Asthma is an inflammatory disease characterized by increased airway reactivity and by airflow obstruction that is at least partially reversible and results in recurrent episodes of wheezing, breathlessness, and cough.
Etiology
Asthma can be divided into two main categories: extrinsic and intrinsic. Extrinsic asthma occurs in patients who are atopic, a term used to refer to the genetic predisposition to respond to antigenic challenge with excessive immunoglobulin E (IgE) production. The inheritance is complex but usually incomplete, and evidence of it is much greater if both parents are atopic. Although patients with extrinsic asthma are invariably atopic, atopy itself is not synonymous with asthma. Atopy occurs in more than 30% of the population, whereas the incidence of asthma is generally less than 10%. In addition to atopy and elevated blood levels of IgE, extrinsic asthma is characterized by high incidences of eczema and rhinitis, onset during the first 3 decades of life, seasonal symptoms, and a tendency for remission in later life. Intrinsic asthma occurs in patients in whom atopy or specific external triggers of bronchoconstriction cannot be identified. Affected patients are characterized by being older than patients with extrinsic disease and by having no or a less convincing family history of asthma or atopy, an absence of elevated blood levels of IgE or positive skin or bronchial response to allergen challenge, increased numbers of blood and sputum eosinophils, decreased responsiveness to therapy, and a tendency to persistent and progressive disease resulting in fixed airflow obstruction.
Prevalence and Epidemiology
Asthma is a common disease, and there is good evidence that its prevalence and the prevalence of other allergic disorders is increasing worldwide. The reasons for this increase are unclear. Estimates of prevalence vary by definition, geography, ethnicity, and age. The prevalence of asthma in most countries with available statistics ranges from approximately 5% to 25% in children and 2% to 12% in adults. The highest prevalences are found in the United Kingdom, Australia, and New Zealand (≈12% each) and in Tristan da Cunha, a group of remote islands in the South Atlantic Ocean in which 56% of the population has asthma. Concomitant sinusitis is common, occurring in 47% to 76% of asthma cases.
The prevalence of asthma is highest in childhood and decreases during adolescence and adulthood. The prevalence before the age of 10 years is higher in boys than in girls; after that, it is higher in females. Females are also more likely to visit the emergency department and to be admitted for acute severe asthma.
Asthma is the most common chronic lung disease and an important health problem worldwide. In the United States, it accounts for nearly 2 million emergency department visits, 500,000 hospitalizations, and 5000 deaths each year. Data from Australia, Canada, and Spain indicate that acute asthma accounts for 1% to 12% of all adult emergency department visits. In a study in France, 7% of adult patients with acute asthma who presented to the emergency department were transferred to an intensive care unit.
Clinical Presentation
The diagnosis of asthma is based largely on a history of periodic paroxysms of dyspnea, alternating with intervals of complete or nearly complete remission. Cough can be a prominent symptom and occasionally the only symptom. The onset of acute asthma (asthma attack) is characterized by gradual increase in shortness of breath, cough, and wheezing and by a decrease in expiratory airflow. The exacerbations may progress during hours, days, or weeks. Physical findings include hyperventilation, inspiratory and expiratory rhonchi and wheezes, decreased breath sounds, and prolonged expiration. Cough and wheezing are the result of bronchial inflammation and bronchoconstriction. Contraction of airway smooth muscle, edema, and hypersecretion also affect the bronchioles and result in small airway closure. To compensate, the patient breathes at a higher lung volume to increase outward retraction of the airways, thereby helping to maintain airway patency. The more severe the airflow limitation, the greater the tendency for airway closure to occur and the higher the lung volume must be to keep airways open. The combination of hyperinflation and airflow limitation markedly increases the work of breathing.
Acute asthma attacks may range from mild to life-threatening. In a study of 3772 patients with acute asthma who presented at various emergency departments in France, 975 (26%) had life-threatening attacks, 1834 (49%) had severe exacerbations without life-threatening features, and 963 (26%) had mild to moderate exacerbations. The overall admission rate was 54%, and mean hospital stay was 6 days. Three patients died in the hospital.
Pathophysiology
The basic pathophysiologic abnormality that determines the functional and symptomatic status of an asthmatic patient is airway narrowing, which can occur by four mechanisms: (1) airway smooth muscle contraction, (2) edema and congestion of the airway wall, (3) plugging of the airway lumen by mucous and inflammatory exudate, and (4) airway wall remodeling. Airway remodeling is a heterogeneous process leading to changes in connective tissue deposition and to altered airways structure. For the most part, it is difficult to determine in a given patient what proportion of airway obstruction is caused by each of these mechanisms. However, it may reasonably be concluded that when obstruction is rapidly reversible after the inhalation of smooth muscle relaxants, the pathogenesis is smooth muscle contraction. On the other hand, when obstruction responds during a period of days to steroids and other therapeutic interventions, it is probably caused predominantly by edema and mucous plugging.
Asthma is a chronic inflammatory disorder of the airways associated with airway hyperresponsiveness, an exaggerated bronchoconstrictor response to a wide variety of exogenous and endogenous stimuli that results in acute episodes of dyspnea and wheezing. These include environmental allergens, respiratory viral infections, exercise, analgesics, air pollution, weather changes, cigarette smoke, occupational sensitizing agents, indoor allergens, and irritants, such as household sprays and paint fumes. Specific antigens can provoke asthmatic attacks in sensitized persons. These individuals frequently suffer from other allergic manifestations, such as hay fever and eczema. Potential antigens are innumerable.
Exercise-induced asthma can be considered to be present when airway narrowing accompanies moderate or vigorous exercise. Rather than being a separate form of asthma, exercise-induced asthma should be considered a trigger for airway narrowing in patients who have asthma. In fact, it occurs in 70% to 80% of patients with asthma who exercise at 80% to 90% of their maximal workload for 6 to 8 minutes.
The association of asthma and gastroesophageal reflux is common; various investigators have estimated the concordance to be 30% to more than 80%. There is evidence that gastroesophageal reflux can induce asthma and that asthma can cause a worsening of gastroesophageal reflux. It is possible that gastroesophageal reflux triggers airway narrowing in susceptible persons by reflex bronchoconstriction secondary to stimulation of afferent nerves in the esophagus or pharynx or by direct aspiration of a small amount of esophageal contents.
Pathology
On histologic examination, asthma is characterized by the presence of chronic inflammation of the airways that involves mainly the medium-sized and small bronchi. The bronchi are thickened because of a combination of edema and an increase in smooth muscle and in the size of the mucous glands ( Fig. 58.1 ). Bronchiolar abnormalities include wall thickening, mucostasis, and constrictive bronchiolitis ( Fig. 58.2 ). Between clinical episodes, the bronchioles may be nearly normal, as viewed in tissue from asthmatics taken for other reasons.


Histologic changes in the bronchial and bronchiolar walls involve the epithelium, lamina propria, muscularis mucosae, and submucosa. The constellation of abnormalities is referred to as airway wall remodeling and consists of changes in the composition, quantity, and organization of the cellular and molecular constituents of the airway wall as a consequence of chronic injury and repair. Collagen deposition in the subepithelial layer, as well as in the adventitia, may underlie the decreased airway distensibility that may be seen in asthmatic patients. An increase in smooth muscle is also a characteristic feature; it is the result of both hyperplasia and hypertrophy and is most pronounced in subjects who die of the disease. Eosinophils are the most characteristic and numerous inflammatory cells in the airway wall; however, there may also be increases in lymphocytes, macrophages, neutrophils, and mast cells.
Lung Function
Measurements of airflow limitation, its reversibility, and its variability are important in the diagnosis and management of asthma. The main measurements used for the evaluation of these patients are forced expiratory volume in 1 second (FEV1), forced vital capacity, the ratio of FEV1 to forced vital capacity, and peak expiratory flow. A 12% or greater improvement in FEV1 or 15% or greater improvement in peak expiratory flow spontaneously, after inhalation of a bronchodilator, or in response to a trial of glucocorticosteroid therapy favors a diagnosis of asthma.
Diffuse airway narrowing is the basic functional abnormality of symptomatic asthma; the resulting increase in resistance leads to decreased flow, hyperinflation, gas trapping, and ultimately an increase in the work of breathing. It is most easily detected and quantified by measurements of maximal expiratory flow. The increase in airway resistance is also associated with hyperinflation, as manifested by an increase in functional residual capacity and, to a lesser extent, total lung capacity.
As an asthmatic episode resolves, there is improvement in expiratory flow (peak expiratory flow and FEV1) and vital capacity and a decrease in functional residual capacity. The single-breath diffusing lung capacity for carbon monoxide is often elevated in both stable and acute asthma. The most plausible explanation for this apparent paradox is the transient increase in pulmonary capillary blood volume that is a result of the more negative inspiratory intrathoracic pressure secondary to obstruction of the airways.
Most patients experiencing an acute attack have some degree of hypoxemia as a result of ventilation-perfusion mismatch. There is not a close relationship between measures of airway obstruction and gas exchange in asthma. However, in severe acute attacks, partial pressure of oxygen in arterial blood generally drops to less than 60 mm Hg, FEV1 is less than 1 L, and peak flow is less than 60 L/min. As the severity and duration of obstruction increase, patients become exhausted, their respiratory muscles fatigue, and values of partial pressure of carbon dioxide in arterial blood rise into the hypercapnic range.
Manifestations of the Disease
Radiography
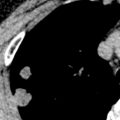
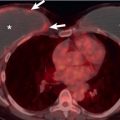
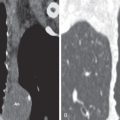
The most common radiographic abnormalities in patients who have asthma are hyperinflation and bronchial wall thickening ( Figs. 58.3 and 58.4 ); less frequent manifestations are prominence of the hila, increased central lung markings, and peripheral oligemia ( Fig. 58.5 ). The prevalence of these abnormalities is influenced by several factors, including the age at onset, the severity of asthma, and the presence of other diseases or complications of asthma.



Pulmonary hyperinflation is manifested as an increase in the depth of the retrosternal space, an increase in lung height, and flattening of the diaphragm (see Fig. 58.3 ). Thickening of the airways occurs in both segmental and subsegmental bronchi and can be seen either as ring shadows viewed end-on or as “tram-line” opacities viewed en face . Prominence of the main pulmonary artery and its hilar branches with rapid tapering is indicative of transient precapillary pulmonary arterial hypertension secondary to hypoxia. Additional vascular findings include diffuse narrowing and blood flow redistribution into the upper lobes, the latter in the absence of other signs of postcapillary hypertension, and a paucity of vessels in the outer 2 to 4 cm of the lungs.
Despite the observations just outlined, the chest radiograph has a limited role in the diagnosis of asthma. It is often normal, even during an acute attack; moreover, when it is abnormal, the findings are nonspecific. The two main indications for chest radiography are to exclude other conditions that cause wheezing—particularly emphysema, left-sided heart failure, and obstruction of the trachea or major bronchi by tumor or foreign body—and to identify complications. Complications of asthma that may be seen on radiography or computed tomography (CT) include pneumonia, atelectasis ( Fig. 58.6 ), pneumomediastinum ( Fig. 58.7 ), pneumothorax, and occasionally pneumorrhachis (i.e., air within the spinal canal).