Imaging Presentation
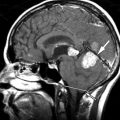
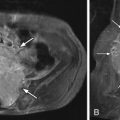
Magnetic resonance (MR) imaging reveals a solid and cystic mass containing heterogeneous regions of high, low, and intermediate signal intensity ( Fig. 7-1 ) . The mass predominantly involves the posterior vertebral arch of T3 on the left, with some involvement of the T3 vertebral body on the left. Computed tomography (CT) shows a large soft tissue mass that has destroyed the T3 spinous process, left lamina, and left pedicle, and extends into the vertebral body ( Fig. 7-2 ) .


Discussion
The lesion that has become known as “aneurysmal bone cyst” was originally described by Van Arsdale in 1893, who referred to this lesion as a “ossifying hamartoma.” The term aneurysmal bone cyst was first used for describing these lesions in 1942 by Jaffe and Lichtenstein. Aneurysmal bone cysts are rare, benign, yet locally destructive; they are expansile, highly vascular bone lesions. They represent approximately 1% to 2% of primary bone “tumors,” although they are not true neoplasms. The majority of aneurysmal bone cysts arise in the metaphysis of the long bones. Approximately 10% to 20% of aneurysmal bone cysts occur in the axial skeleton. Spinal aneurysmal bone cysts occur most frequently in the thoracic spine, followed by the lumbar spine, cervical spine, and least commonly in the sacrum. Aneurysmal bone cysts in the sacrum or pelvis tend to be more aggressive lesions that cause extensive bone destruction ( Figs. 7-2 to 7-8 ) . Spinal aneurysmal bone cysts nearly always arise in the posterior vertebral arch but frequently extend into the ipsilateral pedicle and vertebral body, epidural space, or adjacent neural foramen (see Figs. 7-1 and 7-2 ). They rarely extend into the nearby ribs or adjacent vertebrae.






The majority of patients who present with aneurysmal bone cyst are younger than age 20, and there is a slight female predilection; 95% of patients with spine lesions present with back pain, usually slow in onset. These patients may have scoliosis. Myelopathy or radiculopathy may be present if the spinal cord or nerve roots are compressed. Paresthesias, loss of anal sphincter tone, leg weakness, and urinary retention may occur with spinal or sacral aneurysmal bone cysts depending on their location and extent.
Secondary aneurysmal bone cysts may arise in or adjacent to other primary bone tumors in a small percentage of cases, especially in giant cell tumors and osteoblastomas, but they also occasionally occur in osteosarcomas, chondroblastomas, fibrous histiocytomas, and less commonly in other bone tumors. The etiology of aneurysmal bone cysts is unknown. It is possible that some of these tumors arise secondary to vascular anomalies such as arteriovenous (AV) fistula formation in bone secondary to trauma or neoplasm. Hereditary influences are believed to play a role in a significant number of primary aneurysmal bone cysts. Translocations or deletions in chromosomes 16 and 17 have been demonstrated in some patients.
Histologically, the typical aneurysmal bone cyst is composed of blood-filled cavities with surrounding trabecular and solid elements comprised of vascularized stromal tissues containing multinucleated osteoclastic giant cells, spindle cells, fibroblasts, myofibroblasts, hemosiderin deposits, and a variable amount of cartilage and osteoid that may be mineralized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree