Imaging Presentation
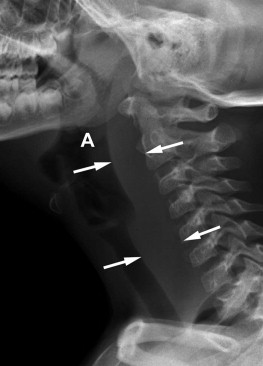
Lateral radiograph of the neck shows abnormal widening of the soft tissues between the posterior airway and the ventral vertebral bodies. Given the patient’s clinical history, one should suspect a retropharyngeal inflammatory process and obtain more specific imaging if the patient is stable ( Fig. 60-1 ) .
Discussion
Retropharyngeal abscess (RPA) is a deep neck space infection that has the potential for very serious complications including airway compromise and sepsis. RPA used to be exclusively a disease of young children; however, it has been increasing in frequency in adults.
An RPA is a collection of pus within lymph nodes in the back of the throat. RPAs are believed to occur as a consequence of infections of the nasopharynx, paranasal sinuses, tonsils, adenoids, or middle ear. The infection then spreads to retropharyngeal lymph nodes that lie between the posterior pharyngeal wall and the prevertebral fascia. It is believed that these lymph nodes atrophy by the third or fourth year of life, which is why the typical nontraumatic RPA is seen in young children. The incidence of RPA decreases in children over 3 years of age. Although rare, the majority of adult cases arise from localized trauma, foreign body ingestion, complications from procedures such as intubation or endoscopy, or in immunocompromised patients. The incidence of RPAs has decreased since the advent of antibiotics. A new subset of patients at risk for RPAs is intravenous drug abusers who inject the vessels in their neck.
Whether in children or adults, RPAs can manifest with a sore throat, difficulty swallowing, nuchal pain, fever, and an elevated white blood cell count. Less common symptoms include stridor and respiratory difficulty. Because stridor and respiratory difficulty are rare, limited neck mobility is an important clinical clue in diagnosing RPA. Torticollis can result if the inflammatory process irritates the cervical muscles or nerves.
Imaging Features
The lateral radiograph was the single most important imaging tool to aid in the diagnosis of retropharyngeal abscess prior to the advent of advanced imaging. If one uses the lateral radiograph as a diagnostic tool, it is important to ensure that it is a true lateral radiograph with the neck in extension and with full inspiration so as to not falsely thicken the retropharyngeal soft tissues. Computed tomography (CT) and magnetic resonance imaging (MRI) are now the preferred imaging techniques. Although these advanced imaging modalities are used to confirm the diagnosis, they more importantly localize the infectious process and search for and define an abscess cavity. However, CT scanning has been shown to have significant false-negative (13%) and false-positive (10%) rates in predicting pus at surgery. The distinction between retropharyngeal abscess (RPA) and retropharyngeal cellulitis (RPC) or phlegmon is important. One study used this difference in its treatment decision. Patients with RPA underwent surgical intervention and antibiotics, whereas those with RPC were treated with antibiotics alone. There were no treatment failures in either arm of this study.
The lateral radiograph is often used as a screening examination and will demonstrate thickening of the prevertebral soft tissues ( Fig. 60-1 ) . CT will demonstrate a region of fluid density in the retropharyngeal space ( Fig. 60-2 ) . There is variable peripheral enhancement of the fluid collection. A mature retropharyngeal abscess is suggested by thick enhancement of the wall. MRI is more sensitive in differentiating the fluid signal intensity abscess (decreased T1, increased T2 signal and peripheral enhancement) from cellulitis. Depending on operator experience, ultrasound is more accurate than either CT or MRI in differentiating RPA from cellulitis.











