Clinical Presentation
The patient is a 57-year-old male with chronic low back pain, bilateral lower extremity pain, paresthesias, and difficulty walking. The pain is exacerbated by standing and walking even short distances. On physical examination, the patient has moderate weakness of the hip flexors bilaterally, increased tone in the lower extremities, bilateral hyperreflexia, and sustained clonus bilaterally. The patient has a cardiac defibrillator, so a computed tomography (CT) scan was ordered instead of a magnetic resonance (MR) scan.
Imaging Presentation
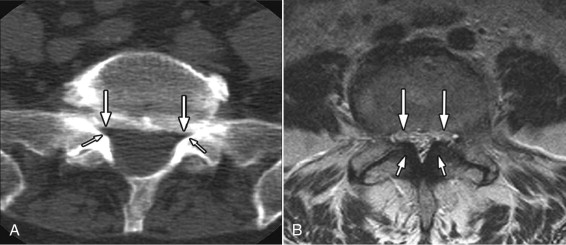
CT scan of the lumbar spine revealed severe central canal stenosis at the L4-5 level caused by generalized disc bulging, bilateral ligamentum flavum thickening, and facet hypertrophy. Bilateral lateral recess stenosis is present below the L4-5 intervertebral disc level (L4-5 subarticular zone) ( Figs. 41-1 and 41-2 ) .

Discussion
The lateral recess is sometimes referred to as the subarticular zone or subarticular groove because it is anatomically located below the intervertebral disc level. There is controversy in the literature as to what actually constitutes the lateral recess. There are those who consider the intervertebral neural foramen as part of the lateral recess. We consider the neural foramen (lateral intervertebral canal) and the lateral recess (subarticular zone) as distinct anatomic entities. Even with the advanced imaging techniques available today, the lateral recess remains a misunderstood anatomic concept, and unfortunately, stenosis of the lateral recess is still overlooked by some who evaluate CT and MR imaging studies.
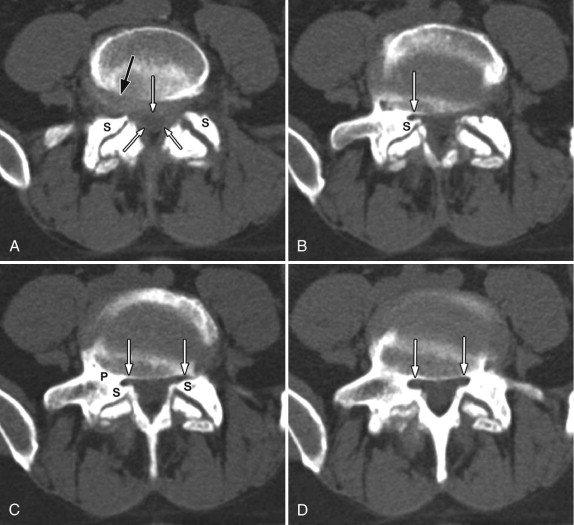
Anatomically, the lumbar lateral recess is formed anteriorly by the posterolateral surface of the vertebral body and overlying posterior longitudinal ligament, posteriorly by the superior articular facet and overlying ligamentum flavum, and laterally by the pedicle ( Figs. 41-3 to 41-5 ) . There are some who also consider the intervertebral disc margin as an anterior boundary of the lateral recess. However, the disc margin is not anatomically part of the lateral recess or subarticular zone . The nerve root that exits the thecal sac at a given disc level is positioned within the lateral recess. This nerve root, which has the same level name as the adjacent pedicle, will course below the pedicle before exiting the spinal canal within the intervertebral neural foramen below. For example, the L4 nerve root exits the thecal sac at the L3-4 disc level, enters the lateral recess, which is a three- sided structure bound by the L4 pedicle medially, the L4 vertebral body anteriorly, and superior articular process of L4 posteriorly. The L4 nerve root courses inferiorly beneath the L4 pedicle to exit the spinal canal via the L4-5 neural foramen.
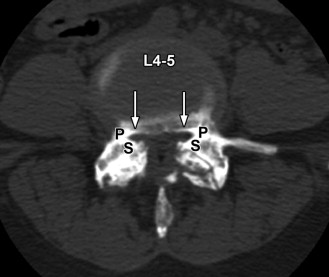
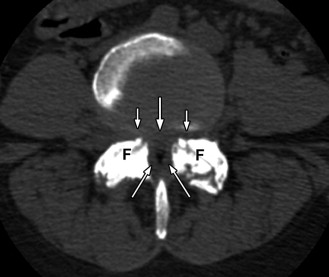
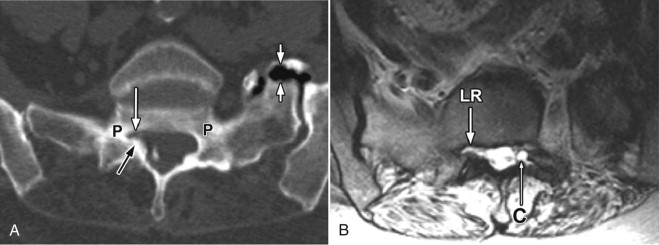
By far the most common level affected with lateral recess stenosis is L4-5 (see Figs. 41-1 and 41-3 ), which causes compression of the L5 nerve root. The second most common level of lateral recess stenosis is L5-S1, which affects the S1 nerve root ( Figs. 41-5 and 41-6 ). The lateral recess may be congenitally narrowed, for example, in patients with developmentally “short” pedicles or in patients with achondroplasia. Acquired lateral recess stenosis is far more common than and is often associated with central canal stenosis secondary to vertebral spondylitic bony ridges and facet osteoarthritis resulting in overgrowth (hypertrophy) of the facets (see Figs. 41-1 and 41-3 ). The lateral recess tends to be most narrowed just below the level of the intervertebral disc, at the level of the superior margin of the vertebral endplate and medial to the pedicle (see Figs. 41-1, 41-2, and 41-7 ). At this level, a nerve root that has exited the thecal sac becomes trapped between hypertrophic spondylitic ridges arising along the posterolateral vertebral endplate margin and the hypertrophic superior articular process (see Figs. 41-1 and 41-8 ). Central canal stenosis is often present in patients with bony lateral recess stenosis (see Figs. 41-4 and 41-9 ). In patients with central canal stenosis, hypertrophic spondylitis ridges, facet hypertrophy, and ligamentum flavum are the common components that cause circumferential thecal sac narrowing at the intervertebral disc level. These same three components also cause bony lateral recess stenosis immediately below the disc level in the subarticular zone (see Figs. 41-1 to 41-9 ). In addition, herniated disc fragments or synovial cysts may occupy a normal-sized bony lateral recess and produce symptoms identical to lateral recess stenosis ( Figs. 41-10 to 41-13 ) . Therefore, it is imperative to carefully evaluate the lateral recess preoperatively in all patients undergoing discectomy or decompressive laminectomy.