Presentation and Presenting Images
A 53-year-old female presents for screening mammography.
38.2 Key Images
38.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
38.2.2 Imaging Findings
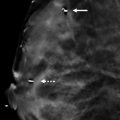
In the lower inner quadrant of the left breast, there is a subtle area of architectural distortion on the mediolateral oblique (MLO) view. ( ▶ Fig. 38.2). However, it is best seen in the tomosynthesis images ( ▶ Fig. 38.3 and ▶ Fig. 38.4). The right breast was normal (not shown).
38.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
38.4 Diagnostic Images
( ▶ Fig. 38.5, ▶ Fig. 38.6, ▶ Fig. 38.7, ▶ Fig. 38.8, ▶ Fig. 38.9, ▶ Fig. 38.10, ▶ Fig. 38.11)
38.4.1 Imaging Findings
The diagnostic imaging demonstrates persistent architectural distortion. However, it is best seen on the left mediolateral oblique (LMLO) spot-compression image ( ▶ Fig. 38.6). On this image, longer spicules that draw into a central region can be seen. A focally defined mass is not seen. The ultrasound reveals an irregular mixed hypoechoic mass with angular and indistinct margins located at 7 o’clock 4 cm from the nipple. This 2.1 × 1.3 × 1.3 cm mass has mild posterior acoustic shadowing ( ▶ Fig. 38.8 and ▶ Fig. 38.9). This mass was biopsied with ultrasound guidance. The postbiopsy mammogram demonstrates the biopsy marker clip (ribbon-shaped) in the expected location.
38.5 BI-RADS Classification and Action
Category 5: Highly suggestive of malignancy
38.6 Differential Diagnosis
Breast cancer (invasive lobular carcinoma): The architectural distortion was best seen on digital breast tomosynthesis (DBT). The additional mammographic images were supportive in the mediolateral oblique (MLO) spot-compression view. The ultrasound confirmed an irregular mass for which biopsy was strongly recommended.
Radial scar: Radial scars are known to be elusive on conventional mammographic imaging. The DBT images demonstrate architectural distortion. The diagnostic ultrasound reveals a larger mass than is typical for a radial scar. If an image-guided biopsy yielded a radial scar for this lesion, a surgical consult for excision would be warranted.
Normal breast tissue: The DBT images are too worrisome to stop and call this a summation artifact. Findings at DBT without a fully supportive diagnostic mammography evaluation warrant an ultrasound. The ultrasound does not demonstrate normal breast tissue.
38.7 Essential Facts
DBT allows the breast to be viewed in a three-dimensional format allowing for stacks of in-focus planes, or slices, to be viewed thus reducing the impact of superimposed breast tissue.
Some DBT–only findings can be effaced on conventional diagnostic imaging.
Architectural distortion and lesion margins are more apparent on DBT.
Architectural distortion is the most common DBT finding that is mammographically occult.
Invasive lobular carcinomas have a high frequency of being seen on DBT and of being occult to very subtle on full-field digital mammography (FFDM).
38.8 Management and Digital Breast Tomosynthesis Principles
Architectural distortion on DBT is the most frequently missed sign of breast cancer, and so result in false-negatives on screening mammography.
The incidence of malignancy for architectural distortion on DBT without a mammographic finding ranges from 21 to 36%.
Worrisome DBT findings that are not reproduced on conventional mammography warrant evaluation with ultrasound. These cases often are found to be cancers that would otherwise be overlooked mammographically.
Worrisome DBT findings without an ultrasound correlate warrant either a wire-localization or tomosynthesis-guided biopsy due to the high incidence of malignancy.
38.9 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Ray KM, Turner E, Sickles EA, Joe BN. Suspicious Findings at Digital Breast Tomosynthesis Occult to Conventional Digital Mammography: Imaging Features and Pathology Findings. Breast J. 2015; 21(5): 538‐542 PubMed

Fig. 38.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree