Most renal masses are benign cysts; a subset are malignant. Most renal masses are incidental findings. Evaluation of renal cysts has evolved with updates to the Bosniak classification system and other guidelines. The Bosniak classification provides detailed definitions and extends the system from computed tomography to MR imaging. This article provides a simple approach to the evaluation of cystic or potentially cystic renal masses. The radiologist is central to this process. Key elements include confirming that a renal lesion is cystic and not solid, determining the need for further characterization by imaging, and judicious application of the Bosniak classification system.
Key points
- •
The first step in evaluation of a renal mass is to determine if it is cystic or solid and apply the Bosniak classification system version 2019.
- •
The need for additional characterization depends on the initial imaging modality and the imaging features that can be used for Bosniak classification.
- •
The Bosniak classification should not be applied to cystic appearing infectious, inflammatory, or vascular etiologies; for all other renal cystic masses with imaging that allows for a complete characterization, the Bosniak classification should be applied.
Is it a renal cyst?
The first step in the evaluation of a renal mass is to determine if it is cystic or solid. Completing this task is critical for management, and the imaging modality is important. The Bosniak classification system version 2019 considers a renal lesion with less than 25% enhancing tissue as cystic, but multiple other definitions for defining a renal cyst now apply and are described elsewhere in this article. In general, the use of colloquial terms that lack standard definitions, such as “complicated cyst” or “complex cyst,” should be avoided, although these terms are common in clinical practice for indeterminate renal cysts that require further characterization by renal computed tomography (CT) scan or MR imaging or renal ultrasound examination.
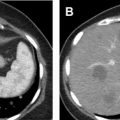
One of the most commonly encountered renal lesions on CT scan are those that are considered too small to characterize (TSTC) owing to problems with volume averaging when attempting to assess the attenuation. Homogeneous low-attenuating renal lesions that are TSTC are now considered benign cystic masses. By comparison, a heterogenous renal lesion that is TSTC by CT scan is rarely encountered, but is indeterminate and cannot be assumed to represent a renal cyst, because some of these lesions may represent solid renal neoplasms ( Fig. 1 ). ,

To characterize a larger renal lesion on CT scan, a region of interest is used to assess the attenuation in Hounsfield units (HU). If the attenuation of 75% or more of a renal lesion on noncontrast or contrast-enhanced CT scanning measures as fluid attenuation (−9 to 20 HU), it can be considered cystic. , , The cystic component of a renal cyst may not measure fluid in attenuation, and enhancement is key to differentiating a hyperdense renal cyst from a solid renal neoplasm. Renal masses with less than 25% enhancing tissue are considered cystic, with enhancement on CT scans defined as an increase of 20 HU or more between noncontrast and contrast-enhanced images, most commonly from dedicated renal protocol CT acquisition. , In addition, homogeneous hyperattenuating (≥70 HU) renal lesions at noncontrast CT scanning and homogenous renal lesions measuring −9 to 30 HU at portal venous phase CT scanning are considered benign cystic masses. , , By comparison, all heterogeneous masses at noncontrast CT scanning are considered indeterminate and could be cystic or solid in nature. ,
The role and reliability of dual energy CT scanning for characterizing renal masses is under investigation in research studies and not yet incorporated into the Bosniak classification system. , More validation is needed in this area of research. Given the decreased importance of renal enhancement in the Bosniak classification system version 2019, characterization and Bosniak classification of many well-defined renal cysts on dual energy CT images may be possible, especially if 75% or more of the renal mass measures fluid attenuation (−9 to 20 HU) at 120 kV imaging.
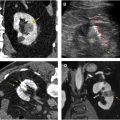
On MR imaging, a renal cyst is defined as a renal mass with less than 25% enhancing tissue, with enhancement defined as an increase of 15% or more in signal intensity between contrast-enhanced and noncontrast images or as definitive visual enhancement on high-quality subtraction images. , On noncontrast MR imaging, homogeneous masses markedly hyperintense at T2-weighted imaging (similar to cerebrospinal fluid) and homogeneous masses markedly hyperintense at fat-saturated T1-weighted imaging (approximately 2.5 times normal renal parenchymal signal intensity) are considered benign cystic masses (Bosniak type II). , Conversely, homogeneous renal masses with mild to moderate intensity at T1- or T2-weighted imaging or heterogenous masses on noncontrast MR imaging are indeterminate and cannot be classified as cystic without further characterization. Furthermore, heterogeneously hyperintense renal masses at fat-saturated T2-weighted imaging cannot be classified as cysts, because some represent necrotic papillary cancers.
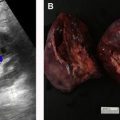
On ultrasound examination, a renal cyst is anechoic or hypoechoic with posterior acoustic enhancement (or increased through-transmission). The posterior acoustic enhancement is a key feature, as some solid masses can be hypoechoic but lack posterior acoustic enhancement. Additional features such as debris, wall thickening, color flow, and number, thickness, and nodularity of septations can also be evaluated and should be used to assist with characterization. On contrast-enhanced ultrasound examination, a renal cyst is defined as a renal lesion with less than 25% enhancing tissue.
Does this renal mass need further characterization?
The need for additional characterization of a renal mass depends on the initial imaging modality and the imaging features that can be used for Bosniak classification ( Table 1 ). With the exception of homogeneous renal lesions that are TSTC, if a renal lesion is not well-defined or not clearly cystic, further characterization by imaging is needed. Most renal lesions are detecting on noncontrast or portal venous CT examinations that are obtained for other purposes, and the Bosniak 2019 classification leads to confident characterization as benign cystic lesion, although for a minority of cases the Bosniak rules cannot be applied completely without additional imaging. A review of renal masses requiring further characterization by additional imaging is presented in Table 2 .
| Class | CT Scan a | MR Imaging a | Ultrasound Examination c |
|---|---|---|---|
| I | Well-defined cyst with thin (<2 mm) smooth wall; homogeneous simple fluid (−9 to 20 HU); no septa or calcifications; the wall may enhance | Well-defined cyst, thin (≤2 mm) smooth wall; homogeneous simple fluid (signal intensity similar to CSF); no septa or calcifications; the wall may enhance | Well-defined cyst (anechoic with posterior acoustic enhancement), thin (≤2 mm) smooth wall; no septa or calcifications |
| II |
|
|
|
| IIF | Cystic masses with a smooth minimally thickened (3 mm) enhancing wall, or smooth minimal thickening (3 mm) of ≥1 enhancing septa, or many (>4) smooth thin (<2 mm) enhancing septa |
| Cystic masses with a smooth minimally thickened (3 mm) wall that may have color flow, or smooth minimal thickening (3 mm) of ≥1 septa that may have color flow, or many (≥4) smooth thin (≤2 mm) septa that may have color flow; may have well-defined calcification that does not obstruct other imaging features |
| III | ≥1 enhancing thick (>4 mm width) or enhancing irregular (displaying <3-mm obtusely margined convex protrusion[s]) walls or septa | ≥1 enhancing thick (≥4 mm width) or enhancing irregular (displaying ≤3-mm obtusely margined convex protrusion[s]) walls or septa | Not applicable to routine renal ultrasound examination c |
| IV | ≥1 enhancing nodule(s) (>4-mm convex protrusion with obtuse margins, or a convex protrusion of any size that has acute margins) | ≥1 enhancing nodule(s) (≥4-mm convex protrusion with obtuse margins, or a convex protrusion of any size that has acute margins) | Not applicable to routine renal ultrasound examination c |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree