Arthritis
Inclusionary criteria
Systemic arthritis
Arthritis in at least one joint
2 weeks’ fever consecutive at least 3 days
Rash, generalized lymphadenopathy, hepatomegaly/splenomegaly, or serositis
Oligoarthritis (persistent)
Arthritis of 1–4 joints during the first 6 months
Never involves more than 4 joints
Oligoarthritis (extended)
Arthritis of 1–4 joints during the first 6 months
Eventually affects at least 5 joints
Polyarthritis (RF negative)
Arthritis of more than 5 joints during the first 6 months
RF test negative
Polyarthritis (RF positive)
Arthritis of more than 5 joints during the first 6 months
RF test positive (at least twice, during the first 6 months)
Psoriatic arthritis
Arthritis and psoriasis
Or arthritis and at least 2 in first-degree relative:
Dactylitis, nail pitting, psoriasis
Enthesitis-related arthritis
Arthritis and enthesitis, with
Sacroiliac joint tenderness and/or lumbosacral pain
HLA-B27 antigen
Male over 6-year-old
Acute anterior uveitis
First-degree relative with ankylosing spondylitis, enthesitis-related arthritis, sacroiliitis with inflammatory bowel disease, Reiter syndrome, or acute anterior uveitis
Undifferentiated arthritis
Arthritis that fulfills two or more of these categories or that fails to fall into one of these categories
The most common JIA subtype, “oligoarticular,” affects no more than four joints during the first 6 months of presentation; it usually affects the knees and/or ankles, as well as the wrists and elbows, of girls less than 6 years old [1]. Up to 30 % of these children also have iridocyclitis. “Polyarticular” arthritis presents with involvement of at least five joints within 6 months of presentation and is usually symmetric, involving the wrists, hands, and feet. Results of serologic testing allow further categorization: RF-positive cases typically occur in adolescent girls, and like rheumatoid arthritis in adults, the disease affects the small joints of the hands. RF-negative cases, which have a broad variety of manifestations, occur throughout childhood.
Arthritis is categorized as systemic if at least one joint is affected and if accompanied or recently preceded by at least 2 weeks of fever (consecutive for at least 3 days), a transitory rash, hepatomegaly, splenomegaly, lymphadenopathy, or serositis. Classic polyarticular and symmetric symptoms generally occur late in the course of disease. Systemic JIA may be life-threatening in a small subset of patients who develop pancytopenia, disseminated intravascular coagulation, and multiorgan failure (“macrophage activation syndrome”).
Psoriatic arthritis and enthesitis-related arthritis (ERA) subtypes are based on the presence of dactylitis, psoriasis, symptoms related to the sacroiliac joints or lower back, presence of human leukocyte antigen (HLA)-B27, and additional findings. Juvenile psoriatic arthritis affects large or small joints, and joint findings may precede development of skin abnormalities. ERA (formerly termed juvenile spondyloarthritis) is unusual among the subtypes of JIA in that the hip is often affected. This disease tends to affect sites of tendinous and ligamentous insertion at the pelvis, knee, and calcaneus. Axial involvement is rare in children under 10 years of age, although the spine and sacroiliac joints may be affected in older children (see following section for further discussion of Sect. 1.1). Undifferentiated JIA encompasses cases with none of these features or with features that are present in at least two different subtypes.
Disease usually becomes inactive with anti-inflammatory medication. However, in many patients, disease progresses unabated, regardless of treatment. Between 28 and 55 % of patients develop cartilage or bone erosions, often leading to joint irregularity, within 7 years of initial diagnosis [4]. Ankylosis, most common in the carpal and tarsal bones as well as the cervical spine, may develop within 3–5 years of disease onset.
Imaging (Table 20.1)
General Considerations. Radiographs are often initially normal, but in the early phase there may be nonspecific consequences of hypervascularity and inflammation, including joint effusion, soft tissue swelling, epiphyseal widening, and periarticular osteopenia. This is partly because in the pediatric skeleton thick cartilage protects bone, so erosive change is encountered only with advanced disease. In addition, the synovial hypertrophy and cartilaginous changes typical of early JIA are radiographically occult. However, radiographs performed early in the course of disease do both allow exclusion of other causes of pain and establish a baseline. US and MRI are able to demonstrate early findings of synovial hypertrophy and hyperemia.
During the intermediate phase, cartilage destruction results in joint space narrowing, cortical erosions, and epiphyseal overgrowth; these findings are demonstrable on both radiographs and MRI and to a lesser extent US. Finally, ankylosis, muscle atrophy, growth disturbance, angular deformity at the joints, and contractures may be seen with late disease.
During active disease, clinical examination generally provides adequate assessment of articular synovitis. US and MRI are, however, useful for early staging and for monitoring response to therapy. Indeed, techniques such as T2 mapping may demonstrate progressive cartilage deterioration even when clinical findings are stable [5]. Numerous attempts have been made to develop radiographic scoring systems, none of which have been widely accepted [6, 7]. Radiographs therefore do not play an important role in monitoring progression, but they are important for evaluating deformities and growth abnormalities.
Radiographic Findings.
Radiographs may demonstrate joint effusions early in JIA, especially at the knee (Fig. 20.1) The small joints of the hands and feet may show fusiform soft tissue swelling, especially common with psoriatic arthritis. US and MRI are more sensitive for evaluation of the small joints than are radiographs.


Fig. 20.1
Knee effusion in a 3-year-old boy with polyarticular juvenile idiopathic arthritis (JIA), symptomatic since age 1 year. There are also growth arrest lines and juxta-articular osteopenia. Findings were bilaterally symmetric (Same patient as Fig. 20.4) (Image copyright Shriners Hospital for Children Northern California)
Osteopenia is another relatively early finding (Fig. 20.2). In the acute setting, this results from juxta-articular hyperemia and resultant trabecular resorption, whereas in chronic disease it is more generalized and results from steroid use and disuse atrophy.


Fig. 20.2
Erosions and osteopenia in a 10-year-old girl with seronegative polyarticular JIA. In addition to the carpal erosions and juxta-articular demineralization/soft tissue swelling, there are flexion deformities at the third through fifth proximal interphalangeal (PIP) joints (Image copyright Shriners Hospital for Children Northern California)
Periostitis occurs at any stage of disease and in any long bone but is most common in the short tubular bones of the hands and feet (Fig. 20.3). This usually develops at para-articular locations, due to inflammation of the joint capsule and tendinous insertions. Bones may enlarge and become square as a result (especially common with psoriatic arthritis) (Fig. 20.4).
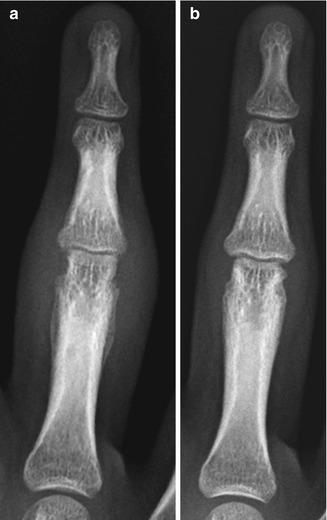

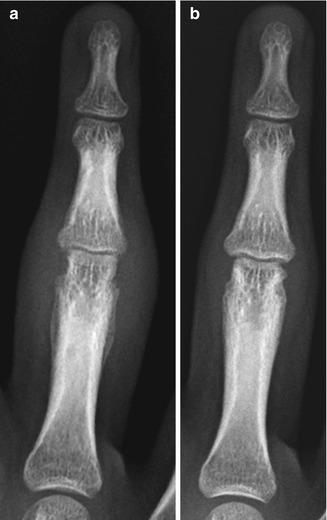
Fig. 20.3
Periostitis in a 15-year-old girl with psoriatic JIA. (a) Marked soft tissue swelling, moderate joint space narrowing, and erosions at the PIP joint of the right fourth digit. Periosteal reaction along the proximal phalanx. (b) Eight months later, after methotrexate therapy, findings have improved (Images copyright Shriners Hospital for Children Northern California)

Fig. 20.4
Squaring of phalanges in a 3-year-old boy with polyarticular JIA. Findings are most striking in the proximal and middle phalanges, where periostitis causes thickening of phalanges. Diffuse soft tissue swelling (Same patient as Fig. 20.1) (Image copyright Shriners Hospital for Children Northern California)
Erosions are evident relatively late, after thick protective cartilage has been destroyed by prolonged synovial proliferation (Fig. 20.5). Although erosions may occur anywhere along the articular surface, they are most common at locations where there is less cartilage—insertion sites of intraosseous ligaments and synovial reflections. Radiographs show decreased joint space due to cartilage loss before erosions become apparent, but they are relatively insensitive for showing trabecular bone loss [8]. In patients with systemic JIA, joint space narrowing and erosions may be found relatively early in the course of disease [9].
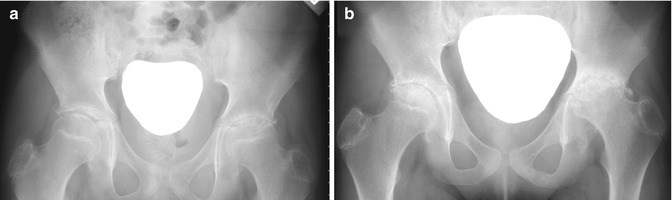
Fig. 20.5
Disease progression in a teenage girl with systemic JIA. (a) At age 15 years, there are small femoral head erosions and uniform joint space narrowing on the left, whereas the right is almost normal. (b) Two years later, the joint space on the left is barely evident, and there are more acetabular and femoral head erosions as well as sclerosis. The right femoral head is developing erosions (Images copyright Shriners Hospital for Children Northern California)
Growth disturbance, a relatively late finding, is both more common and more severe in children with early onset of disease. It may be generalized, resulting from chronic disease and long-term steroid use. Alternatively, localized growth disturbance may result from periarticular inflammation and localized hyperemia, which lead to early growth acceleration and subsequent epiphyseal enlargement as well as early physeal closure and accelerated maturation. This accounts for the typical appearance at the knee (Figs. 20.6 and 20.7): ballooned epiphyses, wide intercondylar notch, and squared inferior patella, which may in turn lead to subluxation. Although hyperemia leads to initial growth acceleration and longitudinal overgrowth, premature bone maturation and physeal fusion/epiphyseal destruction may eventually cause decreased limb length. A similar process takes place in the carpal and tarsal bones, which may demonstrate premature ossification and then osseous coalition (Fig. 20.8). Growth disturbance is also common in the mandible (see discussion below).


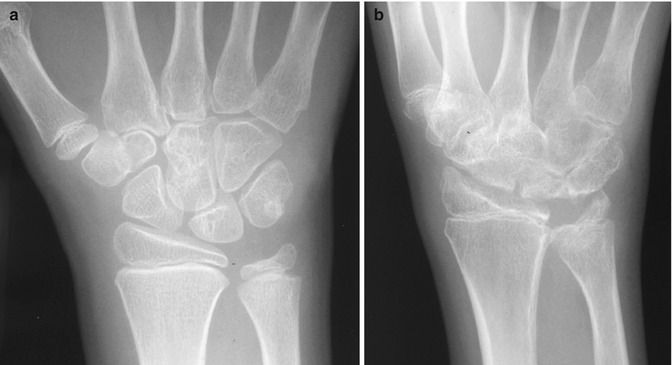

Fig. 20.6
Knee deformity in chronic JIA. Epiphyseal squaring, femoral notch enlargement, joint space narrowing, and subchondral cysts are typical of long-standing disease. Dislocated patella (Image copyright Shriners Hospital for Children Northern California)

Fig. 20.7
Knee deformity and subluxation in an 18-year-old female with JIA. (a) Epiphyseal enlargement and asymmetric growth, joint space narrowing, subchondral cysts, and valgus deformity are characteristic of long-standing disease. (b) Squaring of the patella and subluxation at the tibiofemoral joint. Findings were bilaterally symmetric (Same patient as Fig. 20.17) (Images copyright Shriners Hospital for Children Northern California)
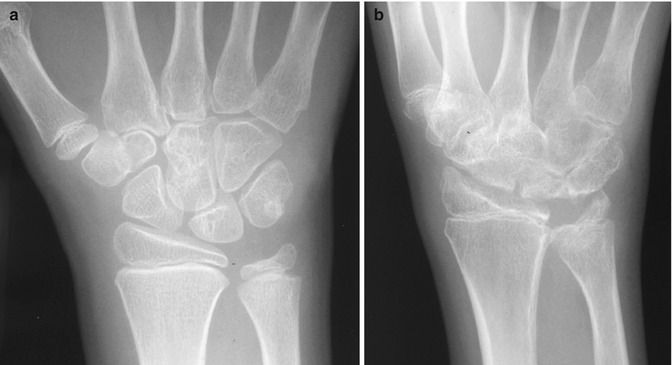
Fig. 20.8
Progression of carpal pathology in a girl with polyarticular JIA. (a) Slight intercarpal joint space narrowing at age 9 years. (b) At age 15 years, there is marked intercarpal narrowing, along with erosions and developing ankylosis. Note erosions and deformity of the distal radius and ulna. The gap at the radiocarpal articulation is likely due to hypertrophic pannus (Images copyright Shriners Hospital for Children Northern California)
Ankylosis (Fig. 20.9), erosions, synovial hypertrophy, effusions, and muscle imbalance may cause abnormal stress at the joints and lead to flexion and extension deformities as well as joint subluxation and dislocation (see subsequent paragraph). The knee may develop varus or valgus deformity, in part due to asymmetric epiphyseal overgrowth (see Fig. 20.7). This may contribute to deformity at the hip, including enlargement of the femoral head, acetabular protrusion, coxa vara, and hip subluxation. A similar process may occur in the upper extremities, with asymmetric epiphyseal enlargement causing deformity at the elbow and shoulder (Figs. 20.10 and 20.11).
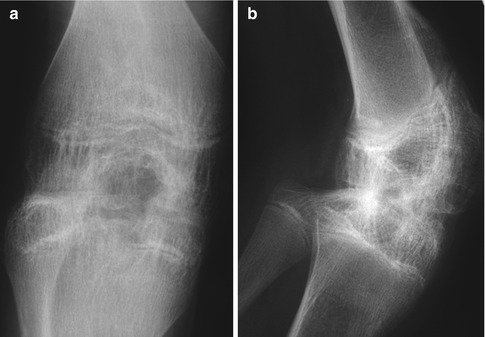
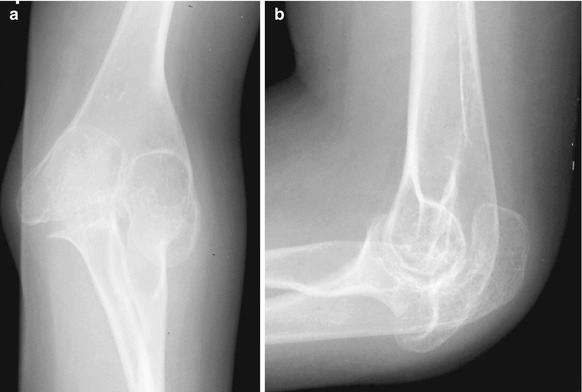

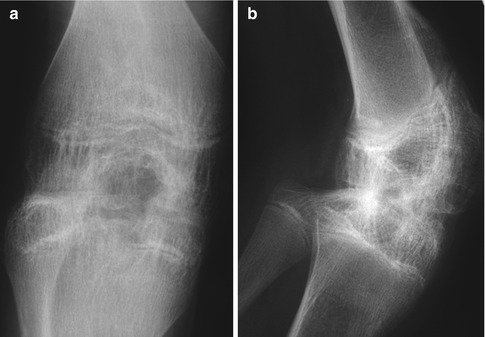
Fig. 20.9
Ankylosis at the knee in late-stage polyarticular JIA. (a, b) Growth plates are still open, and the femoral notch is enlarged (Images copyright Shriners Hospital for Children Northern California)
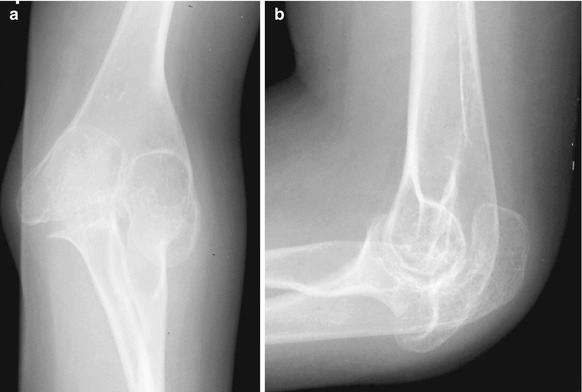
Fig. 20.10
Elbow deformity in a 13-year-old girl with polyarticular JIA. (a, b) Osteopenia, epiphyseal enlargement, and joint space narrowing (Images copyright Shriners Hospital for Children Northern California)

Fig. 20.11
Shoulder deformity in a 17-year-old girl with polyarticular JIA. There are erosions and deformity of the humeral head (Image copyright Shriners Hospital for Children Northern California)
Deformities at the hand and wrist are most common with polyarticular JIA. These include such finger deformities as flexion at the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints, Boutonniere deformity (flexion at PIP with hyperextension at DIP) (Fig. 20.12), and swan neck deformity (extension at PIP and flexion at DIP). Ligamentous laxity and sometimes mass-like hypertrophied synovium may lead to carpal subluxation or dislocation, especially common at the hamate. The wrist may deviate in a radial direction [7].


Fig. 20.12
Boutonniere deformity in a 19-year-old male with JIA (Image copyright Shriners Hospital for Children Northern California)
Patients with the psoriatic or enthesitis-related subtypes may demonstrate overgrowth and inflammation of a digit (dactylitis) (Fig. 20.13). ERA may manifest with thickening of tendons and ligaments, showing wispy periostitis along their osseous attachments.


Fig. 20.13
Sausage digit in a child with psoriatic arthritis. There is soft tissue swelling at the PIP and DIP joints, along with central erosions. Increased width of the affected phalanges results in brachydactyly (Courtesy of J. Herman Kan)
Ultrasound. Both US and MRI may be used for early assessment of the disease process (Fig. 20.14). US depicts the severity of disease by allowing assessment of joint effusions, synovial thickening, cartilage destruction/thinning, associated synovial cysts, erosions, and tenosynovitis (Figs. 20.15 and 20.16). It may identify clinically occult knee effusions as well as subclinical synovitis in multiple joints [10, 11]. Later on, it may identify enthesitis, inflammation of tendons or ligaments where they insert into the bone (most common at the calcaneal insertion of the Achilles tendon). US is especially useful for evaluating the joints of the hand and feet. It may be employed to guide joint aspiration or therapeutic injection, and it helps assess response to intra-articular treatment [7].

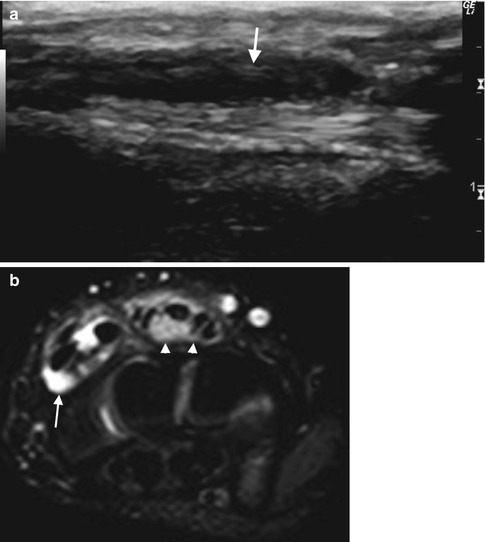
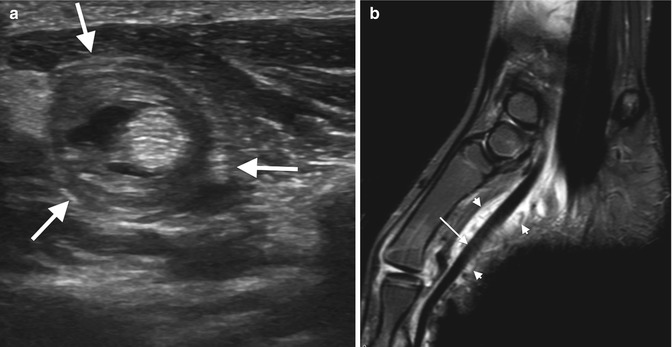

Fig. 20.14
New onset of significant left thenar atrophy, swelling around the wrist, and limited motion in a 7-year-old girl who subsequently received a diagnosis of antinuclear antibody (ANA)- and rheumatoid factor (RF)-negative JIA. (a) There is minimal lateral soft tissue swelling (arrow). (b) Longitudinal ultrasound (US) of the radial aspect of the wrist shows thickened, echogenic synovial tissue (arrow). (c) Color Doppler of the unaffected wrist shows normal flow (for comparison). (d) The affected side is hyperemic (Reprinted from Miller and Doria [37], with kind permission from Springer Science + Business Media) (Image courtesy of Andrea Doria)
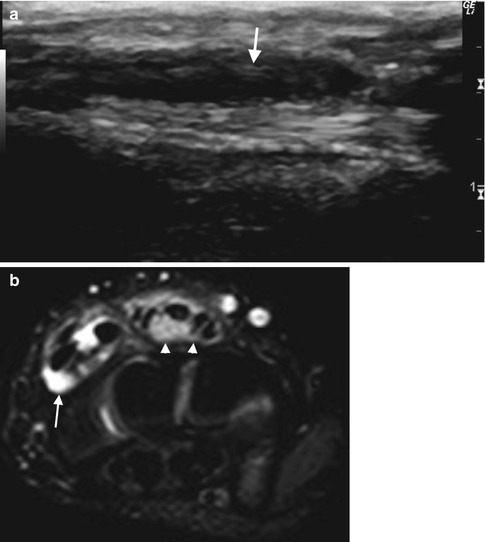
Fig. 20.15
Tenosynovitis in a 7-year-old girl with JIA. (a) Longitudinal US shows pannus along the tendon sheath (arrow). (b) Axial short tau inversion recovery (STIR) image of the wrist shows fluid (arrow) and pannus (arrowheads) surrounding thickened extensor digitorum tendons (Courtesy of J. Herman Kan)
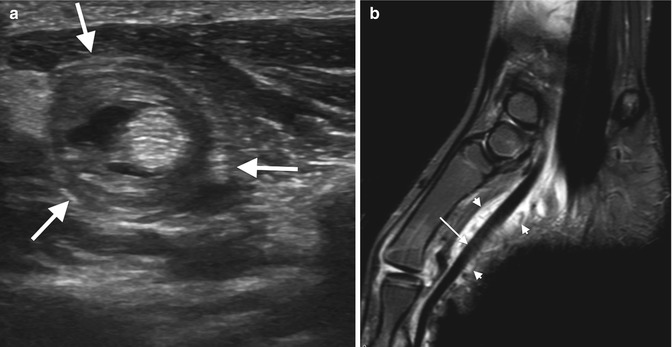
Fig. 20.16
Tenosynovitis in an 11-year-old boy. (a) Axial US of the flexor pollicis longus demonstrates circumferential thickening of the tendon sheath (arrows) and tenosynovial fluid. (b) Sagittal STIR image shows extensive tenosynovitis of the flexor pollicis longus. The tendon is thickened and mildly hyperintense (arrow), and there is surrounding fluid and soft tissue edema (arrowheads). Note fluid in the MTP joint (Courtesy of J. Herman Kan)
Synovial proliferation appears as hypoechoic, irregular synovial membrane thickening, easily distinguishable from joint fluid (see Chap. 22). With cartilage involvement, the normal smooth contour of hypoechoic cartilage is altered, and the typically sharp margins become blurred and obliterated [10]. Erosions appear as a break in the cortex that measures at least 2 mm; the floor is irregular, and adjacent marrow demonstrates acoustic enhancement [12].
If power Doppler demonstrates hypervascular pannus, disease is considered active (see Fig. 20.14). Serial US may then be used to monitor disease activity and demonstrate response to therapy, showing decreased thickness and vascularity of the synovium, as well as a decrease in joint fluid [13]. However, US provides only limited visualization of some joints (such as the sacroiliac and temporomandibular joints), and a narrow acoustic window may preclude complete assessment of large joints. The efficacy of US is also limited by difficulty in positioning and examining children whose joints are swollen and painful.
Magnetic Resonance Imaging. MRI offers optimal assessment of joint disease in JIA, and contrast-enhanced MRI is the most sensitive technique for detecting synovitis, demonstrating pathology even before the physical exam becomes abnormal. It is superior to US in depicting early inflammation and synovitis, as well as in evaluation of the cartilage. MRI readily shows marrow edema, which predicts future erosions [14]. It also accurately evaluates the late manifestations of the disease, including erosions, joint space loss, and ligamentous involvement (Figs. 20.17, 20.18, and 20.19) [7, 13, 15]. MRI thus plays an important role in determining prognosis.


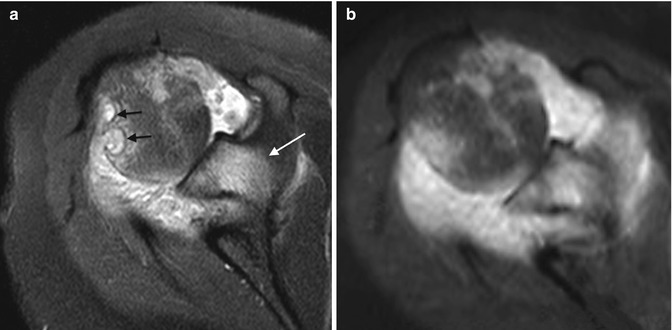

Fig. 20.17
JIA in a 14-year-old girl with polyarticular disease. (a) Coronal proton density (PD) FS image of the knee shows cartilage destruction with joint space narrowing, epiphyseal marrow edema, subcortical erosions and cysts, and deformity. Central menisci are compressed. (b) On sagittal T2-W image, synovial inflammation and joint fluid result in diffuse hyperintensity (arrows). (c) Enhancement on sagittal spoiled gradient (SPGR) gadolinium-enhanced image differentiates joint fluid (arrow) from the synovium (arrowheads) (same patient as Fig. 20.7)

Fig. 20.18
Late manifestations of JIA in an 18-year-old female. (a) Radiograph shows extensive erosions, joint space narrowing, and ulnar overgrowth. (b) Coronal T1-W image better delineates multiple erosions. (c) Coronal T1-W FS gadolinium-enhanced image shows enhancing synovium throughout all carpal joint spaces and extending into the erosions (Courtesy of J. Herman Kan)
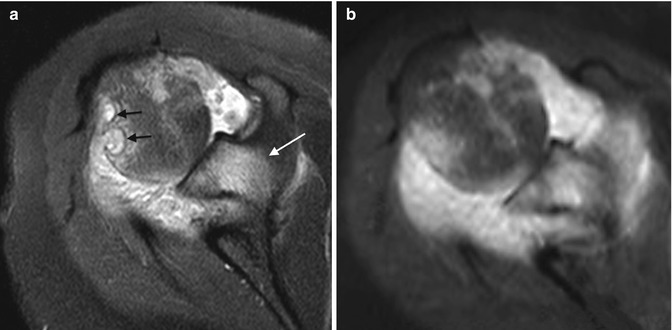
Fig. 20.19
Advanced JIA in a 16-year-old girl. (a) Axial T2-W image of the shoulder shows well-circumscribed hyperintense erosions (black arrows) in the humeral head, with osteitis (white arrow) in the adjacent scapula. (b) T1-W FS gadolinium-enhanced image shows pannus enhances diffusely (Courtesy of J. Herman Kan)
Joint effusion and acute synovitis constitute the earliest MRI manifestations in JIA (Fig. 20.20) [16]. Joint fluid and thickened synovium appear similar on conventional spin echo images. However, heavily T2-weighted (T2-W) images and fast spin echo (FSE) techniques differentiate hyperintense joint fluid from relatively hypointense synovium [13]. Normal synovium (Fig. 20.21) is at most 2 mm thick and appears hypointense on T1-weighted (T1-W) and T2-W sequences. Abnormal synovium appears as a thick, irregular, wavy layer that is hypo- to isointense on T1-W and hyperintense on T2-W sequences (Fig. 20.22). T2-W sequences may delineate frond-like pannus, formed when progressive inflammation leads to synovial proliferation (Fig. 20.23). Hypertrophic synovium may slough and undergo fibrinoid necrosis, forming intra-articular loose bodies (“rice bodies”), readily apparent on heavily T2-W images (Fig. 20.24). These loose bodies preclude the use of intra-articular steroids.
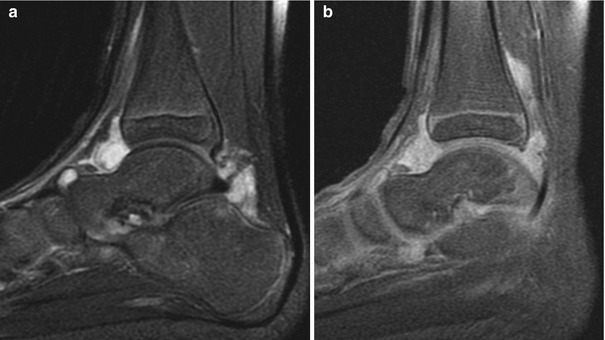
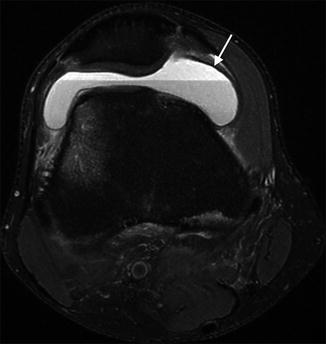
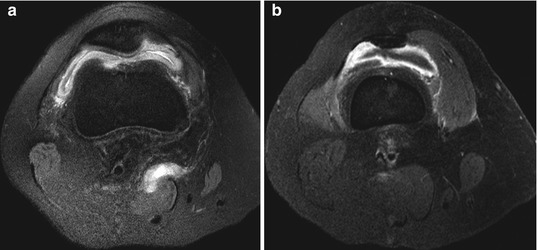
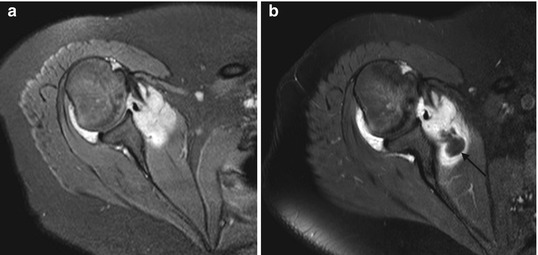
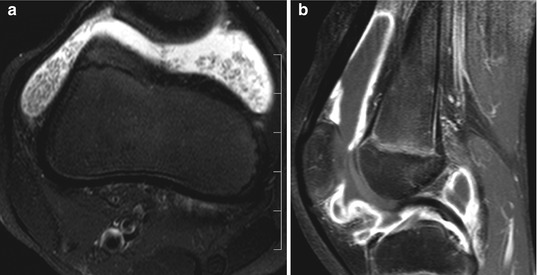
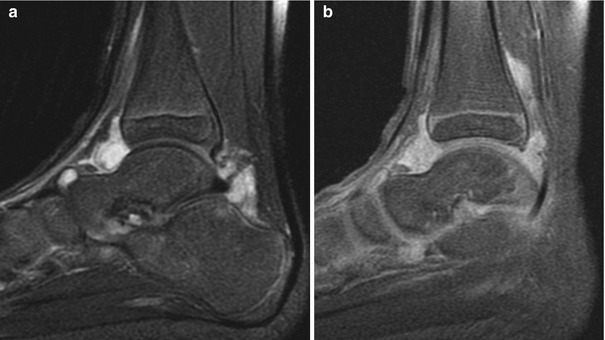
Fig. 20.20
Synovitis with enhancing pannus in a 6-year-old boy with JIA. (a) Sagittal T2-W image shows hyperintense thick material within the ankle joint. After administration of gadolinium (b, T1-W FS), all the hyperintense areas enhance, indicating they represent thickened synovium, not joint fluid. The cartilage appears intact (Courtesy of Tal Laor, Cincinnati Children’s Hospital)
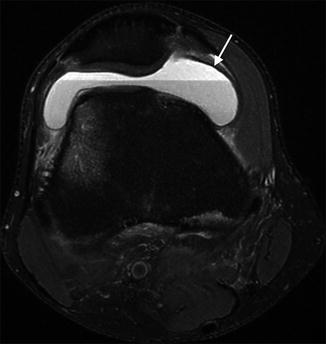
Fig. 20.21
Normal synovium. Axial PD FS image of a 17-year-old male after trauma shows normal hypointense non-thickened synovium (arrow). Note lipohemarthrosis and distal femoral marrow edema
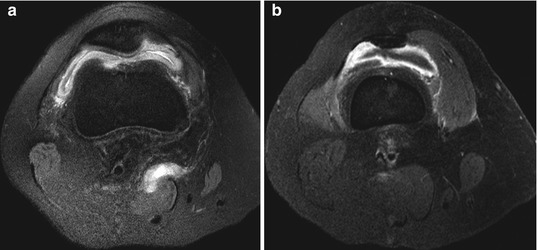
Fig. 20.22
Thickened synovium in a patient with JIA. (a) Axial PD FS image of the knee shows synovial thickening and hyperintensity along with a small amount of joint fluid. (b) T1-W FS gadolinium-enhanced image shows diffuse enhancement of the thickened synovium, along with hypointense joint fluid
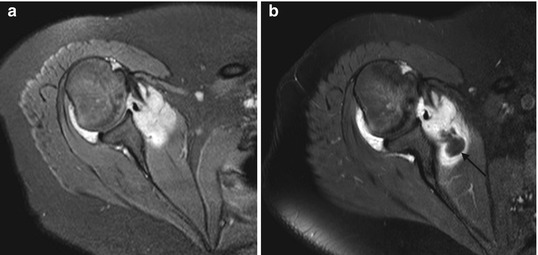
Fig. 20.23
Enhancing pannus in a 19-year-old girl with JIA. (a) T2-W FS axial image shows hyperintense fluid and pannus at the shoulder. (b) T1-W FS gadolinium-enhanced axial image contrasts non-enhancing joint fluid (arrow) and enhancing pannus (Courtesy of J. Herman Kan)
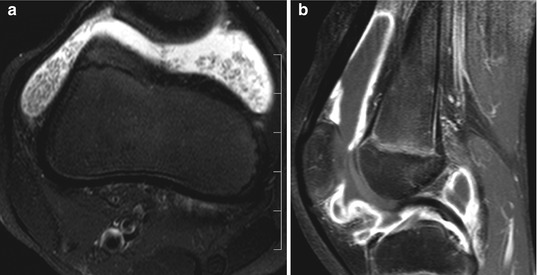
Fig. 20.24




Rice bodies in a 7-year-old girl. (a) Axial T2-W image demonstrates multiple intermediate-intensity rice bodies within hyperintense joint fluid. (b) Sagittal T1-W FS gadolinium-enhanced image shows thick, enhancing synovium, but the rice bodies are occult
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree