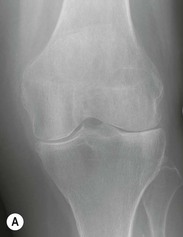
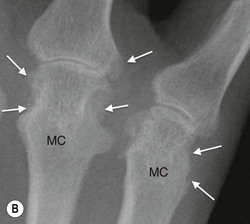
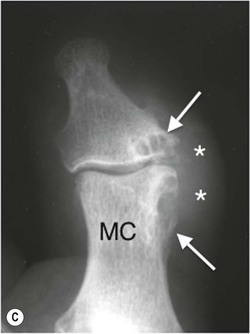
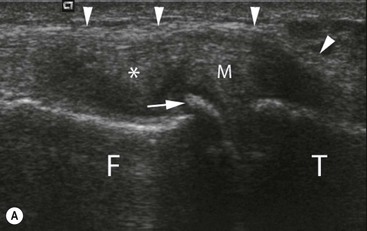
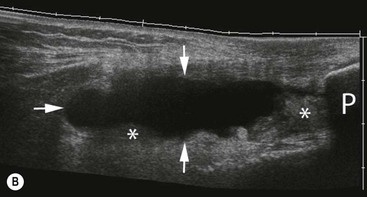
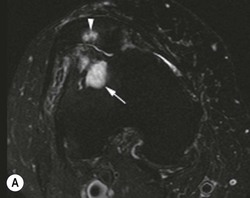
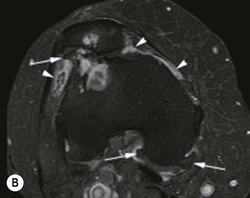
Andrew J. Grainger, Philip O’Connor The imaging of joint disease is complex, with the radiologist required to combine imaging findings and clinical information to accurately characterise arthritis. This chapter details the general principles of the plain radiographic assessment of arthritis and the key features of common arthritic conditions encountered. A systematic approach to the review of radiographs for arthritis is required. Important features to identify are: Finally, the distribution of joint disease provides important information when forming a differential diagnosis. Soft-tissue swelling is usually the earliest sign on CR of an inflammatory arthritis, representing synovial hypertrophy, soft-tissue oedema and joint effusion. When seen at the small joints the swelling has a symmetrical spindle shape about the joint. This pattern contrasts with soft-tissue swelling seen in gout, which tends to show a more irregular asymmetrical ‘lumpy’ appearance. Diffuse swelling of the soft-tissues of a digit is the characteristic finding in the dactylitis seen in hand involvement of the sero-negative inflammatory arthritides (Fig. 51-1). Radiographic soft-tissue abnormality around large joints tends to be limited to the detection of intra-articular effusion or synovitis. Loss of joint space as a result of cartilage destruction is a characteristic feature of many joint diseases. In inflammatory arthritis joint space loss is typically uniform, across the joint. In many joints this is helpful in distinguishing inflammatory arthritis from osteoarthritis (OA), which typically shows non-uniform joint space loss. However, in small joints, both forms of arthritis can show uniform joint space loss (Fig. 51-2). Preserved joint space in a joint otherwise showing evidence of significant arthropathic change is important and may help with the differential diagnosis. In particular gout and psoriatic arthropathy typically show joint space preservation until late in the disease. In severe arthritic change bony ankylosis may occur. This is most commonly seen in the sero-negative arthritides and in juvenile arthritis and represents end-stage disease. Periarticular osteopenia is a well-recognised feature of some arthritides but is difficult to reliably identify. It may be more obvious in cases of mono- or pauci-articular joint involvement, where other joints are visible for comparison. An overexposed radiograph can mimic periarticular osteopenia, as can generalised osteoporosis. Often it is easier to identify that there is no evidence of osteopenia, which in itself is a useful observation when forming a differential diagnosis. Sero-negative disease, OA and gout typically preserve or increase bone density (Fig. 51-3). Bone erosion is the hallmark of inflammatory arthritis. Erosions can be described by their relationship to the joint and can be categorised as central, marginal or juxta-articular. Marginal erosions occur at the edge of the joint line involving exposed bone between the edge of the articular cartilage and the joint capsule. They are a classical feature of rheumatoid arthritis (RA). Central erosions occur into bone normally covered by the articular cartilage. They are less common and are typical of inflammatory (erosive) OA. Juxta-articular erosions occur further away from the joint and are characteristic of gout. Rheumatoid erosions characteristically have no associated bone proliferation when untreated (Fig. 51-4A), whereas sero-negative erosions typically show proliferative bone formation in or around the erosion (Fig. 51-4B), a useful distinguishing feature. Gout erosions have characteristic overhanging sharply demarcated margins giving them a punched-out appearance (Fig. 51-4C). Enthesitis is a feature of the sero-negative arthritides. Entheses represent the bony attachment sites of ligaments, tendons or capsule. On radiographs the important bone changes that can be visualised in enthesitis are enthesophyte formation and erosion (Fig. 51-5). Enthesophytes develop at, or immediately adjacent to, the site of an enthesis. They generally have a coarse appearance, with both cortical and medullary bone involved. Joint malalignment is a feature of many arthropathic processes and results from a variety of causes, including tendon or ligament dysfunction and cartilage or bone loss. In most case this represents late changes of arthropathy though joint malalignment can be seen in several conditions without established bone or soft-tissue arthropathy. The best known of these is systemic lupus erythematosus (SLE) where subluxations and ulnar deviation of the fingers and toes are seen in patients without bone erosion or cartilage loss (Fig. 51-6). An important aid to diagnosis is the distribution of polyarthritic disease when involving the hand and wrist. Symmetrical proximal disease involving the carpal bones and metacarpophalangeal (MCP) joints is typical in rheumatoid arthritis. Distal disease of the interphalangeal joints is characteristic of sero-negative disease and osteoarthritis. Osteoarthritis (OA) is a ubiquitous disease and the most common articular disease. It affects the majority of the population at some time and is seen in other vertebrates. Unsurprisingly, considerable research continues to be centred on understanding the pathogenesis of this condition and developing new ways to treat it. However, it is becoming clear that the disease has a complex aetiology which includes genetic and mechanical factors.1 Fundamentally, the condition results from an alteration in the normal transmission of forces across a joint. This may occur due to an abnormality in the quality of the tissues at the joint, for instance ligamentous laxity as a result of a connective tissue disorder such as Ehlers–Danlos syndrome, or a change in the biomechanics at the joint such as might arise following trauma. However, it is recognised that there are strong influences on the aetiology of osteoarthritis that occur at a personal level such as genetics, race and ethnicity, diet, obesity, age and gender. It will be appreciated that some of these, such as obesity, will also act to alter joint biomechanics, but in general the understanding of how these and particularly genotypes affect the joint structures to bring about osteoarthritis remains unclear and is an important field for research. The term primary generalised osteoarthritis is used to refer to osteoarthritis occurring without an apparent underlying cause. Secondary osteoarthritis refers to cases where an underlying cause is identified. A wide range of secondary causes exists, but characteristically they tend to result in either altered structure in the constituent parts of the joint, altered loading across the joint or a combination of both (Table 51-1). Primary osteoarthritis is more common in women than men and has a strong genetic predisposition. It occurs in a typical distribution, characteristically affecting the hands, thumb bases, the hips, knees and first metatarsophalangeal joint in the foot. Many conditions, including trauma, may result in secondary osteoarthritis (Table 51-1). In many cases the cause is not identified. Only a single joint may be involved (for instance, when trauma has occurred), or in generalised conditions there may be multiple joint involvement. The radiological findings are identical to those of primary osteoarthritis. Typically, the changes of osteoarthritis seen at the joint represent a combination of destruction and repair, although the balance between these two processes varies. 1. Joint space loss: in common with other arthropathic processes, cartilage thinning is a feature of osteoarthritis, which is seen directly on MRI and identified on conventional radiographs as joint space narrowing. In osteoarthritis, cartilage loss occurs in a more asymmetric distribution across the joint, generally occurring in areas of stress (Figs. 51-2B and 51-7). This results in an uneven pattern of joint space loss, a useful distinguishing feature from other causes of arthropathy. 2. Osteophyte formation: osteophytes are an important diagnostic feature for osteoarthritis, representing the hypertrophic aspect of the disease. They represent new bone formation, generally at the joint margins, although subchondral osteophyte may develop within the joint line itself. They comprise trabeculated bone and may be seen on one or both sides of the joint (Fig. 51-7). 3. Subchondral bone change: the bone deep to the cartilage shows characteristic changes in osteoarthritis. Increased osteoblastic activity brings about sclerosis, while subchondral cysts and bony collapse may also be seen (Figs. 51-7 and 51-8). Cyst formation is thought to be the result of synovial fluid passing into the bone through the damaged cartilage. 4. Loose bodies: as fragments of cartilage and bone are shed into the joint, they may be resorbed but often persist as loose bodies (Fig. 51-8). They may become revascularised and actually grow in situ. This means it may not be possible to identify the source of a loose body. 5. Joint deformity and subluxation: the diseased joint will commonly show ligamentous laxity, allowing deformity (which may be contributed to by bony collapse and cartilage loss) and subluxation (Fig. 51-8). Further factors leading to deformity relate to reduced proprioception and reduced muscle tone in the elderly. It has long been recognised that pain experienced by the patient is poorly related to the changes of osteoarthritis seen in a joint on conventional radiographs. One patient may be severely incapacitated, despite only minor changes being evident on the radiograph, while another patient may have very little in the way of symptoms despite radiographically severe changes of osteoarthritis. This has led to investigation of osteoarthritis with more advanced imaging techniques, particularly ultrasound and MRI, in an effort to identify likely pain generators within the osteoarthritic joint. MRI and ultrasound will demonstrate other features such as synovitis, effusion and ligamentous change in addition to the features already described. MRI also demonstrates oedema-like marrow signal in the subchondral bone. Despite this new information, the source of pain in the joint remains unclear, although some evidence suggests that it may be associated with synovitis or bone marrow abnormalities. Osteoarthritis of the knee may show any or all the above features on conventional radiographs. As already noted, joint space loss is usually asymmetrical within a joint in osteoarthritis. The knee demonstrates this observation well as varying degrees of joint space loss are typically seen in the three compartments, often with relative preservation of a compartment despite severe joint space loss elsewhere.2 The most commonly seen pattern of osteoarthritis involves joint space loss in the medial compartment, often leading to varus deformity (Fig. 51-2B), but on occasion patellofemoral or lateral compartment disease will predominate (Fig. 51-9). Weight-bearing radiographs are more sensitive in identifying joint space loss in the medial and lateral compartments. Semi-flexed views also increase sensitivity to the detection of joint space loss compared to views obtained in extension3 (Fig. 51-9). ‘Skyline’ views of the patellofemoral joint are best suited to demonstrate the differential involvement of the medial and lateral facet. Again, joint space loss is typically asymmetrical across the joint. The most common pattern involves the superior aspect of the joint with superior migration of the femoral head and narrowing of the superior joint space. As disease progresses, sclerosis and cyst formation may be seen along with flattening of the femoral head (Fig. 51-7). Less commonly, medial joint space loss will predominate (Fig. 51-10). This pattern of joint space loss is more common in women than men. On occasions, central osteophyte forming within the hip joint will displace the femur laterally, giving apparent preservation of joint space. Osteophytes around the femoral head/neck margin will be appreciated as areas of sclerosis on the femoral neck as the anterior and posterior osteophyte overlies the femoral neck. A particular characteristic pattern of osseous hypertrophy is seen along the femoral neck, typically on the medial side, and is known as buttressing.4 It is appreciated as thickening of the medial femoral neck cortex (Fig. 51-10). Changes in the hands are characteristically associated with the development of firm nodules, which are generally the result of osteophyte formation or synovial hypertrophy. These are known as Heberden’s (distal interphalangeal joint) and Bouchard’s (proximal) nodes. The interphalangeal joints (proximal and distal) are typically involved in primary osteoarthritis. However, the pattern of involvement is usually asymmetrical, with different joints on the two hands affected. Metacarpophalangeal joint disease is less frequently seen. At the wrists the disease usually affects the thumb base, involving the thumb carpometacarpal joint and/or the scaphotrapezio-trapezoid (STT) joint (Fig. 51-8). Degenerative changes, representing osteoarthritis of the spine, are also discussed elsewhere. This most commonly occurs in the cervical and lower lumbar spine where degeneration in the intervertebral disc is seen as loss of disc height. Large osteophytes may be seen arising from the vertebral bodies, along with sclerotic change in the vertebral endplates. On occasion, osteophytes will bridge the intervertebral disc space. Typical osteoarthritic change may also be seen in the facet joints where osseous hypertrophy may contribute to spinal stenosis. Abnormalities of vertebral alignment may also occur as a result of ligamentous laxity and degenerative changes in the disc and facet joints; typically, anterior displacement of the vertebra superior to a degenerative disc is seen with respect to its more caudal neighbour. This can be distinguished from the spondylolisthesis seen in association with pars defects (spondylolysis) because the posterior elements of the vertebral body will also slip forward along with the vertebral bodies, as there is no separation of the anterior and posterior spinal elements. For the most part the advanced imaging of OA remains the preserve of the research environment. However, given the ubiquitous nature of the disease it is not uncommon to identify features of OA on studies undertaken for other purposes or suspected diagnoses. In recent years it had become recognised that OA is not just a disease of cartilage but affects multiple components of the joint. These include the synovium, ligaments, subchondral bone, articular fibrocartilage (for instance, the menisci in the knee and TFC in the wrist) and the periarticular tendons. Both MRI and ultrasound readily identify synovitis in OA and this can be marked in osteoarthritis (Figs. 51-11 and 51-12). Osteophytes are also demonstrated by both techniques, ultrasound having been shown to be more sensitive to their detection in the wrist than conventional radiography.5 While ultrasound is unable to demonstrate the changes in the subchondral bone, MRI will show cystic change and sclerosis but in addition may show oedema-like signal (Fig. 51-12). Research studies suggest this is not due to true oedema within the bone marrow, and thus the term ‘bone marrow lesion’ is increasingly used in this context. Erosive osteoarthritis represents a subset of osteoarthritis with more inflammatory and destructive changes. It is usually seen as a polyarthritis classically involving the distal and proximal interphalangeal joints in the hands, although large joint involvement has been described. It is more common in women and has been shown to have a worse outcome than non-erosive OA.6 While clinical clues may exist as to the inflammatory pattern of disease, the distinction from non-erosive OA is made on the radiographic appearances and the demonstration of erosions. Controversy still exists as to whether this condition represents a separate subgroup of patients with osteoarthritis or represents one end of a spectrum of increasing inflammatory change in osteoarthritis. The pattern of erosion seen in erosive osteoarthritis is characteristically described as being central in location (occurring in the subchondral bone) and gives rise to the characteristic ‘seagull wing’ pattern of erosion7 (Fig. 51-13). Marginal erosions may also be seen but appear to be much less common. Reparative change may occur and can lead to bony ankylosis, not a typical feature of non-erosive OA.8 The inflammatory arthritides are characterised by multiple joint involvement with inflammatory change either within the joint, the enthesis or periarticular soft tissues. The management of inflammatory arthritis has changed dramatically in recent years with the advent of powerful biological therapies that, if instigated early, can induce disease remission and prevent the severe joint destruction previously seen. This has led to a greater emphasis on early diagnosis. While CR shows characteristic features of inflammatory arthritis, these represent late findings in the disease process and the use of advanced imaging techniques such as magnetic resonance or ultrasound is becoming more common. These allow early diagnosis and treatment before irreversible joint damage has occurred. Nevertheless, radiography continues to play an important role in the diagnosis and characterisation of inflammatory arthritis and usually forms the initial imaging study. Rheumatoid arthritis (RA) is a chronic multisystem autoimmune disorder of unknown aetiology. In Europe it has an incidence of approximately 1%. It is more common in women and is characterised initially by a polyarticular symmetrical synovitis.9 The later stages of the disease involve joint destruction as a result of bone erosion and cartilage loss. Synovitis is considered to be a strong predictor of bone erosion.10,11 The hands and wrists are most commonly involved although any synovial joint in the body can be affected. Soft-tissue involvement is seen with the development of tenosynovitis and rheumatoid nodules, which can precede joint changes. The clinical, and consequently radiological, picture of RA has changed over recent years due to dramatic advances in the way RA is treated. The use of powerful biological agents early in the disease process to arrest joint damage and induce disease remission has resulted in a change in the radiographic assessment of RA, with the detection of early or subtle change increasingly important.12 The classical plain film appearance of RA is of a symmetrical polyarthritis of the hands and wrists with a proximal distribution typically involving the carpal, MCP and proximal interphalangeal (PIP) joints. Characteristically the distal interphalangeal (DIP) joints are spared, providing an important distinguishing feature from OA and psoriatic arthritis. The earliest plain film changes are soft-tissue swelling and periarticular osteopenia. At the MCP and PIP joints the soft-tissue swelling is appreciated as spindle-shaped thickening of the soft tissues developing symmetrically about the joint. Periarticular osteopenia can be a difficult radiographic sign to evaluate, particularly when there is symmetrical polyarticular involvement. Joint space loss in RA is usually panarticular, with diffuse joint space loss. Marginal erosions are characteristic of rheumatoid arthritis, and are seen most frequently in the joints of the hands, wrists and feet, erosions being more commonly seen in small joints than large joints. The earliest sites of erosion are typically the radial aspect of the index and middle metacarpal heads and the ulnar aspect of the wrist (Fig. 51-14). Cortical bone loss is first seen as subtle breaks in the bone giving the cortex a ‘dot-dash’ appearance; subsequently, frank bone erosion is seen (Fig. 51-4A). A form of the disease featuring large cystic areas, typically occurring in active men, has been termed robust rheumatoid and is thought to occur as a result of continued physical activity despite active inflammatory arthropathy.13 Ankylosis may occur in the later stages of the disease. Typically this involves the wrist with intercarpal and carpometacarpal fusions. Tendon and ligamentous dysfunction along with bone erosion results in deformity and malalignment in the later stages of the disease. Ulnar deviation of the fingers and the radial deviation of the wrist giving a ‘zigzag’ deformity to the hand is also typical for RA.14 In the fingers, deformity involving flexion of the PIP joint and extension of the DIP joint (Boutonnière) (Fig. 51-15) or flexion of the DIP joint and extension of the PIP joint (swan neck) are common. Subcutaneous rheumatoid nodules over the extensor surfaces of joints and in tendons are a common feature of RA seen in around 20% of patients. Preservation of bone density may be seen with successfully treated rheumatoid arthritis. In cases where irreversible joint damage has occurred, secondary osteoarthritic change can develop. It is important to recognise this when present, as it can lead to persisting symptoms and inappropriate continuation of biological therapy. The proximal distribution of these secondary osteoarthritic changes and the superimposition of proliferative bone changes on rheumatoid erosions are the key observations in making this diagnosis (Fig. 51-16).
Arthritis
Imaging of Joint Disease
Plain Radiographic Interpretation; General Principles
Soft-Tissue Swelling
Alteration in Joint Space
Bone Changes
Osteopenia.
Erosion.
Entheseal Disease.
Bone Alignment
Distribution of Joint Involvement
Osteoarthritis
Primary Osteoarthritis
Secondary Osteoarthritis
Radiographic Findings
Radiographic Changes at Specific Joints
Knee
Hip

Hands and Wrists
Spine
Advanced Imaging
Erosive (Inflammatory) Osteoarthritis
The Inflammatory Arthritides
Rheumatoid Arthritis
Radiographic Features
Radiographs in Treated Inflammatory Disease

Arthritis
Chapter 51
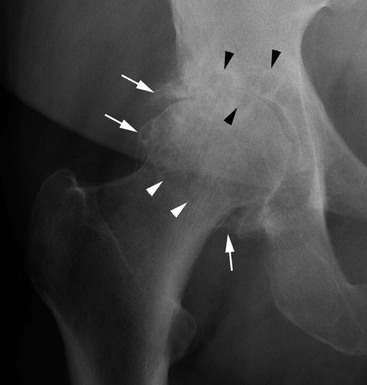
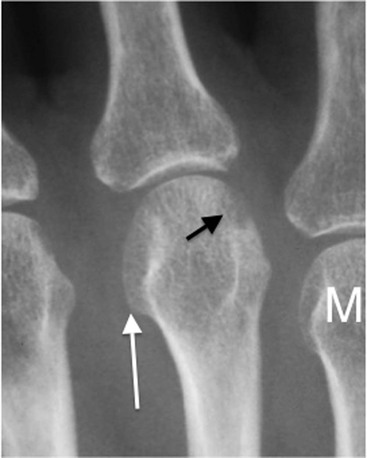
FIGURE 51-10 Severe osteoarthritis of the hip. AP radiograph: In this case joint space loss is in a less common medial distribution (black arrowheads). The study also shows osseous hypertrophy along the medial neck of the femur (buttressing) (white arrowheads). Note also the marginal osteophytes which can also be seen projected over the femoral neck (cf. Fig. 51-7).