Chapter Outline
Angiography of the Major Visceral Vessels
Arterial Anatomy of Specific Segments of the Gut
Vascular Diagnosis and Intervention in the Gastrointestinal Tract
Reasons for Placement of Needles or Catheters into the Gastrointestinal Tract
Diagnostic Biopsy of Bowel Masses
Over the past 2 decades, the applications of angiography and interventional radiology in hollow abdominal viscera have dramatically changed. Multidetector computed tomography (MDCT) angiography and magnetic resonance (MR) angiography have replaced much of the diagnostic angiography that had been performed for investigating mesenteric ischemia, diagnosing abdominal masses, and detecting gastrointestinal (GI) tract bleeding sites. Interventional applications in the GI tract, however, have dramatically increased. In this chapter, new developments in angiography and interventional radiology of the hollow viscera are addressed.
Preparation of Patients
Certain preprocedural steps can enhance the diagnostic quality of a visceral angiogram. For elective studies, a standard bowel cleansing should be considered to delineate vessels and pathologic findings more clearly. Intravenous (IV) glucagon (1.0 mg) given at the time of the procedure, helps reduce the effects of bowel motion, particularly in studies with digital subtraction.
A Foley catheter is useful for studies of the inferior mesenteric artery because a contrast agent filling the bladder can obscure its branches. It also increases the patient’s comfort and helps prevent unnecessary delays during long examinations.
Unless contraindicated, we routinely premedicate patients undergoing visceral angiography with fentanyl (Sublimaze) and midazolam (Versed) in an attempt to achieve the analgesic, anxiolytic, and amnestic effects of these combined agents while maintaining the patient’s ability to cooperate. All patients have intraprocedural monitoring of pulse, electrocardiogram, arterial oxygenation (via a pulse oximeter), and blood pressure.
Technical Factors
Vascular Access
In general, the femoral arterial route of catheterization is used for abdominal aortography and selective visceral angiography; the safety and ease of this approach are well established. Brachial or axillary access may be used in cases of difficult femoral access or when there is a need to advance a catheter more deeply into a vessel that has a steep caudal course.
Catheter Selection
Our catheter of choice for celiac and superior mesenteric arteriography is a simple angled visceral hook, with a single side hole. For inferior mesenteric arteriography, we prefer a catheter with a short curved tip. For most indications, 5-Fr catheters are used to minimize puncture site complications. An angiographic sheath with a check flow valve is placed to secure vascular access.
Advances in guidewire and catheter technology have made subselective catheterization of visceral vessels easier. These include the development of flexible, hydrophilic, torque control guidewires and catheters that have low coefficients of friction, which allow them to follow wires around complex or tight curves more readily. The addition of microcatheters, microwires in 0.018-inch systems, microcoils, and embolic microspheres has allowed the interventionalist to manage acute GI bleeding, regardless of the source of bleeding.
Equipment
Digital subtraction angiography (DSA) is the preferred technique for visceral angiography ( Fig. 8-1 ). In addition, digital image processing features greatly facilitate the guidance of complex vascular catheterizations and interventions. The improvement of digital subtraction systems has allowed the performance of angiography with carbon dioxide, providing exquisite angiographic images and minimizing the risk of contrast-induced nephropathy.

Angiography of the Major Visceral Vessels
Visceral angiography begins with injection of the aorta or one of the three major visceral vessels—the celiac artery, superior mesenteric artery (SMA), or inferior mesenteric artery (IMA). Aortic injection is usually limited to situations that pose a risk for selective catheterization, such as suspicion of severe narrowing or occlusion of one or more of the origins of the major visceral vessels, especially in patients with clinical evidence of intestinal ischemia or those with severe aortic atherosclerosis.
The order of examination of the visceral vessels depends on the clinical situation. Thus, in GI bleeding, angiography should begin with the vessel most likely to be bleeding based on clinical history and the results of prior diagnostic studies.
Selective catheterization of the visceral arteries can be performed as an initial step or after aortography. The celiac artery generally arises from the aorta anteriorly, at the middle T12 or upper L1 vertebral level. The SMA originates slightly caudal to the celiac trunk. Generally, 5 to 7 mL/s of contrast medium is injected into these arteries, for a total of 15 to 35 mL; the rate is based on test injections. For the IMA, which usually arises to the left of midline from the abdominal aorta at the lower aspect of the L3 vertebral body, injection at a rate of 3 to 4 mL/s for a total of 12 to 16 mL is generally appropriate. Injection rates are proportionately decreased for the mesenteric branches.
Angiography using carbon dioxide requires a different technique. It is important to remember that carbon dioxide displaces blood and does not mix with it. This causes carbon dioxide images to appear incomplete or “cut.” Most current digital subtraction systems are now equipped with software for carbon dioxide angiography. The use of stacking software is essential to postprocess the original images obtained during carbon dioxide angiography. When performing carbon dioxide angiography, it is essential to use a “closed” carbon dioxide delivery or injection system to minimize the risk of air contamination. The new CO 2 mmander system (AngioAdvancements, Fort Myers, FL) is a U.S. Food and Drug Administration (FDA)–registered portable carbon dioxide delivery system. It is composed of a converter, which is connected to a cartridge that holds up to 10,000 mL of medical grade carbon dioxide. The converter is connected to the delivery tubing, which has one-way valves to direct flow in the correct direction. The system safely delivers carbon dioxide at a low pressure and avoids air contamination and explosive delivery. Once the carbon dioxide is loaded in the injection syringe, it is gently injected into the selected artery using an end-hole or multiperforated catheter. As a general rule, no more than 200 mL of carbon dioxide should be injected within a period of 5 minutes to prevent a vapor lock effect, which is a known complication of excessive carbon dioxide injection into the arterial system.
Arterial Anatomy of Specific Segments of the Gut
The vascular anatomy of the hollow abdominal viscera is complex. We have used a number of excellent general references in preparing this chapter; the reader is referred to these for more detailed discussions of angiographic and gross anatomy and the embryologic basis for many of the observed anatomic variations.
Esophagus
From a practical standpoint, only the distal esophageal arterial supply is important for angiographers. The gastroesophageal junction is a reasonably common site of arterial hemorrhage potentially treatable by embolization or vasopressin infusion. This region is typically supplied by branches of the left gastric artery (see later) or the left inferior phrenic artery ( Figs. 8-2 and 8-3 ).


Catheterization of the upper and middle portions of the arteries that supply the esophagus is difficult but, fortunately, rarely necessary. The cervical esophagus typically receives its arterial supply from the inferior thyroid arteries (branches of the subclavian arteries), with predominant supply from the right. Subclavian, common carotid, or aortic branches may also supply this segment. The thoracic esophageal arteries arise directly from the aorta or as branches of the intercostal or bronchial arteries. Esophageal arteries anastomose along the length of the esophagus.
Stomach
The stomach has two major vascular arcades, one along the lesser curve formed by the right and left gastric arteries and the other along the greater curve, consisting of the right and left gastro-omental (gastroepiploic) arteries.
The left gastric artery usually arises as one of the three major branches of the celiac trunk, originating anywhere from the orifice of the trunk to the hepatic-splenic bifurcation ( Figs. 8-4 to 8-6 ; see also Figs. 8-2 and 8-3 ). In 2% to 6% of patients, this vessel arises separately from the aorta.



A replaced or accessory left hepatic artery arises from the left gastric artery in 20% to 30% of cases. This has important clinical implications in patients for whom embolization or infusion therapy of hepatic or gastric arteries is anticipated. When this variant is present, the relative blood supply to the stomach and liver can vary, so that minimal supply to either may be present. In about 5% of cases, one or both inferior phrenic arteries arise from the left gastric trunk; this association is much higher when the left gastric artery arises as a separate aortic branch. The importance of this variant is emphasized by the reported association of hypertension and cardiac arrhythmias with vasopressin infusion into the phrenic artery. Accessory left gastric arteries are common.
Because most gastric angiography is performed for GI bleeding, and left gastric arterial ramifications account for about 85% of gastric hemorrhages, this is clearly an important vessel for subselective catheterization. Unfortunately, whereas the celiac artery is most readily catheterized with a caudally directed catheter, the course of the left gastric artery is cephalad. This may make selective catheterization difficult. A number of articles and texts have detailed methods that facilitate catheterization of this sometimes elusive vessel. The basic principle of these procedures is initial selection of the celiac artery with a catheter that has a caudally directed tip, followed by intraceliac exchange for, conversion to, or coaxial insertion of a catheter with a tip that points upward.
The right gastric artery arises at or distal to the common hepatic artery bifurcation, usually from the proper hepatic (57%) but occasionally from the left (17%) or right hepatic (2%) branches or at the origin or proximal portion of the gastroduodenal artery (10%). It has generally been considered an unimportant vessel for arteriographers, along with the cystic and falciform arteries; however, these small vessels are found to be of increasing concern with the evolution of transarterial chemoembolization and arterial brachytherapy. Because the right gastric and cystic arteries have variable origins, these vessels increase the possibility of nontarget embolization, with subsequent tissue necrosis and/or inflammation (e.g., mucosal ulceration, cholecystitis, skin necrosis).
The right gastro-omental (gastroepiploic) artery is typically the larger of the two gastro-omental vessels (see Figs. 8-2, 8-4, and 8-5 ). It is the terminal branch of the gastroduodenal artery. The left gastro-omental (gastroepiploic) artery arises from the splenic artery or in conjunction with its inferior splenic branch (see Fig. 8-4 ). The gastro-omental arteries anastomose in a well-formed arcade along the greater curve of the stomach in 65% to 75% of cases; in most other cases, an anastomosis is still present but is not as well developed. In slightly fewer than 50% of individuals, a parallel anastomotic arcade called the arc of Barkow is present in the greater omentum, joining the right and left omental arteries, branches (respectively) of the right and left gastro-omental arteries (see Figs. 8-4 and 8-5 ).
The supply from the gastric and gastro-omental arcades is supplemented by other branches. A variable number of short gastric arteries supply the fundus and superior aspect of the greater curve of the stomach, usually arising from splenic hilar vessels (see Figs. 8-4 and 8-5 ). In 36% to 60% of individuals, a posterior gastric artery arises from the main splenic artery to supply the posterior wall of the stomach and parts of the fundus and gastroesophageal junction. The pyloric region typically receives part of its supply via branches of the gastroduodenal artery.
Small Bowel
Much of the blood supply to the duodenum is via a series of freely anastomosing vessels; the anterior and posterior pancreaticoduodenal arcades provide a rich source of collaterals for the duodenum and head of the pancreas and between the celiac artery and SMA. These arcades (usually dual) form a continuous loop along the descending and transverse duodenum and the pancreatic head. The superior origin of this complex is usually dual, with both branches arising from the gastroduodenal artery and the posterior arcade typically arising more cephalad than the anterior ( Fig. 8-7 ; see also Figs. 8-5 and 8-6 ). The inferior origin is usually a single trunk, usually arising from the SMA or its first or second jejunal branch (see Figs. 8-5 and 8-7 ).

Other sources of duodenal perfusion are branches of the right gastro-omental artery, supraduodenal artery (which has many possible origins, including the hepatic artery, gastroduodenal artery, posterior pancreaticoduodenal arcade, and right gastric artery), and smaller gastroduodenal branches.
In addition to the pancreaticoduodenal arcades, another potential collateral route between the celiac and superior mesenteric territories is the arc of Buhler, which represents persistence of an embryologic anastomosis between the celiac and superior mesenteric trunks.
The jejunum and ileum are supplied primarily by multiple branches arising from the left side of the SMA ( Figs. 8-8 and 8-9 ); the level of the ileocolic artery origin is a good general indicator of the division between jejunal and ileal territories. The distal ileum also receives blood from the ileocolic artery (see later). An extensive network of vascular arcades connects the jejunal and ileal branches; along the mesenteric border of the small bowel, the distal arcades give rise to multiple straight vasa recta that enter the bowel wall. The number of arcades increases, and the length of the vasa recta decreases more distally in the small bowel; these anatomic factors must be considered when performing small bowel embolization.


An important anatomic variant is a persistent vitelline artery, indicating the presence of Meckel’s diverticulum. This vessel has a characteristic appearance—a relatively long vessel arising in the ileal region, without anastomoses to other ileal branches and with a network of irregular small distal branches ( Fig. 8-10 ). Meckel’s diverticulum may also be supplied by ileal branches without a well-defined vitelline artery, although this is less common. A dense mucosal stain at the tip of the diverticulum suggests the presence of ectopic gastric mucosa.

Colon and Rectum
The right colon and transverse colon are usually supplied by the SMA. Classically, this supply is described and diagrammed as consisting of three main branches arising independently from the SMA—the ileocolic, right colic, and middle colic arteries. Although the ileocolic is a constant vessel, a true right colic artery (arising independently from the SMA) is uncommon, and the middle colic “artery” is frequently variable in extent and branching pattern, consisting of one or more of five distinct vessels. The discrepancy between the classic description of three main independent branches and the most common situation, in which there are two independent branches, has given rise to some confusion and has caused the termination of the SMA to be labeled as the ileocolic artery on angiograms in various anatomic texts. It should be emphasized that the SMA termination is not a colic artery: its branches supply the ileum, and its final terminus joins the ileal branch of the ileocolic artery in a vascular arcade at the ileocecal junction.
The ileocolic artery supplies the transition between the small bowel and colon, with branches to the terminal ileum, cecum, ascending colon, and appendix (see Figs. 8-8 and 8-9 ). It is the last branch arising from the right side of the superior mesenteric trunk, and its constancy makes it a very important angiographic landmark. Most often, it consists of a main stem branching into two cecal branches distally, with anastomotic branches arising along the main stem. A nearly constant branch of the ileocolic artery is the superior colic, which anastomoses with the next colic artery arising from the SMA, whether the right colic or part of the middle colic complex.
The designation of right colic artery should apply only to an independent branch arising directly from the superior mesenteric trunk that supplies the middle portion of the ascending colon. The midportion of the ascending colon is usually supplied via an arcade formed between the ileocolic artery and middle colic system.
The middle colic artery has been classically described as the major proximal branch of the SMA, which supplies the right colonic flexure and transverse colon. A true middle colic artery is actually seen in slightly fewer than 50% of cases. In other cases, variant arteries or combinations of these arteries supply the vascular territory between the ileocolic or right colic artery and the left colic artery; a single vessel is present 75% of the time (see Figs. 8-8 and 8-9 ).
The middle colic artery or accessory arteries to the middle colic territory can arise from the celiac, splenic, hepatic, or pancreatic arteries (especially the dorsal pancreatic artery; Fig. 8-11 ). Thus, angiography of the entire colon may require injection of the celiac artery or its branches.

In unusual situations, portions of the blood supply to the colon can arise directly from the aorta between the origins of the SMA and IMA. In two publications, such a variant has been called the middle mesenteric artery, although in one report the artery supplied the distal transverse and proximal descending colon, and in the other the artery supplied the entire proximal colon, up to and including the splenic flexure.
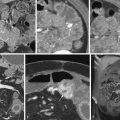
The IMA usually supplies the splenic flexure, descending colon, sigmoid colon, and upper rectum IMA ( Figs. 8-12 to 8-15 ). However, the boundary between the parts of the colon supplied by the SMA and IMA can be variable—proximal or distal to the splenic flexure. The IMA terminates in two superior rectal (hemorrhoidal) branches (see Figs. 8-12 and 8-13 ). It gives off branches from its left side. The first is the left colic artery, which courses toward the splenic flexure (see Figs. 8-12 , 8-14 , and 8-15 ). Its branches anastomose with branches of the middle colic territory (see Figs. 8-12 and 8-15 ). The left colic artery is frequently absent if there is an accessory left colic vessel arising as a portion of the middle colic supply. Other branches arise from the left colic artery or IMA trunk proximal to the superior rectal arteries to supply the descending and sigmoid colon and upper rectum. A colosigmoid artery or branch (see Figs. 8-13 and 8-14 ) can usually be identified as a large dominant vessel supplying the transition between the descending colon and sigmoid.




The marginal artery of Drummond designates a vascular arcade that runs along the mesenteric border of the colon, where it gives off its nutrient vessels ( Figs. 8-16 and 8-17 ; also see Figs. 8-12, 8-14, and 8-15 ). Defined in this way, the major colic arteries can parallel the marginal artery or constitute part of it; the paracolic arcade can be considered part of the generalized system of paraintestinal arcades present throughout the abdominal GI tract. An enlarged marginal artery frequently provides a collateral pathway between the SMA and IMA territories (see Figs. 8-16 and 8-17 ). The marginal artery is not always reliably complete along its entire length. Griffith’s point, for example, represents a watershed area of a potentially poor anastomotic connection between the SMA territory and marginal artery of the descending colon at the splenic flexure; it is an area susceptible to ischemic injury when its marginal artery is poorly developed. The arc of Riolan refers to a more central anastomotic loop that lies within the mesentery, joining the IMA and SMA territories. The term meandering mesenteric artery has also been used. This actually represents an enlarged and tortuous left colic artery acting as part of a collateral pathway (see Figs. 8-16 and 8-17 ).


The more distal rectum is supplied by branches of the internal iliac territory, the middle rectal and inferior rectal arteries. As is the case with the most proximal portion of the gut, angiography of this region is infrequently performed. Collateralization via the rectal arteries between the IMA and internal iliac system can become important in occlusive disease of the aorta and common iliac arteries.
Venous Anatomy
The mesenteric venous system is studied for two main indications: (1) evaluation of the patency of the mesenteric veins in the setting of suspected acute mesenteric ischemia; and (2) evaluation of the patency and direction of flow in the mesenteric, splenic, and portal veins and potential collateral pathways in portal hypertension. Angiography in patients with portal hypertension may be difficult to interpret, and images of high quality are essential. A very good mesenteric venous phase can be obtained using a total volume of 35 mL of nonionic contrast at an injection rate of 5 to 7 mL/s. The use of glucagon (1-mg IV bolus) to slow down the peristalsis and vasodilators to increase the flow improve the quality of the images. Vasodilators may include papaverine (30-mg intra-arterial bolus, followed by a 10-mL saline flush to prevent papaverine crystallization) or tolazoline (Priscoline), 25 mg diluted in 10 mL of normal saline solution, injected slowly for 2 minutes. Contrast medium injection and filming begin immediately after drug administration.
The most important gastric vein is the left gastric, or coronary vein, which courses along the lesser curve of the stomach and joins the splenic-portal venous system at variable sites. It is a frequent pathway for portosystemic collateralization in portal hypertension and splenoportal collateralization in splenic vein occlusion. Gastro-omental and short gastric veins parallel their respective arteries and can be important collateral pathways as well. The superior mesenteric and inferior mesenteric veins run to the right of, parallel to, and drain the respective territories of the SMA and IMA. The superior mesenteric vein joins the splenic vein behind the pancreatic neck to form the portal vein (see Fig. 8-1 ); the inferior mesenteric vein can join the splenic or superior mesenteric vein or their confluence ( Fig. 8-18 ).