Aspiration refers to the misdirection of contents of the oral or upper gastrointestinal tract that have passed through the trachea and larynx and entered the lung. The diagnosis rests mostly on the history of presenting illness, medical history, vital signs, and chest radiograph. Aspiration includes a spectrum of clinical and radiologic manifestations secondary to chemical pneumonitis or bacterial pneumonia that range from asymptomatic focal inflammatory reactions with few or no radiologic abnormalities to severe life-threatening disease.
Pulmonary complications develop when there is a compromise of the usual defenses that protect the lower airways, and aspirated material affects the lower respiratory tract by direct toxic effect, sufficient volume to cause obstruction, or contamination, thus resulting in bacterial infection. The pathogenesis of lung injury depends on the amount and nature of the aspirated material, the frequency of aspiration, and the host’s response to the aspirated material. Three different clinicopathologic syndromes have been described: aspiration pneumonia, aspiration pneumonitis, and aspiration of inert fluids or particulate material. In the management of aspiration syndromes, it is important to distinguish aspiration pneumonitis from aspiration pneumonia. Aspiration pneumonia refers to pulmonary infection caused by aspiration of colonized oropharyngeal secretions; aspiration pneumonitis refers to the acute lung injury caused by the aspiration of materials inherently toxic to the lungs: gastric acid, milk, mineral oil, and volatile hydrocarbons.
The most important predisposing factors for aspiration are alcoholism, debilitating diseases, loss of consciousness, structural abnormalities of the pharynx and esophagus, neuromuscular disorders, and deglutition. Aspiration is common in normal persons during sleep or periods of diminished consciousness. Aspiration has been documented in 70% of patients in stupor or coma.
Aspiration Pneumonia
Etiology, Prevalence, and Epidemiology
Aspiration pneumonia results from aspiration of secretions containing a variety of bacteria that are normally present in the oropharynx. Healthy adults have an average of 10 to 100 million bacteria per milliliter of oropharyngeal secretions.
Although the microbial agent of aspiration pneumonia is variable, 90% of aspiration pneumonias are caused by polymicrobial flora that include enteric gram-negative bacilli, anaerobic bacteria, Staphylococcus aureus , Streptococcus pneumoniae, and Haemophilus influenzae. The most common anaerobes are Prevotella and Fusobacterium species.
Under these circumstances, aspiration material is well tolerated, and the microorganisms neither reach the alveoli nor invade the mucosa of the normal tracheobronchial tree. Pneumonia is more common when host defenses are impaired. Failure of mechanical defenses and defects in phagocytosis or ciliary function, neutropenia, and hypogammaglobulinemia can result in increased frequency or severity of pneumonia. Patients with poor dental hygiene or advanced periodontal disease are at particular risk for development of aspiration pneumonia. In these individuals the amount of bacteria per milliliter of oropharyngeal secretions may increase 100- to 1000-fold.
The pathogenesis of lung injury depends on the amount and nature of the aspirated material, the frequency of aspiration, and the host’s response to the aspirated material. During sleep, 50% of normal individuals aspirate small volumes of oropharyngeal secretions, but host defenses prevent lung infections, and the types of microorganisms aspirated are less virulent. The distinction between aspiration pneumonia and other forms of pneumonia is largely based on the clinical characteristics, but clearly overlaps exist.
Aspiration pneumonia is a major form of community-acquired pneumonia (CAP) and health care–associated pneumonia (HCAP), occurring as an acute fulminant illness or as a chronic, insidious process. As many as 5% to 15% of cases of CAP are related to aspiration. Most hospital-acquired infections result from aspiration of pharyngeal contents, and the majority of cases occur without the use of intubation or other respiratory assistance. In these patients the stomach may become colonized with gram-negative bacteria, and aspiration may overwhelm lung defenses, resulting in the development of pneumonia. Intubation and mechanical ventilation may increase the incidence and size of aspirations, with a resultant increase in the development of pneumonia. Critical factors in pathogenesis include colonization of the oropharynx with pathogenic microorganisms, aspiration of these organisms from the oropharynx into the lower respiratory tract, and compromise of the normal host defense mechanisms.
Recurrent pneumonias in the neonatal period are often the result of direct lung contamination from a congenital tracheoesophageal fistula. Acute episodes of aspiration are symptomatic, and patients usually present with symptoms of pneumonia or respiratory distress. In adults esophageal fistulas are generally acquired lesions and should be suspected in any patient with any underlying condition predisposing to aspiration. They may occur as a complication of intrathoracic malignant neoplasms (60%), infection, or trauma.
Fistulous connections between the esophagus and the lung, bronchi, or trachea are exceedingly rare in the absence of predisposing factors. Fistulas may occur in 5% to 10% of patients with advanced esophageal cancer. In such cases radiation therapy is complicated with a high risk of fistula formation. Tracheoesophageal fistula in these patients is usually incurable, and once this complication has developed, the prognosis is extremely poor. The clinical presentation is variable. Some patients present with an acute onset, whereas others have a subacute or chronic presentation. Diagnosis is usually made with a fluoroscopic esophagram. However, computed tomography (CT) may be helpful in the diagnosis of fistulous track formation in cases with normal findings on esophagography.
In the past acute aspiration was reported in 7% to 16% of patients undergoing anesthesia. However, in recent years, the frequency of aspiration of gastric contents during anesthesia has decreased considerably, and symptomatic aspiration pneumonia is currently an uncommon complication of anesthesia.
Lentil aspiration pneumonia is a granulomatous pneumonitis caused by aspiration of leguminous material, such as lentils, beans, and peas. Predisposing factors, such as neurologic disorders, structural abnormalities of the pharynx and esophagus, emergency surgical procedures, and dementia, are frequent associations. The histologic findings are characteristic and consist of an epithelioid granuloma, with or without central necrosis, in response to durable cellulose content. Repetitive aspiration episodes may result in numerous small bilateral nodules representing inflammation with foreign-body reaction in bronchioles, ducts, and alveolar sacs.
Clinical Presentation
The clinical presentation of aspiration pneumonia is variable. Some patients present with an acute onset; others have a subacute or chronic presentation. Acute aspiration is usually associated with cough, wheezing, cyanosis, dyspnea, and tachypnea. Acute aspiration is usually associated with cough, wheezing, cyanosis, dyspnea, and tachypnea; the characteristic clinical manifestations are usually those of an acute pneumonia and consist of fever, leukocytosis, increase in respiratory secretions, and purulent sputum. Less common manifestations include pleuritic chest pain and hemoptysis. However, the signs and symptoms of pneumonia may be milder or even absent in the elderly. Silent aspiration occurs during anesthesia or while a patient is intubated in the intensive care unit.
Pathologic Findings and Pathophysiology
Acute aspiration is not uncommon and represents a common incidental finding at autopsy in debilitated patients dying of other causes. Pathologic changes depend on the amount and nature of the aspirated material and the time after aspiration at which the lungs are examined. The classic pathologic appearance is a necrotizing acute bronchopneumonia in which there is a foreign-body granulomatous reaction to aspirated exogenous material. Histologically, aspiration pneumonia is characterized by the presence of edema, hemorrhage, numerous polymorphonuclear leukocytes, and foreign-body granulomas within alveolar spaces. The process centers around the bronchioles, which can be destroyed and replaced by acute inflammation and necrosis. Multinucleated giant cells are often seen in the surrounding infiltrate.
Complications associated with aspiration pneumonia include abscess formation, necrotizing pneumonia, pleural effusion, and empyema. Lung abscess is defined as an inflammatory mass within lung parenchyma, the central part of which has undergone purulent liquefaction necrosis. The most common cause of lung abscess is aspiration. The most frequently involved regions are the posterior segment of an upper lobe or the superior segment of a lower lobe, especially when aspiration occurs in a supine position.
Manifestations of the Disease
Radiography
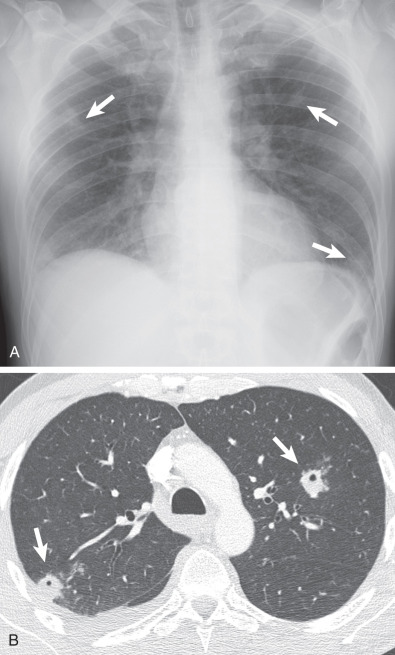
The chest radiograph typically demonstrates unilateral or bilateral patchy or confluent consolidation involving mainly the dependent lung regions ( Fig. 64.1 ). The location of pneumonia depends on the position of the patient when aspiration occurs. In recumbent patients diffuse perihilar consolidation reflects pneumonia involving mainly the posterior segments of the upper lobes or superior segments of the lower lobes; in upright patients consolidation is seen mainly in the basal segments of the lower lobes. Consolidations may be simultaneously present in various lobes when a large volume of fluid is aspirated ( Fig. 64.2 ).


Prolonged clinical course or large aspirations may result in severe necrotizing bronchopneumonia or lung abscess formation occurring 8 to 14 days after the initial aspiration event. Lung abscesses consist of single or multiple, often cavitary, nodules or masses usually measuring 2 to 6 cm in diameter. Their internal margins are smooth in 90% of cases and shaggy in 10%. Air-fluid levels are seen in 70% of cases and adjacent parenchymal consolidation in 50% ( Fig. 64.3 ). Lung abscesses may be seen anywhere in the lungs but are most commonly located in the dependent regions ( Fig. 64.4 ). Neither clinical nor radiographic features permit a specific diagnosis of lung abscess.


When aspiration is secondary to congenital tracheobronchial fistulae, the radiologic manifestations are variable, depending on the spread and severity of the aspiration. The most common radiographic pattern is that of bronchopneumonia with patchy airspace opacities. The most useful diagnostic imaging modality is esophagram, and barium is the best contrast agent to use to demonstrate the presence of a fistula ( Fig. 64.5 ). In adults radiographic findings are nonspecific. Diagnosis should be strongly suspected in any patient with a known esophageal carcinoma in whom there is evidence of recurrent pneumonias ( Fig. 64.6 ). Consolidation is usually unilateral but may involve both lungs.


Bronchopleural fistula, defined as a communication between the bronchus or lung parenchyma and pleural space, is a known complication of necrotizing pneumonia that may accompany aspiration ( Figs. 64.7 and 64.8 ).


Elderly persons may have diminished production of saliva as a result of medications and oral/dental disease, leading to poor oral hygiene and oropharyngeal colonization with pathogenic organisms. A distinct form of infection is caused by Actinomyces israelii , an anaerobic bacterium that is normally found in the mouths of patients with poor oral hygiene. Aspiration of infected material results in a localized or lobar pneumonia, usually in the dependent portions of the lung. Although radiologic features include focal or patchy ill-defined consolidations and progressive abscess formation, pulmonary actinomycosis can mimic a broad spectrum of pathologies, from benign infection to lung cancer. If untreated, actinomycosis spreads, invading the chest wall, the mediastinum, or the diaphragm (see Fig. 64.4 ).
Computed Tomography
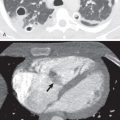
Similar to the radiographic findings, CT manifestations of aspiration pneumonia consist of unilateral or bilateral patchy or confluent consolidation and ground-glass opacities involving mainly the dependent lung regions. Other common findings include centrilobular branching structures (“tree-in-bud” opacities) and centrilobular nodules, reflecting cellular bronchiolitis, peribronchiolar inflammation, and interlobular septal thickening. Airspace nodules, ground-glass opacities, and lobular consolidation are seen better by CT than by conventional radiography. In patients with infection secondary to aspiration of contaminated secretions, as from periodontal disease, the CT findings may also include multiple rounded opacities surrounded by a halo of ground-glass opacity that may mimic septic emboli. The opacities are usually unilateral but may involve both lungs ( Fig. 64.9 ). These may progress to abscess formation and cavitation.
Differential Diagnosis
The most useful imaging modalities available for the evaluation of patients with known or suspected aspiration pneumonia are chest radiography and CT. Imaging examinations should always be interpreted with awareness of the clinical findings, including duration of symptoms, presence of fever, cough, and dyspnea, and the degree of leukocytosis. Knowledge of the immune status of the patient is helpful in arriving at a short list of most likely causative organisms. In the absence of clinical information, radiologists cannot reliably distinguish between pneumonia and other pulmonary processes.
Although certain radiologic patterns are highly suggestive of pneumonia, chest radiography is of limited value in determining the specific etiology. Distinction of localized pneumonia from other pulmonary processes cannot be made with certainty by imaging. Diagnosis is equally difficult when pneumonia manifests with diffuse bilateral opacities. Other conditions that also commonly manifest with diffuse bilateral opacities include pulmonary edema and acute respiratory distress syndrome (ARDS).
Aspiration Pneumonitis
Etiology, Prevalence, and Epidemiology
Aspiration pneumonitis refers to the acute lung injury caused by the aspiration of materials inherently toxic to the lungs, such as gastric acid, milk, mineral oil, and volatile hydrocarbons. Pneumonitis caused by aspiration of large amounts of gastric contents (Mendelson syndrome) is the most serious aspiration syndrome, with a mortality rate ranging from 30% to 70%. Vomiting with massive pulmonary aspiration of gastric contents is a very frequent phenomenon and is probably one of the most common etiologies of aspiration diseases. This syndrome occurs in patients who have a marked disturbance of consciousness, including from a drug overdose, seizures, or a massive cerebrovascular accident. Today, pulmonary aspiration of gastric contents is a rare complication during modern anesthesia.
The magnitude of injury is directly related to the pH and volume of aspirated material. Severe pulmonary damage occurs predominantly when the pH of the aspirate is less than 2.5 and the volume more than 25 mL. Because gastric acid prevents the growth of bacteria, the contents of the stomach are sterile under normal conditions. Colonization of the gastric contents by potentially pathogenic organisms may occur when the pH in the stomach is increased by the use of antacids, histamine H 2 –receptor antagonists, or proton-pump inhibitors.
Gastrointestinal conditions related with gastric acid aspiration include vomiting, gastroesophageal reflux, achalasia, and hiatal hernia. Acid liquid introduced into the airways is rapidly disseminated throughout the bronchial tree and lung parenchyma, producing a chemical pneumonitis within minutes. The overall mortality rate associated with massive aspiration is approximately 30% and exceeds 50% in those patients with initial shock or apnea, secondary pneumonia, or ARDS. The posterior segments of the upper lobes or superior segments of the lower lobes are most frequently involved when the patient is recumbent.
Aspiration of barium contrast medium is a well-recognized complication that occurs during radiologic examination of the gastrointestinal tract and can have serious consequences in weak and debilitated patients. Predisposition to barium aspiration is caused by several factors, including swallowing disorders or recent esophageal surgery. The overall mortality rate associated with massive barium aspiration is approximately 30% and exceeds 50% in those patients with initial shock or apnea, secondary pneumonia, or ARDS. Water-soluble nonionic contrast medium may be the cause of significant morbidity but does not cause intense chemical pneumonitis as occurs with aspirated ionic water-soluble contrast media.
Acute aspiration of volatile hydrocarbons may cause a chemical pneumonitis. Most cases of hydrocarbon pneumonia are related to accidental poisoning in children. Adult fire-eaters use liquid hydrocarbons, such as petroleum, for the performance of the flame-blowing part of the show. For flame blowing, the performer blows out a mouthful of liquid hydrocarbon against a burning stick, thus creating an aerosol that catches fire around the stick. This entity is rare but easily diagnosed on the basis of clinical history. A relatively common late complication of hydrocarbon aspiration is the development of pneumatoceles.
Clinical Presentation
The characteristic clinical presentation of gastric acid pneumonitis is abrupt in onset, with dyspnea, cyanosis or arterial hypoxemia, low-grade fever, rales, and opacities on chest radiography. The clinical course is variable. In a retrospective study of 50 patients with gastric acid pneumonitis, 12% of the patients died shortly after aspiration, 62% had rapid clinical and radiologic improvement (mean time, 4.5 days), and 26% demonstrated rapid improvement but then had clinical and radiographic progression associated with recovery of bacterial pathogens from the sputum and a fatal outcome in more than 60%. Long-term follow-up studies demonstrate either complete recovery or radiographic evidence of pulmonary fibrosis.
Pathologic Findings
The pathologic changes of chemical lung injury include focal and confluent areas of edema with protein-rich fluid in the alveolar spaces, hyaline membrane formation, and denudation of the alveolar epithelium. Diffuse alveolar damage (i.e., ARDS) after severe acute chemical injury is nonspecific and indistinguishable to that of other etiologies.
Manifestations of the Disease
Radiography
The characteristic radiographic appearance of acute pure gastric acid aspiration is that of bilateral perihilar ill-defined consolidation. The normal size of the heart and the absence of signs of pulmonary venous hypertension help differentiate this form of edema from that of cardiac origin. ( Fig. 64.10 ). Radiographic changes may worsen for several days in uncomplicated cases, but improvement is generally manifested within the first week after aspiration. Worsening of opacities after initial improvement suggests development of superimposed bacterial pneumonia, ARDS, or pulmonary embolism.

In hydrocarbon aspiration, chest radiograph shows scattered pulmonary opacities that are almost invariably bilateral with middle and lower lung zone predominance. Although consolidations tend to clear over the next few days, formation of pneumatoceles may also occur ( Fig. 64.11 ). Hydrocarbon aspiration may be complicated with the development of a bronchopleural fistula and spontaneous pyopneumothorax.

Aspiration of barium results in a characteristic appearance of high-density material in the dependent lung regions ( Fig. 64.12 ).