Presentation and Presenting Images
A 47-year-old female whose Gail model risk assessment estimates her 5-year risk for breast cancer is 1.7% and her lifetime risk is 16.7%. presents for routine screening mammography.
75.2 Key Images
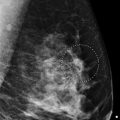
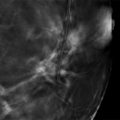
( ▶ Fig. 75.3)
75.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
75.2.2 Imaging Findings
The imaging of the right breast is normal (not shown). There is an asymmetry (circle) seen in the craniocaudal (CC) view only in the lateral aspect of the left breast ( ▶ Fig. 75.3). There is no comparison imaging.
75.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
75.4 Diagnostic Images
75.4.1 Imaging Findings
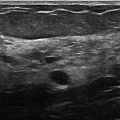
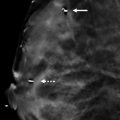
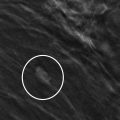
A repeat left CC view with adequate compression and a left CC digital breast tomosynthesis (DBT) image demonstrate normal breast tissue without an associated mass lesion ( ▶ Fig. 75.4 and ▶ Fig. 75.5). Ultrasound was performed (not shown) and demonstrated normal fibroglandular tissue, confirming benignity.
75.5 BI-RADS Classification and Action
Category 2: Benign
75.6 Differential Diagnosis
Overlapping parenchyma or summation artifact: DBT obtained at the diagnostic evaluation demonstrated that this asymmetry is created by overlapping tissue.
Breast cancer: Breast cancer may present as asymmetry; however, this finding did not persist on tomosynthesis imaging. Suspicious findings would be confirmed on sonography.
Fibrocystic changes: Fibrocystic changes may present as an asymmetry on mammography. The ultrasound was negative and did not reveal any cysts or changes of fibrocystic disease.
75.7 Essential Facts
This finding was the result of a summation artifact secondary to a lack of compression. Attention to proper technique with adequate compression can avoid recalls for pseudolesions.
A pseudolesion may be misinterpreted as a true lesion and lead to a biopsy.
The combination of conventional mammography and DBT improves the diagnostic performance, reduces recall rates, and increases cancer detection.
The Gail model estimates the risk of developing breast cancer over the next 5 years and over a lifetime. A 5-year risk of 1.7% or higher means there is an increased risk of developing breast cancer.
This patient is at increased risk of developing breast cancer in the next 5 years and has a lifetime risk of 16.7%.
75.8 Management and Digital Breast Tomosynthesis Principles
Rather than depending on the high likelihood that a one-view finding is a false-positive, radiologists should determine which asymmetries may have clinical significance.
Asymmetries associated with clinical findings, architectural distortion, or calcifications are of likely clinical significance and warrant further imaging evaluation and/or biopsy.
Asymmetries seen with DBT may be biopsied using tomosynthesis-directed stereotactic-guided biopsy.
Since early-stage breast cancer can have a subtle presentation, radiologists must consistently and carefully scrutinize mammograms to detect early breast cancer.
75.9 Further Reading
[1] Brenner RJ. Asymmetric densities of the breast: strategies for imaging evaluation. Semin Roentgenol. 2001; 36(3): 201‐216 PubMed
[2] Giess CS, Frost EP, Birdwell RL. Interpreting one-view mammographic findings: minimizing callbacks while maximizing cancer detection. Radiographics. 2014; 34(4): 928‐940 PubMed

Fig. 75.1 Left craniocaudal (LLC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree