Presentation and Presenting Images
( ▶ Fig. 16.1, ▶ Fig. 16.2, ▶ Fig. 16.3, ▶ Fig. 16.4, ▶ Fig. 16.5, ▶ Fig. 16.6)
An 83-year-old female with a history of left breast cancer (invasive ductal carcinoma) treated 15 years ago presents for screening mammography.
16.2 Key Images
( ▶ Fig. 16.7, ▶ Fig. 16.8, ▶ Fig. 16.9, ▶ Fig. 16.10, ▶ Fig. 16.11, ▶ Fig. 16.12)
16.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
16.2.2 Imaging Findings
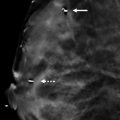
The patient was previously treated for invasive ductal carcinoma with a lumpectomy and radiation therapy. The imaging shows a postsurgical scar (circle) with associated architectural distortion, focal skin thickening, and surgical clips in the left breast upper outer quadrant at the 1 o’clock location, 6 cm from the nipple ( ▶ Fig. 16.7, ▶ Fig. 16.8, ▶ Fig. 16.10, and ▶ Fig. 16.11). There is no mammographic evidence of recurrent disease. The skin is marked with a scar marker (solid arrow in ▶ Fig. 16.7 and ▶ Fig. 16.10) and coarse vascular calcifications are noted by the broken arrow ( ▶ Fig. 16.7, ▶ Fig. 16.9, ▶ Fig. 16.10, and ▶ Fig. 16.12).
16.2.3 BI-RADS Classification and Action
Category 2: Benign
16.3 Differential Diagnosis
Postsurgical changes: The architectural changes at the postsurgical bed seen on the conventional two-dimensional (2D) mammogram or on tomosynthesis images are typical findings.
Recurrent breast cancer: There is no evidence of a mass, developing asymmetry, or suspicious calcifications in the postsurgical bed on either the conventional 2D mammogram or on tomosynthesis images.
Radial sclerosing lesion: The clinical history and postsurgical changes make a radial sclerosing lesion a very unlikely diagnosis. Without the clinical history, this could be a reasonable possible diagnosis.
16.3.1 Essential Facts
Postsurgical scars usually present as an area of architectural distortion with interspersed radiolucency, which represents entrapped fat. Typically scars contract over time. Tomosynthesis reduces overlap and demonstrates entrapped fat within postsurgical scars.
Radiologists can differentiate between postsurgical changes and recurrent malignancy by having a knowledge of characteristic imaging findings of both entities.
Postoperative changes usually decrease in size over time. Recurrence may be seen as a new mass, new calcifications, a new asymmetry, or a new area of architectural distortion in the lumpectomy site. Tomosynthesis can help to differentiate between a true mass lesion and a summation artifact resulting from overlapping breast tissue.
Findings that are equivocal or suspicious for recurrence warrant biopsy. If the findings are sonographically occult, biopsy may be performed using tomosynthesis guidance.
There are no suspicious findings. The calcifications present in this case are vascular. Tomosynthesis is helpful to demonstrate the orientation and location of the vascular calcifications. The location of the vascular calcifications is importation information if a biopsy is needed.
16.4 Management and Digital Breast Tomosynthesis Principles
Postsurgical masses, fluid collections, architectural distortions, scars, edema, skin thickening, and calcifications can mimic or mask recurrent malignancy. The three-dimensional imaging capability of tomosynthesis eliminates overlapping tissue providing imaging clarity of findings and the ability to accurately characterize lesions.
Performing conventional mammography and tomosynthesis imaging in a single compression allows for co-registration of these images, which allows for direct comparison. Any findings seen on the conventional study that are suspicious for new or recurrent malignancy can be either confirmed or excluded on tomosynthesis.
The inability to perform magnification of suspicious calcifications is a limitation of tomosynthesis, which is overcome by performing these views with conventional mammography.
16.5 Further Reading
[1] Krishnamurthy R, Whitman GJ, Stelling CB, Kushwaha AC. Mammographic findings after breast conservation therapy. Radiographics. 1999; 19(Spec No): S53‐S62, quiz S262–S263 PubMed

Fig. 16.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree