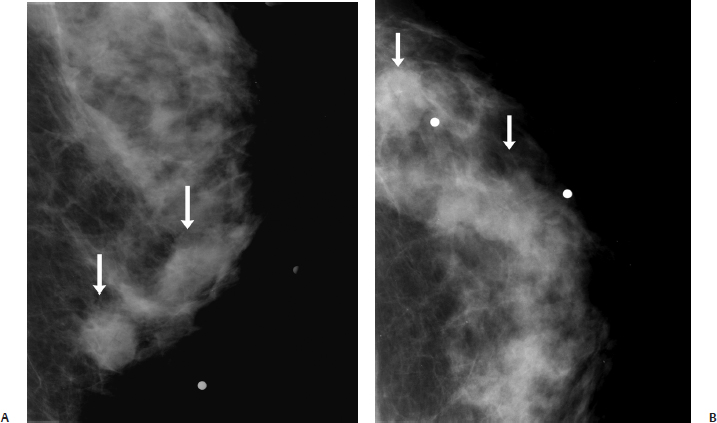
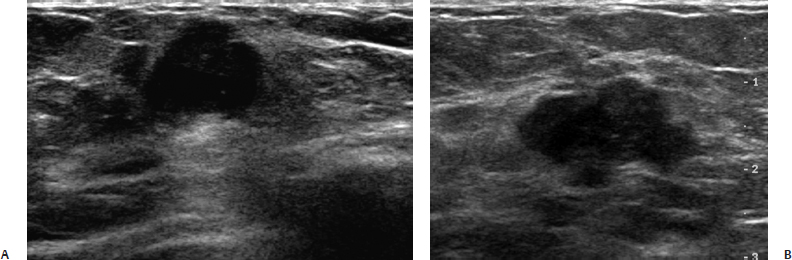
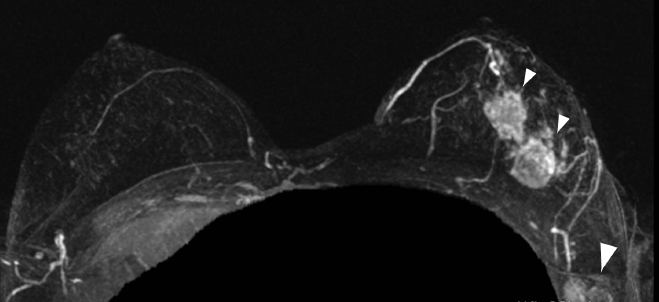
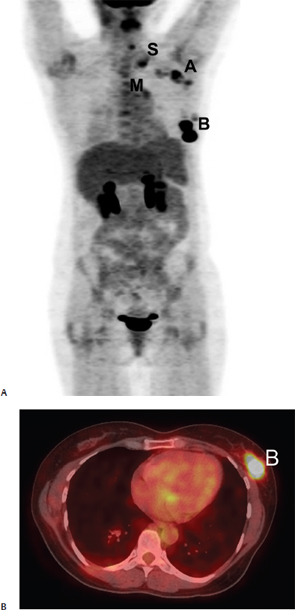
36 Assessing Response to Therapy A 47-year-old woman presents with a palpable left breast mass. • Palpable lump in the left 4 o’clock position Mass (Fig. 36.1) • Two masses have the same characteristics. • Margin: ill defined • Shape: irregular • Density: equal density Fig. 36.1 In the left outer inner quadrant, there are two irregular masses (arrows). (A) Left ML spot compression. (B) Left CC spot compression. Fig. 36.2 The left breast palpable masses and the mammographic masses correspond to two solid irregular masses at the 4 o’clock and 5 o’clock positions. (A) Left transverse breast sonogram of the mass at the 4 o’clock position. (B) Left transverse breast sonogram of the mass at the 5 o’clock position. Fig. 36.3 Contrast-enhanced bilateral breast MRI maximum projection intensity (MIP) image. There are two highly enhancing suspicious irregular masses that correspond to the sonographic masses (small arrowheads). Suspicious enhancing axillary adenopathy is also evident (large arrowhead). Fig. 36.4 The positron emission tomography–computed tomography (PET-CT) scan performed after the MRI demonstrates extensive 18F-fluorodeoxyglucose (FDG) uptake in the left breast (B), axillary (A), supraclavicular (S), and mediastinal (M) region. (A) Maximum intensity projection (MIP) PET image prior to chemotherapy. (B) Axial PET-CT prior to chemotherapy. Fig. 36.5 After 4 months of chemotherapy, PET-CT demonstrates resolution of the uptake in the left breast and previously abnormal lymph nodes. (A) MIP PET image after 4 months of chemotherapy. (B) Axial PET-CT image after 4 months of chemotherapy. • Left mastectomy and axillary dissection (performed 2 weeks after the second positron emission tomography [PET] scan) demonstrates a residual invasive ductal cancer 0.8 cm in size. Six of eight axillary nodes exhibit metastatic disease. The largest metastatic axillary nodal involvement is < 2 mm. • Left mammographic and sonographic mass: BI-RADS assessment category 5, highly suggestive of malignancy • This case illustrates the usefulness of PET in following a patient’s response to preoperative neoadjuvant systemic therapy. Multiple investigators have shown that PET is an important method to monitor the effect of these drug regimens. A 55 to 60% serial reduction in the tumor 18
Case 36.1: Assessing Response to Therapy
Case History
Physical Examination
Mammogram
Ultrasound (Fig. 36.2)
Other Modalities: MRI and PET-CT (Figs. 36.3, 36.4, and 36.5)
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine