery
The inferior phrenic artery can arise from the celiac artery in 35% to 65% of persons or directly from the aorta. The right and left inferior phrenic arteries may have a common or separate origins. Before entering the diaphragm, the left inferior phrenic artery may give off a small gastroesophageal branch. The inferior phrenic arteries may not be well opacified on celiac arteriography, because they arise from the most proximal aspect of this vessel.8,9
Superior mesenteric artery
The SMA arises from the aorta approximately 1 to 2 cm inferior to the origin of the celiac artery at the level of L1 vertebral body1 (Figs. 28-7 and 28-8). The celiac artery and the SMA from the aorta (celiacomesenteric trunk) have a common origin in 0.4% of persons (Fig. 28-9).3 Branches of the SMA include the inferior pancreaticoduodenal artery, the jejunal and ileal arteries, the middle colic artery, right colic artery, and ileocolic artery. Branches of the SMA supply the head of the pancreas, duodenum, jejunum, ileum, cecum, ascending colon, and proximal half of the transverse colon.
Inferior pancreaticoduodenal artery (IPDA)
The first branch of the SMA, the IPDA occasionally may have a common origin with a jejunal artery. It divides into anterior and posterior branches, which anastomose with the corresponding branches of the superior pancreaticoduodenal arteries from the GDA to form the pancreaticoduodenal arcades. The IPDA may arise as a single artery or as one anterior branch and one posterior branch with separate origins.3,6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree