Key Point
- ▪
The high spatial resolution and excellent field of view of CCT enables it to depict a range of myocardial, septal, and other structural lesions.
Myocardial Crypts
Myocardial crypts (or clefts) have been defined as discrete V-shaped extensions of the blood pool inserting more than 50% into the compact myocardial wall that tend to be less visible during systole and are not associated with local hypokinesis or dyskinesia. Increased prevalence of crypts has been reported in carriers of the gene for hypertrophic cardiomyopathy (as much as 81%). However, myocardial crypts also are seen in normal subjects, so their precise significance has yet to be determined.
For CCT images of myocardial crypts, see Figures 20-1 and 20-2 ;
Myocardial Diverticulum
Congenital left ventricular (LV) diverticula are rare cardiac malformations characterized as outpouchings of the myocardium and can be fibrous or muscular. The prevalence has been reported between 0.02% and 0.04%. They are associated with other congenital abnormalities in about 70% of cases. Muscular diverticula typically are apical and have a full-thickness myocardial wall with preserved systolic contraction. Diverticula can be differentiated from crypts or clefts by a narrow mouth but a wide outpouching extending beyond the normal LV margins. Cardiac CT (CCT) has been proposed as useful for differentiating aneurysm from pseudoaneurysm by exclusion of coronary artery disease, visualization of the LV wall layers, and dynamic assessment of regional wall function ( Fig. 20-3 ).
Post-Infarction Ventricular Pseudoaneurysms, Septal Rupture, and Intramyocardial Hematoma
Pseudoaneurysms are an uncommon complication of acute myocardial infarction, occurring in less than 1% of cases. Cardiac surgery, penetrating or other trauma, and infection also can lead to the development of these abnormalities. The excellent spatial resolution of CT should be ideal for identifying the myocardial wall disruption. Single case reports have demonstrated the ability of CCT to depict post-infarction ventricular pseudoaneurysms, and coronary anatomy.
- □
Post-infarction septal rupture and intramyocardial hematoma also have been noted in single case reports.
- □
For CCT images of post-infarction pseudoaneurysms, see Figure 20-4 .
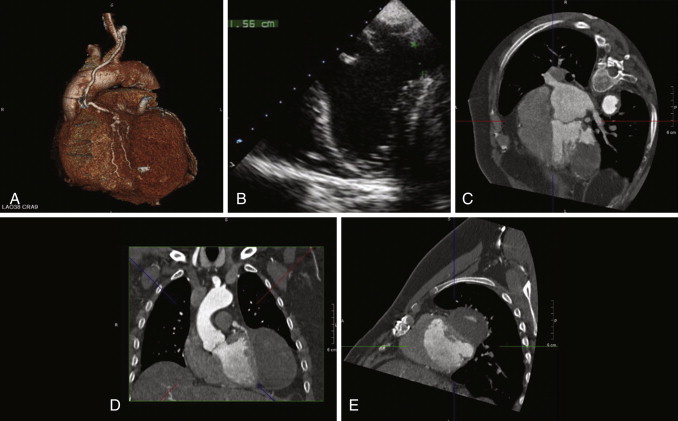
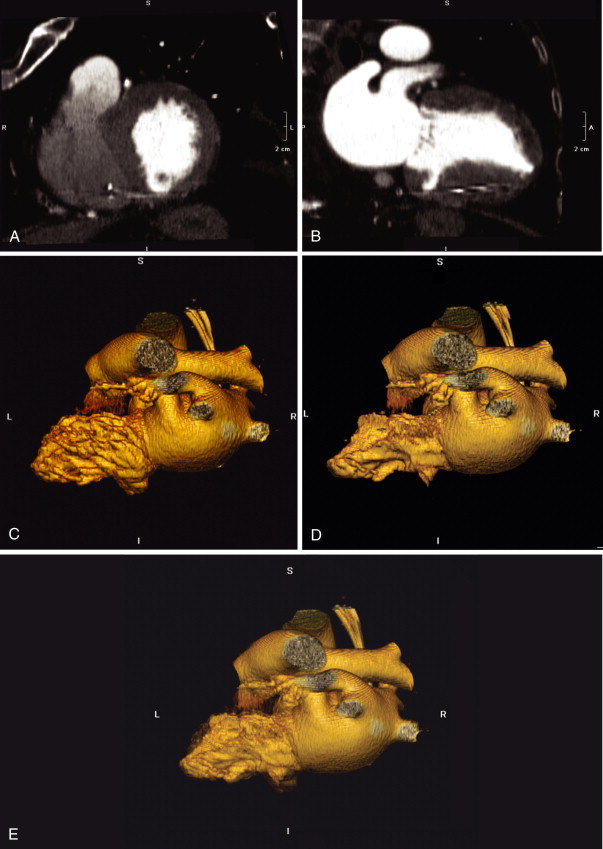
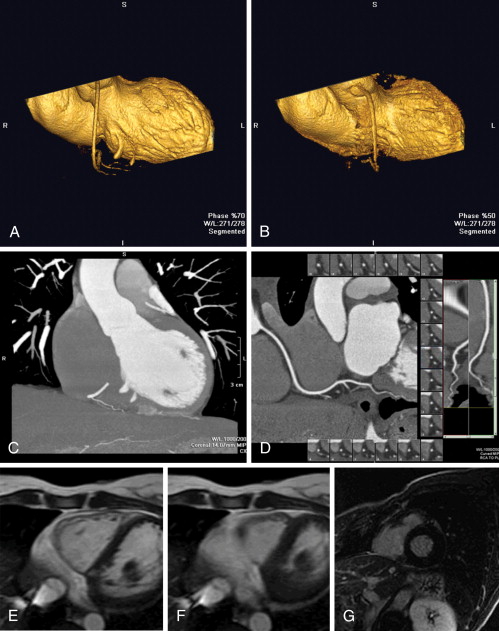
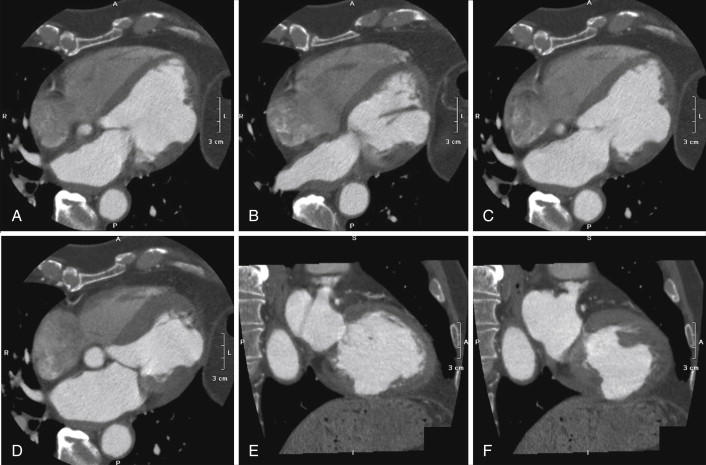
Figure 20-4
A, Three-dimensional volume-rendered image shows the patent left internal mammary to left anterior descending artery graft in relation to the left ventricular pseudoaneurysm (LVPA). B, Transesophageal image shows the large LVPA arising from the lateral wall below the mitral valve and reveals the abrupt myocardial discontinuity marking the neck of the LVPA. Cardiac CTA modified four-chamber ( C ), horizontal long-axis ( D ), and two-chamber ( E ) views of the heart show the posterobasal opening of the LVPA and its relation to adjacent cardiac structures.
(Reprinted with permission from Yavari A, Sriskandan N, Khawaja MZ, et al. Computed tomography of a broken heart: chronic left ventricular pseudoaneursym. J Cardiovasc Comput Tomogr . 2008; 2:120.)
- □
For CCT images of post-infarction septal rupture, see Figures 20-5 and 20-6 ;
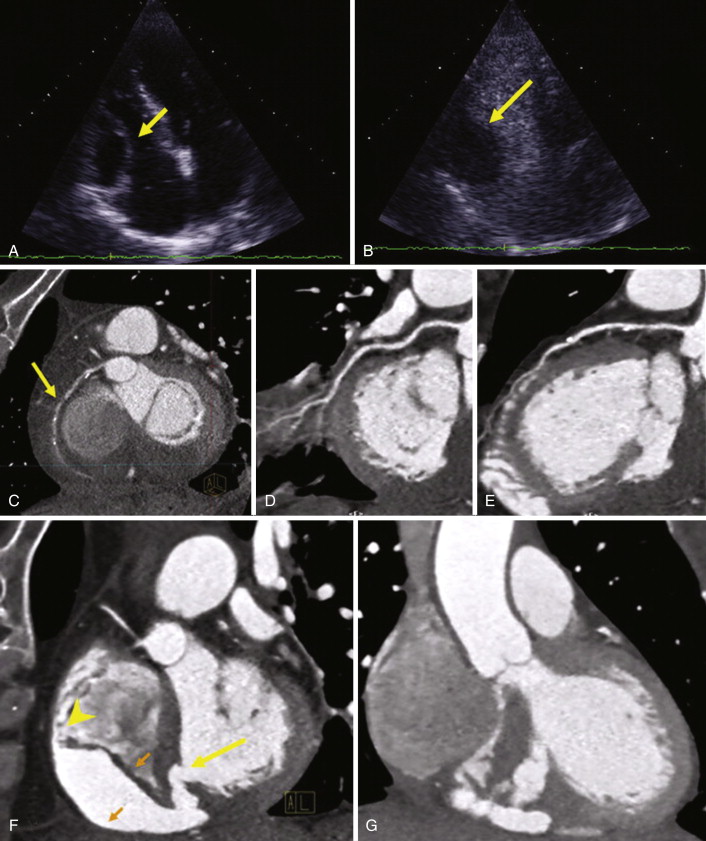
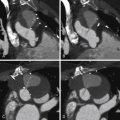
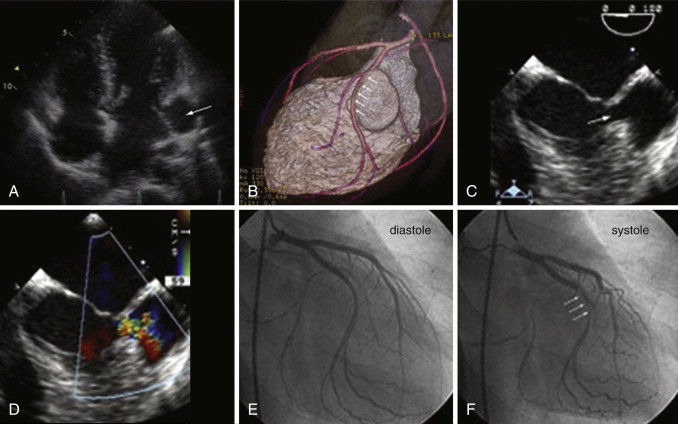
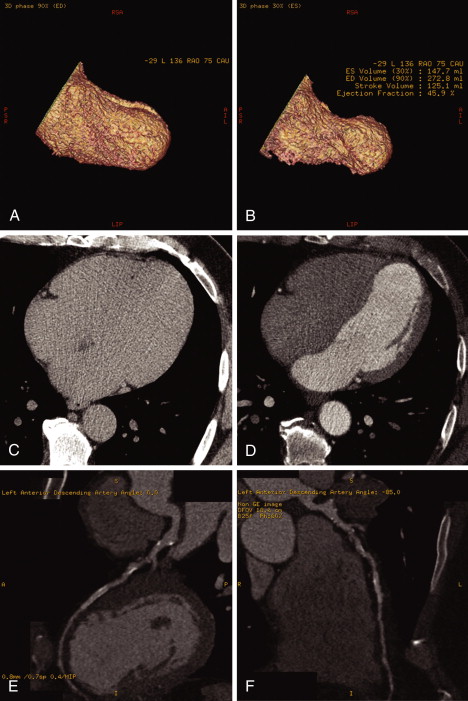
Figure 20-5
A, Four-chamber view echocardiogram with a cavity by the right ventricle ( arrow ). B, Four-chamber view after intravenous contrast, showing no enhancement of the structure ( arrow ). Curved multiplanar reconstructions show that the right coronary artery ( C ) has a high-grade lesion ( arrow ) and poor contrast opacification in the distal portion of the artery, and that there is nonsignificant stenosis of the left circumflex artery ( D ) and of the left anterior descending artery ( E ). F, Short-axis view shows the ventricular septal rupture ( larger arrow ), the myocardial dissection ( two small arrows at both sides of the right ventricular wall), and the re-entry orifice on the right ventricle ( arrowhead ). G, Multiple orifices document the complex anatomy of the ventricular septal rupture.
(Reprinted with permission from Bittencourt MS, Seltmann M, Muschiol G, Achenbach S. Ventricular septal rupture and right ventricular intramyocardial dissection secondary to acute inferior myocardial infarction . J Cardiovasc Comput Tomogr . 2010;4(5): 342-344.) See
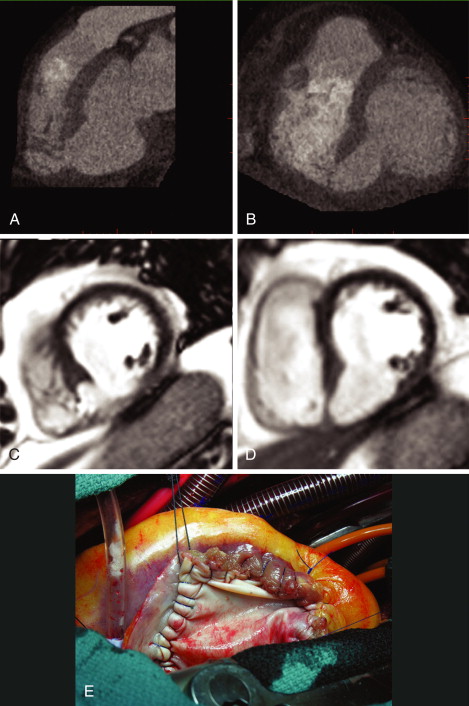
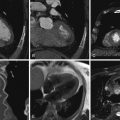
Figure 20-6
ECG-gated contrast-enhanced CT images ( A and B ), steady-state free precession cardiac MR (CMR) images ( C and D ), and photo ( E ) of the surgical repair of a post-infarction septal rupture. The CT and CMR images reveal the aneurysmal deformation of the inferior septum as well as the inferior wall. The CT images in particular reveal the detail of the septal rupture (fenestrations of the thinned aneurysmal septum). The thinness of the aneurysmal inferior septum and inferior wall is most obvious on the CMR images. The surgical photo shows the thinness of the aneurysmal septum, adjacent to the pericardial patch. See
Post-Infarction Left Ventricular Aneurysm
True aneurysms of the LV most commonly are secondary to myocardial infarction but can (rarely) be congenital in origin or secondary to inflammatory (e.g., Kawasaki disease and sarcoidosis) or infectious (e.g., Chagas) disease. Occasionally changes associated with right ventricular dysplasia or hypertrophic cardiomyopathy also can be associated with LV aneurysm formation.
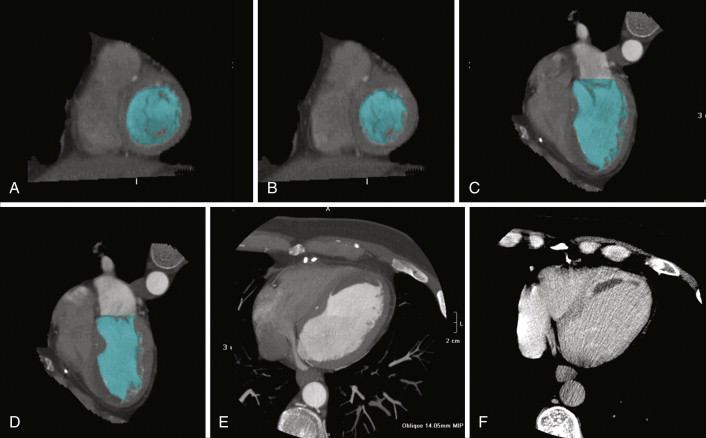
For CCT images of ventricular aneurysms, see Figures 20-7 through 20-10 ;

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree