Introduction
Undifferentiated chest pain presents a diagnostic dilemma because there are many potential causes, with some etiologies being imminently life threatening. These diagnoses often cannot be determined by history or physical examination alone. Patients may be hypotensive or deteriorate quickly, requiring emergent procedures. For these reasons, point-of-care ultrasound (POCUS) is used to evaluate chest pain.
The most urgent systems to evaluate are cardiac, aortic, and pulmonary, which can be performed together using a “focused chest” algorithm. Multiple algorithms exist, including a 5Es approach to review cardiac pathology, the SEARCH 8Es approach to assess the lung and heart, and a modified rapid ultrasound for shock and hypotension (RUSH) examination. Different algorithms prioritize ultrasound views in different orders. We recommend starting with the view most likely to yield a diagnosis based on initial history and physical.
Technique
Because the heart is an essential organ upon which life depends, echocardiographic views are often obtained first to evaluate for life-threatening and immediately reversible causes.
Cardiac
The 5Es approach is a problem-driven algorithm. The assessment for pathology is largely qualitative.
- •
Effusion—Is there a pericardial effusion? Is there cardiac tamponade?
- •
Parasternal long or short axis, apical four-chamber, or subxiphoid views
- •
- •
Ejection (fraction)
- 1.
Is the left ventricular function preserved or depressed?
- •
Parasternal long or short axis, apical four-chamber, or subxiphoid views
- •
- 2.
Is there acute focal wall motion abnormality indicating acute myocardial infarction?
- •
Mainly parasternal short axis, complemented by parasternal long axis or apical four-chamber view
- •
- 1.
- •
Equality—Is the right ventricle (RV) enlarged compared with the left ventricle indicating an acute obstructive process such as pulmonary embolus (PE)?
- •
Parasternal long or short axis, apical four-chamber views
- •
- •
Exit—Is there thoracic aortic dilation or dissection?
- •
Parasternal long-axis (PSLA) view specifically measuring the aortic outflow tract (AOT)
- •
The PSLA view should be performed at a depth great enough to visualize and measure the descending thoracic aorta in the same view
- •
- •
Entrance—What is the volume status (preload) entering the heart? Is there hypervolemia or obstruction to blood flow?
- •
Subxiphoid long-axis view reviewing inferior vena cava (IVC) distensibility and respirophasic variations
- •
If possible, obtain at least two views to confirm findings. Patient acuity, mobility, body habitus, and time constraints are all factors that may limit the number of views that can be obtained.
Although valve assessment has not been incorporated into routine algorithms for chest pain echocardiographic assessment, concern for a new murmur or entities such as critical aortic stenosis should prompt valvular evaluation.
Pulmonary
- •
Is there a pneumothorax?
- •
Sagittal view obtained in the second intercostal space
- •
Review for lack of pleural sliding: M-mode or power Doppler may be used for assistance
- •
- •
Is there significant pulmonary edema (chest pain from cardiac demand)?
- •
Sagittal view obtained in the second intercostal space
- •
Review for B-lines, which are vertically extending reverberation artifacts through the whole depth of field
- •
- •
Is there pleural effusion or consolidation (chest pain from pleurisy)?
- •
Coronal view obtained in the right and left upper quadrant flanks cephalad enough to see the pleural space above the diaphragm
- •
Review the pleural space for the presence of pleural effusion (hypoechoic) or consolidations from pneumonia or masses (with hepatization containing air bronchograms)
- •
In the presence of pathology, a “spine sign” will be seen, with the thoracic spine visualized extending cephalad past the diaphragm
- •
Other lung views may be obtained if time is not limited.
Other Applications to Consider
If no reasons for chest pain etiology are found using echocardiographic and thoracic views, other etiologies can be considered.
- •
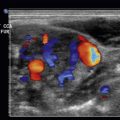
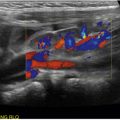
Is there a deep vein thrombosis (DVT)?
- •
If a DVT is found, it may mean that chest pain can still be caused by a PE that is not extensive enough to cause evidence for RV enlargement or strain on echocardiography evaluation
- •
Evaluate the saphenofemoral junction, common femoral vein, and popliteal vein to its trifurcation
- •
- •
Does the patient have symptomatic cholelithiasis or cholecystitis causing chest pain that radiated from the epigastric region or right upper quadrant?
- •
Evaluate the gallbladder for presence of stone, thickened gallbladder wall, and pericholecystic fluid
- •
The Views of This Algorithm
An algorithmic approach has been shown to narrow the differential diagnoses and increase diagnostic confidence and accuracy in the setting of dyspnea, chest pain, or symptomatic hypotension ( Fig. 13.1 ).

Examples and Cases
The following cases exemplify the use of an ultrasound protocol, such as the one we propose, as well as examples of the pathology ultrasound can help uncover.
Case 1. Regional Wall Motion Abnormality
A 67-year-old male with a history of hypercholesterolemia on medications, prior negative stress test several years ago, and no diagnosed coronary artery disease presents to the emergency department with chest pain that started 3 hours prior. It is described as tight, nonradiating, and associated with nausea and diaphoresis. It improved with nitroglycerin administered in the ambulance. Electrocardiogram (EKG) showed J-point elevations in V1 and V2 without reciprocal changes, T wave, or ST-segment abnormalities.
Given the concerning patient history and nondiagnostic EKG, a point-of-care ultrasound was performed, clips of which are provided in Figs. 13.2 to 13.8 and .







Ultrasound evaluation detected a posterior wall motion abnormality in the parasternal long- and short-axis views. An apical four-chamber view was not recorded for this patient. Evaluation also showed the presence of lung sliding, absence of B-lines, absence of pleural effusions, and a normal-sized, collapsible IVC. The combination of findings argued against pneumothorax, pneumonia, pericardial effusion, and dissection. The study revealed a focal wall motion abnormality consistent with acute coronary syndrome.
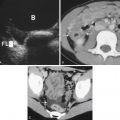
Case 2. Aortic Dissection
A 50-year-old male smoker with no significant medical problems was mowing the lawn and developed substernal chest pain, described as pressure with a dull component between the shoulder blades. Vital signs were normal, except for hypertension to 159/77 mm Hg. EKG was normal, and troponin negative. A point-of-care ultrasound was performed to elucidate the etiology of the chest pain, clips of which are provided in Figs. 13.9 to 13.14 and .