Clinical Presentation
The patient is a 67-year-old woman who presented in early 2005 with mild, low back pain and severe pain and numbness from the knees down. The patient gave a history of back surgery 40 years previously and has had some problems with her back ever since. She had an epidural steroid injection in February 2004 but began to feel numbness in her left leg, beginning in July 2004 that progressed to bilateral leg pain and tingling in the feet. The pain from her knees down was rated at 8/10 and was characterized as deep, achy, and burning. Her pain occurred with activity and at rest. The patient denied any bowel or bladder symptoms.
Imaging Presentation
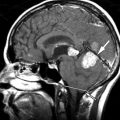
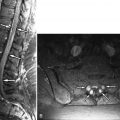
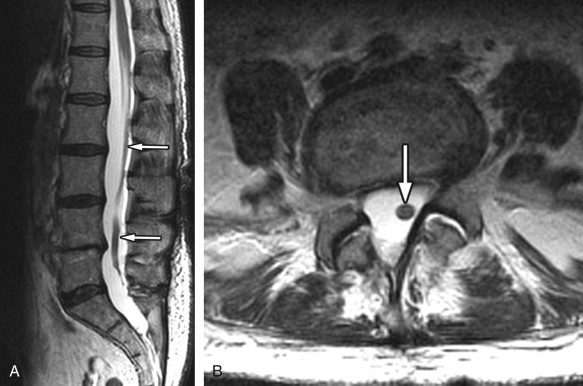
Sagittal and axial T2-weighted magnetic resonance (MR) images reveal a single thickened cord of soft tissue extending from a normal-appearing and normal-positioned conus medullaris to the lumbosacral junction. The thecal sac has a featureless appearance, and one does not see the normal intrathecal nerve roots that would be expected. This thickened cord represents adhesion of the intrathecal nerve roots into a solitary cord ( Fig. 10-1 ) .
Discussion
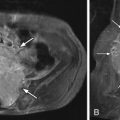
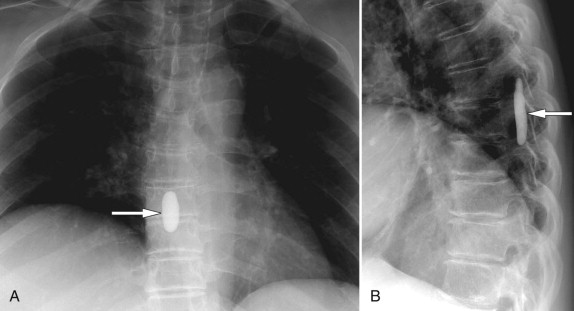
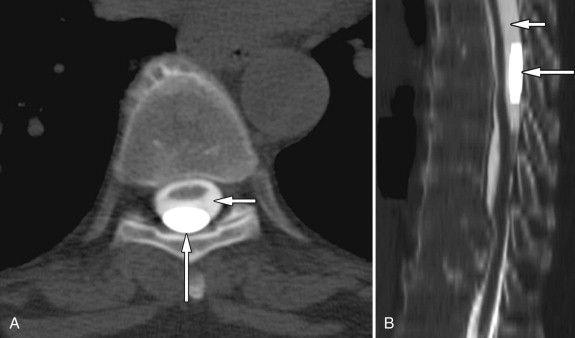
Lumbar arachnoiditis is an inflammatory condition of the arachnoid membrane that surrounds the spinal cord and its roots that eventually results in adhesions and clumping of nerve roots, thus the synonym chronic adhesive arachnoiditis . Quincke, in 1893, is credited with the initial description of arachnoiditis and with linking it to syphilis, gonorrhea, tuberculosis, and extension of infections from the middle ear. Currently, arachnoiditis is usually associated with substances that are injected into the subarachnoid space (myelographic contrast media, anesthetics, and steroids), infection, trauma, surgery (both intradural and extradural), and intrathecal hemorrhage. The oily contrast media iodophendylate (Pantopaque) has been estimated to cause radiographic arachnoiditis in approximately 70% of cases, whereas the early water-soluble agents caused arachnoiditis much less. The residua of Pantopaque myelography can still be seen today in routine imaging of elderly patients. Pantopaque has a high density and therefore is radiopaque on plain films ( Fig. 10-2 ) and computed tomography (CT) ( Fig. 10-3 ) . Pantopaque’s oily characteristics make it readily apparent on MR ( Fig. 10-4 ) . The clinical symptoms of arachnoiditis were seen in only about 1% of the total cases. Today’s water-based contrast agents have further decreased the incidence of both radiologic arachnoiditis (imaging findings of arachnoiditis without symptoms) and clinical arachnoiditis (imaging findings and symptoms of arachnoiditis).

Three membranes, the arachnoid, dura, and pia, cover and protect the spinal cord and nerve roots. The arachnoid membrane is very thin and fragile. It does not have innervation or vascularization and therefore it heals poorly. The pathogenesis of arachnoiditis is similar to the repair process of serous membranes in that there is a negligible inflammatory cellular exudate and a prominent fibrinous exudate. The fibrinous exudate covers the nerve roots and causes them to stick to each other and the thecal sac. During the repair phase, as arachnoiditis progresses, dense collagenous adhesions are formed by proliferating fibrocytes. Burton reviewed 100 patients with arachnoiditis and described the process beginning with a radiculitis or inflammation of the pia-arachnoid with associated hyperemia and swelling of the nerve roots. This was followed by fibroblast proliferation and collagen deposition that caused adherence of the nerve roots to each other and to the thecal sac. As arachnoiditis proceeded to its end stage, there was complete encapsulation of the nerve roots, which were atrophic and hypoxemic.
The patient with clinical arachnoiditis can demonstrate a myriad of symptoms, each of which taken alone could point to a different etiology. Back pain is one of the most frequent manifesting symptoms, which often begins unilaterally and may become bilateral later. However, certain bizarre symptoms can serve as clues to the proper diagnosis. The patient may describe a “burning sensation in the sacral region, gripping or clawing pain down the back of one or both legs not of sciatic distribution, tingling pain in the insteps, burning at the inner aspects of the knees, or tingling and pain in the feet. The symptoms often persist at rest and at night.” The patient may also have urinary urgency, frequency, and incontinence. There may be unexplained skin rashes and itching, loss of sensation below the affected area, or partial/complete paralysis of the lower extremities.
Potential complications of arachnoiditis are cauda equina syndrome and arachnoiditis ossificans. The cauda equina syndrome is often a late complication of arachnoiditis with symptoms of paresthesias, bowel and bladder abnormalities, and potentially paralysis. Arachnoiditis ossificans is calcification and/or ossification of the spinal meninges. A bony metaplasia of the arachnoid membrane occurs, which can compress the spinal nerves, resulting in severe, intractable pain, paraparesis, and bowel/bladder abnormalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree