Chapter 6 Antepartum fetal surveillance
Antenatal care should be appropriate and effective. The low-risk mother will be seen largely by the midwife in community antenatal clinics. Higher-risk mothers will be seen in hospital antenatal clinics often by doctors. All require access to antenatal testing facilities. Recent years have seen a proliferation of maternofetal assessment units or day-care units. The benefits of this include the gathering together of the various tests with the compilation and review of results. Daily outpatient assessment and review may be undertaken where previously admission to hospital was the norm. However, easy access may result in excessive testing with largely normal results. Protocols of referral should be formulated and audit undertaken. An assessment unit should be located near the ultrasound department because testing can be integrated with ultrasound examination. The focus of fetal assessment is the antenatal cardiotocograph (CTG). Appropriate equipment is the Sonicaid Team, Hewlett-Packard 1351, Corometrics 118 or Huntleigh Baby Dopplex 3000. The Sonicaid System 8000 is an additional option which has a particular value in providing electronic storage of the CTG. Caution should be exercised in depending on computerized trace analysis with consequent risk of the loss of human skills of interpretation. A data collection computer has become essential. The unit should be staffed by motivated midwives who can diversify their clinical interest. They should have the support of available and interested medical staff in assessment of problem cases. The individual requesting the test should be aware of the result in order to plan and justify the further management. This should not be delegated by default to a junior member of staff.
IDENTIFICATION OF THE FETUS AT RISK
There are two groups of women who may require fetal assessment:
1. Women with previously recognized historical risk factors such as previous stillbirth and neonatal death, or medical disorders such as diabetes mellitus, hypertension or other conditions.
2. Lower-risk women who develop obstetric complications during pregnancy such as antepartum haemorrhage, hypertension, reduced fetal movement, intrauterine growth restriction, cholestasis or prolongation of pregnancy.
FETAL GROWTH
The abdomen may be judged to be a different size from that expected from the dates. More commonly this is smaller rather than larger. The importance of detecting small babies in utero has been emphasized in Chapter 2.
The clinical scenario may indicate a risk of hypoxic intrauterine growth restriction (IUGR) in well-recognized situations: previous IUGR baby, malnourished mother, smoking, alcohol, drug abuse, medical conditions, gestational hypertension, multiple pregnancy and other conditions. The measurement of the fundosymphysis height (see Figs 2.1 and 2.2) in cm, given that the fetus is a single fetus in a longitudinal lie, is plotted on a chart or simply compared with the gestational age in weeks. If it is more than 2 cm smaller than the gestational age before 36 weeks or 3 cm thereafter, then it is clinically small for dates. The confounding effects of abnormal lie, obesity, fibroids, multiple pregnancy and polyhydramnios have already been mentioned.
Clinically small for dates is an indication for an ultrasound scan.
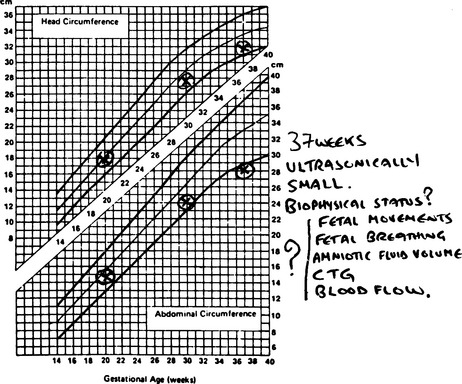
On ultrasound examination measurements of head circumference (HC), abdominal circumference (AC) and femur length (FL) are taken and plotted on a growth chart (Fig. 6.1). The AC reflects fetal weight most accurately and if it falls below the 5th centile, this is ultrasonically small for dates. Customized fundosymphysial growth charts based on ethnicity, parity, height and weight of the mother are available (http://www.gestation.net)19 and are said to identify more cases of IUGR than conventional measurement with the tape which is plotted on a ‘gravidogram’ (fundosymphysial height plotted in relation to gestation). Similarly customized growth charts are available to plot the estimated fetal weight based on ultrasound measurements.19 A fetus that is ultrasonically small may be an expected small baby due to small parents, i.e. genetic smallness. Alternatively a small fetus may be pathologically small due to an abnormal process. To distinguish one from the other the following should be taken into account:
• subjective and objective fetal movements
• other biophysical elements: fetal breathing, fetal tone, blood flow velocity waveform in the fetal vessels by Doppler ultrasound.
Not all small fetuses are suffering from IUGR.
A growth-restricted baby is one that has not realized its own intrinsic growth potential.
BIOPHYSICAL MONITORING OF FETAL HEALTH
Fetal movements
Fetal activity in the form of fetal movement perceived by the mother is a reliable indicator of fetal health. Women should be encouraged to be aware of this. A reduction in fetal movement of concern to the mother is an indication for careful assessment, initially by CTG followed by an ultrasound assessment. An appropriate abdominal circumference and normal amniotic fluid volume on ultrasound are reassuring and often the fetus is seen to be active during the scan. The woman will also see this and be reassured. Commonly the fetus recommences normal movements and there is no need for further assessment.
In a randomized study involving 68 000 women routine use of fetal movement charts was not beneficial compared with more selective use.20 Reduced or no movements predicted poor perinatal outcome but this could not be prevented. This may be partly to do with different reporting times in the study and inadequate surveillance, i.e. late surveillance or being only dependent on the CTG. The commonly-used chart is the Cardiff ‘Count to Ten’ chart. Sadovsky, who studied fetal movement extensively, suggested that there should be four fetal movements in a 30-min period during one day of which one has to be strong.21 The expectation of four fetal movements in 30 min or 10 in 12 h is arbitrary and correlated with good perinatal outcome.22–24 A single fetal movement felt by the mother may not be recorded by the ultrasound movement detection devices. However, when a mother feels clusters of fetal movements for 15–20 s it is detected by the ultrasound transducer and is almost always associated with fetal heart rate (FHR) accelerations (see Fig. 5.19).25 Women should be encouraged to be reassured by clusters of fetal movements.
Increased fetal activity can lead to confluence of accelerations mimicking a fetal tachycardia, and the synchronous automatic recording of fetal movements as done by the newest monitors will help to clarify this situation.26 There are monitors using actograms that attempt to record fetal movement and fetal breathing in addition to the FHR. The clinical application of this principle remains to be proven.
Antepartum electronic fetal heart rate monitoring
Non-stress test
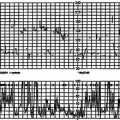
The recording of the FHR for a period of 20–30 min without any induced stress to the fetus (like oxytocin infusion or nipple stimulation) to produce uterine contractions is called the non-stress test (NST). In the UK this is commonly referred to as an antenatal CTG. The duration of this test should be until reactivity is observed; until there are two accelerations in a 10-min period. The sleep phase with no fetal movement and no FHR accelerations does not exceed 40 min in the vast majority of healthy fetuses and almost all healthy fetuses show a reactive trace within 90 min.27 This forms the framework for extending the NST for 40 min when it is not reactive in the first 20 min. In some centres vibro-acoustic stimulus is used to provoke activity if there is no reactivity for 40 min.
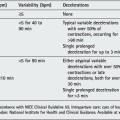
A summary of the interpretation of the NST based on the International Federation of Obstetrics and Gynaecology (FIGO) recommendations12 and the actions that are recommended with each type of trace are given below.
Antepartum cardiotocograph (NST)
Normal/reassuring
• At least two accelerations (>15 beats for >15 s) in 10 min (reactive trace), baseline heart rate 110–150 beats per min (bpm), baseline variability 5–25 bpm, absence of decelerations.
• Sporadic mild decelerations (amplitude <40 bpm, duration <30 s) are acceptable following an acceleration.
• When there is moderate tachycardia (150–170 bpm) or bradycardia (100–110 bpm), a reactive trace without decelerations is reassuring of good health.
Interpretation/action: Repeat according to clinical situation and the degree of fetal risk.
Suspicious/equivocal
• Absence of accelerations for >40 min (non-reactive).
• Baseline heart rate 150–170 bpm or 110–100 bpm, baseline variability >25 bpm in the absence of accelerations.
• Sporadic decelerations of any type unless severe as described below.
Interpretation/action: Continue for 90 min until trace becomes reactive, or repeat CTG within 24 h, or vibro-acoustic stimulation (VAS)/amniotic fluid index (AFI)/biophysical profile (BPP)/Doppler ultrasound blood velocity waveform.
Pathological/abnormal
• Baseline heart rate <100 bpm or >170 bpm.
• Silent pattern <5 bpm for >90 min.
• Sinusoidal pattern (oscillation frequency <2–5 cycles/min, amplitude of 2–10 bpm for >40 min with no acceleration and no area of normal baseline variability).
• Repeated late, prolonged (>1 min) and severe variable (>40 bpm) decelerations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree