Abstract
Aortic coarctation consists of a constriction of the aortic arch that causes some degree of aortic arch hypoplasia. The suspicion of coarctation of the aorta must be raised in the presence of a discrepancy in the size of the left heart. However, the false-positive rate is high. There is a high risk for associated anomalies, particularly for cardiac and extracardiac abnormalities. The overall prognosis in isolated defects is good.
Keywords
congenital heart defect, aortic coarctation, hypoplastic left heart
Introduction
Aortic coarctation (AoC) is a ductal-dependent heart anomaly characterized by a narrowing of the aorta. The presence of physiologic right-to-left shunts in the fetal circulation constitutes a challenge for prenatal diagnosis, making AoC one of the congenital heart diseases (CHDs) with the most common false-positive and false-negative diagnoses.
Disease
Definition
AoC consists of a constriction on the aortic arch that causes obstruction of the blood flow and consequently causes some degree of aortic arch hypoplasia. The constriction can affect a variable length of the vessel or consist on a shelf-like obstruction. The constriction is usually located at the level of the aortic isthmus, between the left subclavian artery and the ductus arteriosus.
Prevalence and Epidemiology
AoC accounts for 7% of all CHDs, and affects 1 : 1600 newborns. It is twice as common in males, and is frequently associated with other CHDs, especially ventricular septal defects and left heart obstructive lesions.
Etiology and Pathophysiology
The etiology is unknown. AoC is usually a multifactorial disease, although familial inheritance has been described. It can be associated with chromosomal abnormalities and genetic syndromes, including Turner syndrome in 30% of cases, as well as trisomy 21 and 18, and 22q11 microdeletion. Various theories have been proposed for the development of coarctation of the aorta, such as a reduced flow through the aortic arch or the presence of a ductal sling.
AoC can be classified according to its location in relation to the ductus arteriosus. Preductal AoC is the most frequent form in fetal and neonatal life. It is usually associated with other CHDs and can be suspected prenatally. Reduced blood flow leads to underdevelopment and tubular hypoplasia of the aortic arch previous to the constricted area.
Postductal AoC is typically diagnosed during childhood. It is usually an isolated CHD with a normal aortic arch, but a localized “shelflike” constriction with proximal tapering of the aorta.
Manifestations of Disease
Clinical Presentation
It depends on the severity and location of the obstruction and the presence of associated anomalies. Neonates are usually asymptomatic until postnatal closure of the ductus arteriosus. Severe cases lead to blood-flow obstruction to the left heart and eventually heart failure, shock, and even death during the first weeks of life. Less severe or postductal AoC can be misdiagnosed until childhood or adulthood.
Imaging Technique and Findings
Ultrasound.
Coarctation of the aorta is the CHD with the highest rate of false-positive and false-negative diagnoses. The coarctation site itself is difficult to identify, so suspicion of AoC relies on indirect signs, mainly a size discrepancy between the left and right chambers and outflow tracts on four-chamber view, or three-vessel and tracheal views. To assess the disproportion objectively, z scores for right and left measurements and ratios can be calculated. Recent data suggests that gestational age-specific scoring systems combining size-based cardiac parameters may improve the accuracy of fetal echocardiography to stratify the risk of AoC.
- •
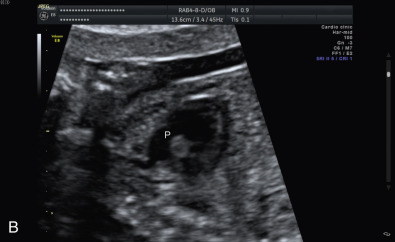
Ventricular disproportion is the classic sign identified on the four-chamber view. The right ventricle appears larger than the left ventricle with a subjectively larger inflow by color Doppler ( Fig. 82.1 and ). Severe cases show inversion of the interatrial shunt (left-to-right flow). Ventricular disproportion can be present not only in AoC and other CHDs but also in extracardiac fetal conditions, such as growth restriction, maternal drug intake, and fetal anemia. In addition, the right ventricle becomes more dominant with advancing gestational age, which further challenges the accurate diagnosis of AoC. For this reason, the positive predictive value is only 30%, particularly when the suspicion is established in late pregnancy.

Fig. 82.1
Severe ventricular disproportion. The left ventricle (LV) is smaller than the right ventricle (RV).
- •
There is a disproportion of outflow tracts as well, with a larger pulmonary artery compared with the aorta ( Fig. 82.2 ).