Key Points
- ▪
Cardiac CT is able to image both biologic and mechanical cardiac valve prostheses.
- ▪
Helical CCT scanning enables recognition of normal or impaired occluder motion.
- ▪
Thrombus or pannus on mechanical valves can be depicted by CCT scanning.
- ▪
Atrial fibrillation is more common in patients with mitral prostheses, making CCT scanning less useful in such cases.
- ▪
Hemodynamic limits of patients with prosthetic valve dysfunction will preclude many from undergoing CCT scanning.
Currently, only preliminary data are available on the evaluation of prosthetic cardiac valves by CCT, although contemporary CCT, if cardiac gated, can yield excellent images of many prosthetic valves. Prosthetic valve disease, though, is prone to many of the factors that pose significant technical limitations or usual exclusions to cardiac CT, such as a high incidence of atrial fibrillation associated with prostheses in the mitral valve position, in particular.
Retrospectively gated helical imaging is the best means to assess prosthetic, especially mechanical, valves, and contrast enhancement improves image quality and diagnostic confidence.
Prosthetic Valves
Transthoracic echocardiography (TTE) and especially transesophageal echocardiography (TEE) have been the mainstays of bioprosthetic and mechanical prosthetic valve assessment, by virtue of the combination of two-dimensional imaging and spectral and color Doppler modalities. However the limitations of echocardiography are real, and these limitations are regularly encountered in busy laboratories and hospitals:
- □
Inability to resolve transvalvular versus paravalvular insufficiency
- □
Inability to image thrombus or pannus within the valve ring of a mechanical aortic valve prosthesis
- □
Inability to distinguish thrombus from pannus
- □
Inability to image an abscess on the far side of an aortic valve replacement (AVR) ring because shadowing or reverberation from the ring is projected onto the far root
- □
Inability to image an AVR well because of a mechanical mitral valve replacement (MVR) projecting reverberation artifact and shadowing onto the AVR
- □
Inability to adequately image the occluders of an AVR to determine their excursion
- □
Inability to distinguish postoperative inflammatory changes and hematomas from early infection-related changes
- □
Inability to assess the pulmonic valve by TEE due to near-field shadowing and reverberations from an AVR
Among a series of 170 patients with 208 mechanical prostheses who underwent surgery, echocardiographic diagnostic errors were encountered in 7% of MVRs and 15% of AVRs. The most common mistakes were the following :
- □
Lack of surgical confirmation of paravalvular insufficiency: 36% of errors
- □
Failure to identify pannnus overgrowth: 4% of errors
- □
Failure to identify thrombus/pannus overgrowth: 4% of errors
- □
Failure to identify vegetations: 4% of errors
- □
Failure to identify ball variance: 4% of errors
- □
Erroneous diagnoses: 28% of errors
- □
AVR misclassification of aortic insufficiency (AI) as transvalvular: 28% of errors
- □
AVR misclassification of AI as paravalvular: 8% of errors
Although the primary means of assessing valve prostheses remains echocardiographic, there appears to be a complementary role for CCT, because most prosthetic valves are well imaged by CCT, which is not necessarily the case with TTE and TEE. Some very old models of mechanical prostheses contain a large amount of ferrous metal that generates prohibitive artifact. Most contemporary bileaflet occluder “mechanical“ valves are so well seen that it is necessary to have a high degree of familiarity with the structure and motion of different models to understand the imaging findings.
Assessing the opening angle of the occluder elements of a mechanical prosthesis is one of the traditional means of establishing the normality of mechanical prosthesis function, or, alternatively, obstruction by thrombus, pannus, or both; vegetations; tissue; or primary mechanical failure. Fluoroscopy or cineradiology can measure the opening angle accurately (difference between real and measured opening angles: –0.7 ± 1.8 degrees) and with high reproducibility (to within –0.1 ± 0.8 degrees). Pressure gradient recording or Doppler calculations of gradients by TTE or TEE are complementary to two-dimensional imaging findings by CT.
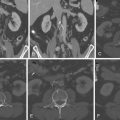
The opening and closing angles of mechanical prosthesis occluder motion can be accurately assessed or measured using CCT.
Obstructing pannus or thrombus also can be identified using CCT.
The opening, closing, and range of occluder motion vary for different tilting disc models of mechanical valve replacements ( Table 17-1 ).
| MODEL | OPENING ANGLE (°) | CLOSING ANGLE (°) | EXCURSION (°) |
|---|---|---|---|
| Bileaflet Hemidisc Occluder | |||
| Carbomedics (Sorin Group, Milan, Italy) | 78 | 35 | 43 |
| St. Jude Medical (St. Paul, MN) | 85 | 35 | 50 |
| Single Tilting Disc Occluder | |||
| Bjork-Shiley (Irvine, CA) | 60 | 0 | 60 |
| Medtronic-Hall (Minneapolis, MN) | 60 | 0 | 60 |
| Omniscience (Medical CV, Ivea Grove Heights, MN) | 60 | 0 | 60 |
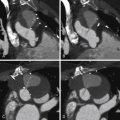
Current bileaflet occluder mechanical valves (e.g., those manufactured by St. Jude Medical, Inc., St. Paul, MN, or Carbomedics) generate little artifact, and the sewing ring and occluders are clearly imaged with non–contrast-enhanced imaging. Single tilting disc valves also can be well imaged. The motion of the occluders can thus be assessed for obstruction due to thrombus or pannus on cine imaging. The opening angle is established with reference to the plane of the base of the sewing ring. Cardiac CT is able to accurately determine the opening angle.
Identification of thrombus or pannus requires contrast enhancement of the blood pool.
Assessment of occluder motion of bileaflet mechanical valves in the aortic position is difficult by TEE because the valve ring is oriented away from the probe, and fluoroscopy is variably able to convincingly depict occluder motion; hence, CCT may provide a novel contribution.
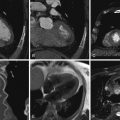
The wire struts of bioprostheses (e.g., Edwards Lifesciences, Irvine, CA) are easily seen, and the leaflets also may be seen. The heavy metal struts (stents) of some models may generate artifacts.
Complications of valve replacement surgery such as pseudoaneurysms of the left ventricular outflow tract and ascending aorta are well depicted by CCT.
For images of normal bileaflet occluder prosthetic mechanical heart valves, see Figures 17-1 through 17-4 ;




For images of single tilting disc prosthetic mechanical heart valves, see Figures 17-5 and 17-6 ;


For images of obstructed bileaflet occluder prosthetic mechanical heart valves, see Figures 17-7 through 17-9 ;