Introduction
The upper extremity arterial system requires a different diagnostic approach than that used in the lower extremity. Although progression of focal atherosclerosis or acute arterial emboli are almost always the cause of symptomatic disease in the lower extremity, upper extremity arterial disease is more complex. Mechanical compression in the thoracic outlet region, vasospasm of the digital arteries, trauma-related thrombi in the hand or wrist, arteritis, and emboli from the heart or from proximal arm aneurysms are pathologies to be considered when evaluating the upper extremity arteries. The arteries of the hand have many anatomic variants and their evaluation may require a high level of technical expertise. Specialized probes that have sufficient resolution to visualize small vessels and detect low blood flow velocity signals are often required. Physicians and sonographers may sometimes feel out of their comfort zone when it comes to evaluating the arm arteries because of the overall low prevalence of native upper extremity arterial disease and the infrequent requests for these examinations. However, the introduction of arterial evaluations for dialysis fistula placement and evaluation, radial artery catheterization, and radial artery harvesting for coronary artery bypass surgery or skin flap placement have increased demand for these tests.
This chapter provides the basics of upper extremity arterial assessment including:
- 1.
Basic review of the anatomy
- 2.
Patient evaluation
- 3.
Physiologic testing
- 4.
The appropriate ultrasound imaging technique
- 5.
An overview of the pathologies that might be encountered
Basic Anatomy
The upper extremity arterial system takes origin from the aortic arch ( Fig. 13.1 ). On the right, there is a common trunk, the innominate or right brachiocephalic artery, that then bifurcates into the right common carotid artery (CCA) and subclavian artery. On the left, the subclavian artery originates directly from the aortic arch. The subclavian artery continues to the lateral edge of the first rib where it becomes the axillary artery. The axillary artery courses underneath the pectoralis minor muscle, crosses the teres major muscle, and then becomes the brachial artery. The brachial artery continues down the arm to trifurcate just below the elbow into the radial, ulnar, and interosseous (or median) arteries. The radial and ulnar arteries are the dominant branches that continue to the wrist.
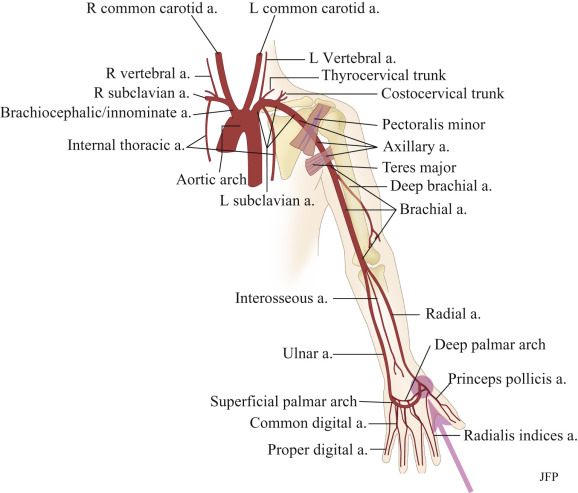
The radial and ulnar arteries typically (most common variant) join in the hand through the superficial and deep palmar arches that then feed the digits through common palmar digital arteries and communicating metacarpal arteries. The radial artery takes a course around the thumb to send branches to the thumb (princeps pollicis) and a lateral digital branch to the index finger (radialis indices). It then goes on to form the deep palmar arch with the ulnar artery. A superficial radial artery branch originates before the major radial artery branch deviates around the thumb and then continues to join the ulnar artery through the superficial palmar arch. The deep and superficial palmar arches may not be complete in anywhere from 3% to 20% of hands, hence the concern for hand ischemia after harvesting of the radial artery for coronary artery bypass grafting or as part of a skin flap.
Normal imaging protocol
The upper extremity arterial examination normally starts at the proximal subclavian artery ( Fig. 13.2 ). The entire course of each major artery is imaged, including the subclavian ( Figs. 13.3 and 13.4 ), axillary ( Fig. 13.5 ), brachial ( Figs. 13.5 and 13.6 ), radial, and ulnar ( Fig. 13.7 ) arteries. The distal radial artery, princeps pollicis artery, deep palmar arch, superficial palmar arch, and digital arteries are selectively imaged on the basis of the clinical indication ( Figs. 13.8 to 13.12 ).











Because the arm arteries are mostly superficial, high-frequency transducers are used. Most, or sometimes all, of the arteries in the arm can be imaged with transducers set at frequencies between 8 and 15 MHz. However, some areas near the clavicle may require the use of 3- to 8-MHz transducers. Imaging of hand arteries requires very high frequency transducers because these vessels are extremely small and superficial. Intraoperative transducers work quite well for imaging the digital arteries because they have a small footprint and operate at frequencies between 10 and 15 MHz.
Color Doppler ultrasound is used to identify blood flow within the vessels and to give the examiner an idea of the velocity and direction of blood flow. Pulsed-wave Doppler signals and angle-corrected Doppler waveforms are used to determine blood flow velocities at selected portions of the artery.
Normal, angle-corrected peak systolic velocities (PSVs) within the proximal arm arteries, such as the subclavian and axillary arteries, generally run between 70 and 120 cm/s. Brachial artery PSVs range from 50 to 100 cm/s. Velocities in normal radial and ulnar arteries range between 40 and 90 cm/s, whereas velocities within the palmar arches and digits are lower. Normal upper extremity Doppler waveforms are triphasic but the waveforms can change in response to the ambient temperature and to maneuvers such as making a fist, especially when acquired near the hand ( Fig. 13.13 ). The large arteries of the upper arm and forearm are relatively easy to identify and evaluate with ultrasound. Imaging the small arteries of the hand is very challenging for several reasons. Not only are the vessels small, there are numerous anatomic variations. Furthermore, the vascular anatomy of the hand described herein is a simplified version of the actual anatomy because detailing all of the arterial variants of the hand is beyond the scope of this chapter. The anatomy as shown in this chapter is sufficient to perform a comprehensive examination of the upper extremity arteries.
- •
The proximal upper extremity arterial anatomy is different between the right and left sides:
- •
The left subclavian artery has a direct origin from the aorta.
- •
The right subclavian artery and the right CCA are branches of the innominate (right brachiocephalic) artery.
- •
- •
The standard examination extends from the neck to the wrist.
- •
Specialized imaging of the hand can be performed to detect disease of the digital arteries.
- •
There are many anatomic variants of the hand arteries, specifically concerning the communicating arches between the radial and ulnar arteries.

Patient evaluation
Prior to the performance of the vascular study, there are certain questions that the examiner should ask the patient and specific physical observations that might help conduct the examination and arrive at a diagnosis. The first step is to ask the patient what his/her symptoms are:
- •
Is there pain, and if so, how long has it been present?
- •
Did the pain or discomfort come on suddenly or slowly?
- •
Is the pain constant or transient?
- •
What makes the pain or discomfort better or worse?
- •
Does exposure to cold or stressful situations bring on or intensify symptoms?
- •
Is there an arm or hand asymmetry?
- •
Are any fingers discolored?
- •
Is there a temperature difference between hands or finger(s)?
- •
Are there ulcers on the fingertips?
Because of the multiple etiologies of upper extremity arterial disease, consider:
- •
Talking to the patient:
- •
to assess the type and duration of symptoms
- •
- •
Examining the arms for:
- •
evidence of skin changes and differences in color
- •
differences in limb size
- •
The upper extremity arterial evaluation
Color Doppler and duplex ultrasound are used in conjunction with or following noninvasive physiologic testing. These tools include:
- 1.
Continuous-wave Doppler (with a recording device to display arterial waveforms)
- 2.
Pulse volume recordings (PVRs) and segmental pressures
- 3.
Photoplethysmographic (PPG) sensors to detect blood flow in the digits
One or all of these tools may be needed to diagnose a given problem. For instance, if fingers are cool and discolored with exposure to cold but fine otherwise, the examination will focus on the question of whether this is a vasospastic disorder (e.g., Raynaud disease) versus a situation where arterial obstructive disease is present. In some cases both might apply. An extensive diagnostic workup may be required. Close attention should be given to each finger (usually with PPGs), and then cold exposure may be required to provoke symptoms. If cold does not seem to be a factor, then a cold challenge may be omitted. If the problem is positional, a baseline PPG study should be done, followed by waveforms obtained with the arm in different positions. Finally, if nonimaging Doppler and PPG waveforms suggest arterial obstructive disease, duplex imaging can be done to identify the cause.
Obstructive Arterial Disease
Physiologic evaluation
For almost every situation where arterial disease is suspected in the upper extremity, the standard noninvasive starting point is the PVR combined with segmental pressure measurements ( Fig. 13.14 ). Continuous-wave Doppler signal assessment of the subclavian, axillary, brachial, radial, and ulnar arteries ( Fig. 13.15 ) is complementary to the segmental pressures and PVR information. This simple set of tests can answer the clinical question: Is hemodynamically significant arterial obstruction present in a major arm artery? If the fingers are symptomatic, PPGs (see Fig. 13.14B ) should be obtained from all digits.


The PVR and Doppler examinations are conducted as follows. Blood pressure cuffs are placed at the mid-portion of the upper arm and the forearm and PVR waveform recordings are taken at both levels. Then, the systolic blood pressure is measured at both levels, using the appearance of an audible Doppler signal during the release of the respective blood pressure cuffs. The Doppler signals are typically acquired at the radial artery. The measured blood pressures should be similar side to side, and from one level to the other (see Fig. 13.14A ). A blood pressure difference of more than 20 mm Hg between arms is a specific indicator of a hemodynamic significant lesion on the side with the lower pressure. A difference of 10 mm Hg has better sensitivity but lower specificity, whereas a difference of 15 mm Hg may be taken as a reasonable cut point. A difference of 20 mm Hg between levels in the same arm is believed to represent evidence of disease although there are no large studies to support this assertion. A pressure difference accompanied by an abnormal PVR ( Fig. 13.16 ) is highly indicative of the presence of significant disease although this combination of findings has poor sensitivity. The presence of a pressure difference between arms or between levels in the same arm may require additional testing to determine the cause, usually with Doppler ultrasound imaging.

If pressures and waveforms are normal, one can assume there is no clinically significant obstruction in the upper extremity arteries. This observation may be an appropriate stopping point, especially if the referring physician only needs to rule out major, limb-threatening disease or to make sure there is no inflow disease before coronary artery bypass surgery with the internal thoracic artery (a branch of the subclavian artery; see Fig. 13.1 ). It must be understood, however, that normal results of these indirect tests cannot rule out nonobstructive plaque or thrombus, aneurysm, transient mechanical compression of an artery segment, vasospasm, or other pathologies (such as arteritis). If any of these problems are suspected, additional testing may be required.
Color Doppler and duplex ultrasound imaging
Clinically significant atherosclerotic plaque preferentially develops in the proximal subclavian arteries and occasionally in the axillary arteries. The principal effect is blood flow reduction because of stenosis or occlusion that can result in arm ischemia. Atherosclerotic obstruction of more distal arteries, such as the brachial, radial, and ulnar arteries, is less common; nevertheless, distal arteries may occlude secondary to low-flow states or embolization.
Although stenosis of the proximal upper extremity arteries is most often caused by atherosclerosis, other pathologies include vasculitis, trauma, or thoracic outlet compression. A stenosis that reduces the lumen diameter by 50% or greater is considered blood flow reducing, or of hemodynamic significance. Such a stenosis is identified by an increase in PSVs ( Fig. 13.17 ), and, in the case of a severe stenosis or occlusion, by a damped (tardus-parvus) waveform distal to the level of a high-grade stenosis or occlusion, as shown in Fig. 13.18 . In addition, high-grade arterial stenosis or occlusion cause overall reduced blood flow velocities proximal to (upstream from) the point of obstruction ( Fig. 13.19 ). There are no universally accepted velocity cut points that determine the severity of a stenosis in the arm arteries; however, when a stenosis causes the PSV to double (compared with the prestenotic velocity), it is considered of hemodynamic significance (≥50% diameter narrowing). A more severe stenosis will further increase systolic and diastolic velocities.




Color Doppler imaging of a stenosis shows: (1) narrowing of the arterial lumen; (2) altered color flow signals (aliasing) at the stenosis consistent with elevated blood flow velocities; and (3) an altered poststenotic color flow pattern due to turbulent flow ( Fig. 13.20 ). With arterial occlusion, proximal Doppler waveforms show a high-resistance pattern often with decreased PSVs (see Fig. 13.19 ), no detectable flow in the occluded vessel lumen with color and power Doppler (see Fig. 13.18 ) or on Doppler spectral waveforms at the level of occlusion, and a damped, monophasic Doppler signal distal to the obstruction (see Fig. 13.18 ). When occlusion is detected, it is important to determine the extent of the occluded segment and the location of arterial reconstitution by collaterals (see Fig. 13.18 ).

Arterial thrombosis may occur distal to a critical stenosis or may result from embolization, trauma, or thoracic outlet compression. The result may be occlusion or partial occlusion. Thrombus or vasculitis can be visualized directly with gray-scale imaging, but color and power Doppler imaging are used to determine vessel patency and to assess the degree of vessel recanalization following thrombolysis.
If a patient has a significant difference in arm blood pressures (20 mm Hg, as observed during the segmental pressure/PVR portion of the study), the duplex imaging examination should be expanded to check for vertebral to subclavian steal. This is a situation where a tight stenosis or occlusion is present in the subclavian artery proximal to the origin of the vertebral artery (see Fig. 13.1 ). The pressure drop caused by the obstruction causes the subclavian artery to be supplied by the ipsilateral vertebral artery. Vertebral to subclavian steal can cause decreased blood flow to the affected arm, thus causing symptoms. For details concerning the pathophysiology of this condition and its clinical consequences, please see Chapter 9 .
Successful visualization of a proximal subclavian stenosis is more likely on the right side, as shown in Fig. 13.20 , than on the left because the right subclavian artery is a branch of the innominate artery and often has a good imaging window. The stenosis is generally seen in the most proximal segment of the subclavian artery, just beyond the bifurcation of the innominate artery into the right common carotid and subclavian arteries. Seeing a stenosis on the left side is very difficult because the subclavian artery arises directly from the aorta at an angle and depth that limit the imaging window. This is unfortunate, considering that approximately 75% of subclavian stenosis cases occur on the left side.