Arthritis
Clyde A. Helms
Osteoarthritis
Osteoarthritis, or degenerative joint disease (DJD), is the most common arthritide. It is believed to be caused by trauma—either overt or as an accumulation of microtrauma over years, although there is also a hereditary form called primary osteoarthritis that occurs primarily in middle-aged women. The hallmarks of DJD are joint space narrowing, sclerosis, and osteophytosis (Table 43.1 and Fig. 43.1). If all three of these findings are not present on the radiograph, another diagnosis should be considered. Joint space narrowing is the least specific finding of the three; yet, it is virtually always present in DJD. Unfortunately, joint space narrowing is also seen in almost every other joint abnormality.
Sclerosis should be present in varying amounts in all cases of DJD unless severe osteoporosis is present. Osteoporosis will cause the sclerosis to be diminished. For instance, in long-standing rheumatoid arthritis in which the cartilage has been destroyed, DJD often occurs with very little sclerosis. Osteophytosis will be diminished in the setting of osteoporosis also. Otherwise, sclerosis and osteophytosis should be prominent in DJD.
The only disorder that will cause osteophytes without sclerosis or joint space narrowing is diffuse idiopathic skeletal hyperostosis (1). This is a common bone-forming disorder that at first glance resembles DJD, except that there is no joint space narrowing (or disc space narrowing in the spine) and there is no sclerosis (Fig. 43.2). Diffuse idiopathic skeletal hyperostosis is not believed to be caused by trauma or stress as is DJD and is not painful or disabling as DJD can be. Millions of dollars per year are awarded to federal employees at retirement, representing “disability” payments for supposed DJD acquired during their employment, when in fact, these retirees have diffuse idiopathic skeletal hyperostosis and have been misdiagnosed.
Osteoarthritis is divided into two types: primary and secondary. Secondary osteoarthritis is what radiologists refer to when speaking of DJD. It is, as mentioned, secondary to trauma of some sort. It can occur in any joint in the body but is particularly common in the hands, knees, hips, and spine.
Primary osteoarthritis is a familial arthritis that affects middle-aged women almost exclusively and is seen only in the hands. It affects the distal interphalangeal joints, the proximal interphalangeal joints, and the base of the thumb in a bilaterally symmetrical fashion (Fig. 43.3). If it is not bilaterally symmetrical, the diagnosis of primary osteoarthritis should be questioned.
A type of primary osteoarthritis that can be very painful and debilitating is erosive osteoarthritis. It has the identical distribution mentioned for primary osteoarthritis but is associated with osteoporosis of the hands, as well as erosions. It is uncommon, and radiologists generally see little of this disorder. It is also called Kellgren arthritis.
There are a few exceptions to the classic triad of findings seen in DJD (sclerosis, narrowing, and osteophytes). Several joints also exhibit erosions as a manifestation of DJD: the temporomandibular joint, the acromioclavicular joint, the sacroiliac (SI) joints, and the symphysis pubis (Table 43.2). When erosions are seen in one of these joints, DJD must be considered or inappropriate treatment may be instituted (Fig. 43.4).
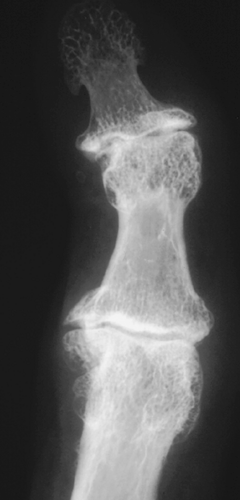
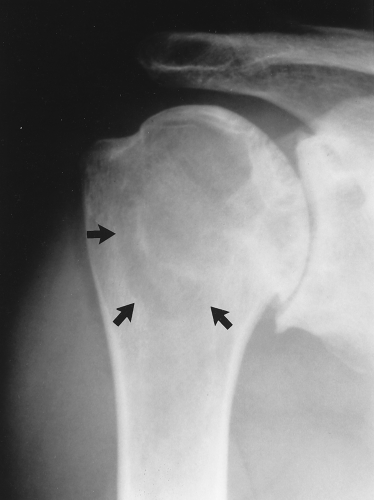
A subchondral cyst, or geode (taken from the geologic term used when a volcanic rock has a gas pocket that leaves a large cavity in the rock), is often found in joints affected with DJD. Geodes are cystic formations that occur around joints in various disorders (including, in addition to DJD, rheumatoid arthritis, calcium pyrophosphate dihydrate crystal deposition disease, and avascular necrosis (AVN) (Table 43.3) (2). Presumably, one method of geode formation is that synovial fluid is forced into the subchondral bone, causing a cystic collection of joint fluid. Another etiology is following a bone contusion in which the contused bone forms a cyst. They rarely cause problems by themselves but are often misdiagnosed as something more sinister (Fig. 43.5).
Table 43.1 Hallmarks of Degenerative Joint Disease | |||
|---|---|---|---|
|
Rheumatoid Arthritis
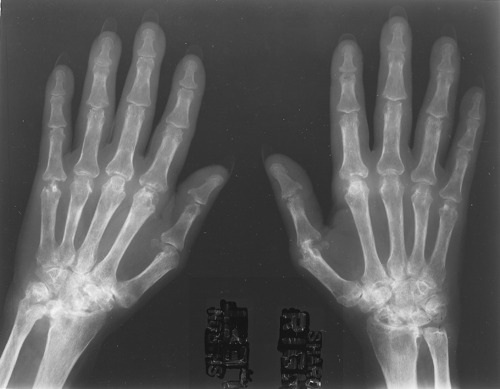
Rheumatoid arthritis is a connective tissue disorder of unknown etiology that can affect any synovial joint in the body. The radiographic hallmarks are soft tissue swelling, osteoporosis, joint space narrowing, and marginal erosions. In the hands, it is classically a proximal process that is bilaterally symmetrical (Table 43.4 and Fig. 43.6). There are so many exceptions to these rules, however, that I have come to regard them as no better than 80% accurate. Rheumatoid arthritis has a large variety of appearances, and from its radiographic appearance alone, it can be very difficult to diagnose with any degree of assurance.
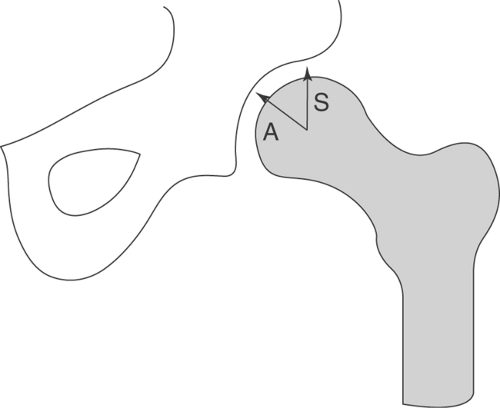
Rheumatoid arthritis in large joints is fairly characteristic in that it causes marked joint space narrowing and is associated with osteoporosis. Erosions might or might not be present and tend to be marginal, that is, away from the weight-bearing portion of the joint. In the hip, the femoral head tends to migrate axially, whereas in osteoarthritis, it tends to migrate superolaterally (Figs. 43.7, 43.8). In the shoulder, the humeral head tends to be “high-riding” (Fig. 43.9). Other things to think of when confronted with a high-riding shoulder are a torn rotator cuff and CPPD (Table 43.5).
Table 43.2 Joints That Have Erosions As A Feature of Degenerative Joint Disease | ||||
|---|---|---|---|---|
|
Table 43.3 Diseases in Which Geodes Are Found | ||||
|---|---|---|---|---|
|
Table 43.4 Hallmarks of Rheumatoid Arthritis | ||||||
|---|---|---|---|---|---|---|
|
Table 43.5 Causes of High-Riding Shoulder | |||
|---|---|---|---|
|
When rheumatoid arthritis is long-standing, it is not unusual for secondary DJD to superimpose itself on the findings one would expect with rheumatoid arthritis. This picture of DJD differs somewhat from that usually seen, in that the sclerosis and the osteophytes are considerably diminished in severity as compared with the joint space narrowing (Fig. 43.10).
Hla-B27 Spondyloarthropathies
A group of diseases that was formerly known as rheumatoid variants is now known as the seronegative, human leukocyte antigen B27 (HLA-B27)-positive spondyloarthropathies. These disorders are all linked to the HLA-B27 histocompatibility antigen. Included in this group of diseases are ankylosing spondylitis, inflammatory bowel disease, psoriatic arthritis, and Reiter syndrome (also called reactive arthritis). They are characterized by bony ankylosis, proliferative new-bone formation, and predominantly axial (spinal) involvement.
One of the more characteristic findings in these disorders is that of syndesmophytes in the spine. A syndesmophyte is a paravertebral ossification that resembles an osteophyte, except that it runs vertically, whereas an osteophyte has its orientation in a horizontal axis. Sometimes it can be difficult to decide whether a particular paravertebral ossification is an osteophyte or a syndesmophyte based on its orientation alone (Fig. 43.11).
Bridging osteophytes and large syndesmophytes can have a similar appearance, with both having an orientation halfway between vertical and horizontal. How should one evaluate those cases? Look at the other vertebral bodies and use the ossifications on them to determine whether they are osteophytes or syndesmophytes. If no other level is involved, one might not be able to tell one from the other.
Bridging osteophytes and large syndesmophytes can have a similar appearance, with both having an orientation halfway between vertical and horizontal. How should one evaluate those cases? Look at the other vertebral bodies and use the ossifications on them to determine whether they are osteophytes or syndesmophytes. If no other level is involved, one might not be able to tell one from the other.
Syndesmophytes are classified as to whether they are marginal and symmetrical or nonmarginal and asymmetrical. A marginal syndesmophyte has its origin at the edge or margin of a vertebral body and extends to the margin of the adjacent vertebral body. They are invariably bilaterally symmetrical as viewed on an AP spine film. Ankylosing spondylitis classically has marginal, symmetrical syndesmophytes (Fig. 43.12).
Inflammatory bowel disease has an identical appearance when the spine is involved. Nonmarginal, asymmetrical syndesmophytes are generally large and bulky. They emanate from the vertebral body away from the endplate or margin and are unilateral or asymmetrical as viewed on an AP spine film (Figs. 43.11, 43.13). Psoriatic arthritis and Reiter syndrome classically have this type of syndesmophyte.
Inflammatory bowel disease has an identical appearance when the spine is involved. Nonmarginal, asymmetrical syndesmophytes are generally large and bulky. They emanate from the vertebral body away from the endplate or margin and are unilateral or asymmetrical as viewed on an AP spine film (Figs. 43.11, 43.13). Psoriatic arthritis and Reiter syndrome classically have this type of syndesmophyte.
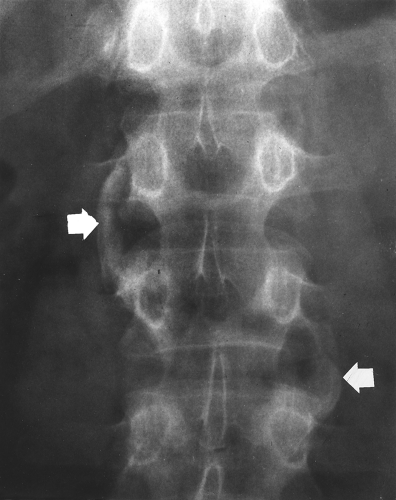 Figure 43.13. Syndesmophytes in Psoriatic Arthritis. Large, bulky, nonmarginal, asymmetrical syndesmophytes (arrows) are seen in this patient with psoriatic arthritis. |
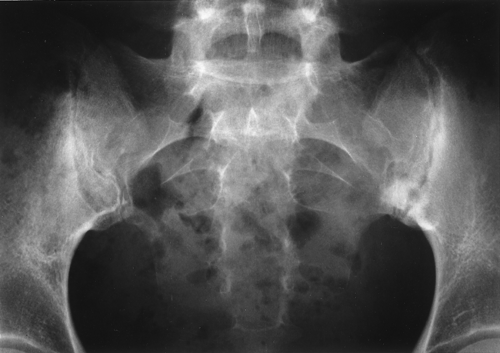
Involvement of the SI joints is common in the HLA-B27 spondyloarthropathies. The patterns of involvement, like the patterns of involvement of the spine, are somewhat typical for each disorder. Ankylosing spondylitis and inflammatory bowel disease typically cause bilaterally symmetrical SI joint disease, which is initially erosive in nature and progresses to sclerosis and fusion (Figs. 43.14, 43.15). It is extremely unusual to have asymmetrical or unilateral SI joint disease in these two disorders.
Reiter syndrome and psoriatic arthritis can exhibit unilateral or bilateral SI joint involvement. It seems that it is bilateral about 50% of the time. It is often asymmetrical when it is bilateral, but exact symmetry can be difficult to assess; therefore, when it is definitely bilateral and not clearly asymmetrical, consider the SI joints to be in the bilateral symmetrical category. This means that if there is bilateral, symmetrical SI joint disease, it could be caused by any of the four HLA-B27 spondyloarthropathies. If there is unilateral (or clearly asymmetrical) SI joint involvement, one can exclude ankylosing spondylitis and inflammatory bowel disease and consider Reiter syndrome or psoriatic disease. In this latter example, one would also have to consider infection and DJD (remember that DJD can cause erosions in the SI joints). Although seen less commonly, gout can also affect the SI joints unilaterally (Table 43.6 and Figs. 43.4, 43.16).
Table 43.6 Causes of Sacroiliac Joint Disease | |||||||
|---|---|---|---|---|---|---|---|
|
CT can be very helpful in examining the SI joints and is considered by many to be the diagnostic procedure of choice because of the unobstructed view of the entire joint (Fig. 43.17).
Large joint involvement with the HLA-B27 spondyloarthropathies is uncommon (except for ankylosing spondylitis), but when it does occur, the arthropathy will resemble rheumatoid arthritis (Fig. 43.18). The hips are involved in up to 50% of the patients with ankylosing spondylitis.
Small joint involvement, specifically in the hands and the feet, is not common in ankylosing spondylitis and inflammatory bowel disease. Psoriasis causes a distinctive arthropathy that is characterized by its distal predominance, proliferative erosions, soft tissue swelling, and periostitis. Proliferative erosions are different from the clean-cut, sharply marginated erosions seen in all other erosive arthritides in that they have fuzzy margins with wisps of periostitis emanating from them (Fig. 43.19A). The severe forms are often associated with bony ankylosis across joints (Fig. 43.19B) and arthritis mutilans deformities. A fairly common finding is a calcaneal heel spur that has fuzzy margins as opposed to the well-corticated heel spur seen in DJD or post-trauma (Fig. 43.20).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree