Atelectasis is defined as less than normal inflation of all or part of the lung with a corresponding diminution in lung volume. Although the term collapse is often used synonymously with atelectasis, it should be reserved for complete atelectasis.
Mechanisms of Atelectasis
Mechanisms of atelectasis can be classified into five types: obstructive (resorptive), passive, compressive, adhesive, and cicatrization (scar).
Obstructive Atelectasis
Obstructive or resorptive atelectasis occurs when airflow to a region of lung is interrupted as a result of airway obstruction ( Fig. 3.1 ). As oxygen is resorbed, alveoli decrease in volume, with their pressure remaining atmospheric. Consequently, the partial pressure of carbon dioxide and nitrogen in the alveoli rises relative to capillary blood, and both gases diffuse into blood to maintain equilibrium. Thus alveolar volume is further reduced, with a consequent rise in the alveolar-capillary blood P o 2 gradient; oxygen diffuses into capillary blood, and the cycle is repeated until all alveolar gas is absorbed. In healthy lungs breathing atmospheric air, complete air absorption occurs within 24 hours. In intubated patients breathing a high concentration of inspired oxygen, complete air absorption often occurs within an hour. The end result of such airway obstruction is complete collapse of the involved lobe or lung unless, as is often the case, pneumonitis develops distal to the obstruction. O bstructive pneumonitis (e.g., distal to pulmonary carcinoma) frequently leads to consolidation severe enough to limit loss of volume; this condition is often referred to as “drowned lung.” The characteristic radiographic picture of obstructive pneumonitis (i.e., homogeneous opacification of a segment, lobe, or lung without air bronchograms) is highly suggestive of an obstructing endobronchial lesion.

Computed tomography (CT) often provides valuable additional information in patients with obstructive atelectasis, particularly with regard to the precise location and extent of the obstructing process (see Fig. 3.1 ). CT performed after the administration of intravenous contrast material may distinguish a proximal obstructing tumor from collapsed lung or adjacent mediastinal structures. In some patients, magnetic resonance imaging (MRI) or positron emission tomography (PET) can provide comparable or complementary information by depicting the mass and adjacent collapsed lung.
Passive Atelectasis
Passive atelectasis denotes loss of volume as the lung retracts in the presence of pneumothorax ( Fig. 3.2 ). The lung has a natural tendency to collapse and does so when removed from the chest. While the lungs are in the thoracic cavity, this tendency is opposed by the chest wall. At the resting respiratory position (functional residual capacity), the tendency for the lung to collapse and the chest wall to expand is equal and opposite. In the presence of pneumothorax the lung retracts and its volume decreases. Provided that the pleural space is free (i.e., without adhesions), atelectasis of any portion of lung is proportional to the amount of air in the adjacent pleural space. As the lung shrinks adjacent to a pneumothorax, its density does not increase appreciably until it is almost completely collapsed. This presumably occurs because the reduction in lung volume is approximately balanced by a reduction in blood content and accounts for the difficulty commonly experienced in identifying the lung edge in cases of small or moderate spontaneous pneumothorax.

Compressive Atelectasis
Compressive atelectasis (also called relaxation atelectasis by some radiologists) results from compression of the lung by an adjacent space-occupying process. Any intrathoracic space-occupying process, such as a bronchogenic cyst, bulla, neoplasm, pleural effusion, or large osteophyte, induces airlessness of a thin layer of contiguous lung parenchyma ( Fig. 3.3 ).

On CT atelectasis is seen commonly in the dependent lung regions as an ill-defined area of increased attenuation or subpleural curvilinear opacities ( Fig. 3.4 ). The former measures from a few millimeters to 1 cm or more in thickness and has been called dependent opacity or dependent density. Subpleural curvilinear opacities, also known as subpleural lines, are linear areas of increased attenuation measuring several centimeters in length and located within 1 cm of the pleura and parallel to it. Both manifestations of dependent atelectasis characteristically disappear when the patient changes position; differentiation of dependent atelectasis from true interstitial or airspace disease can be established easily by scanning the patient in the supine and prone positions (see Fig. 3.4 ).

Round Atelectasis
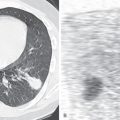
Round atelectasis (also called rounded atelectasis) is a distinct form of atelectasis characteristically associated with focal pleural thickening. The majority of cases of round atelectasis are seen in patients exposed to asbestos. Other causes include pleural effusion or thickening from tuberculosis, infections other than tuberculosis, pulmonary infarction, left heart failure, hemothorax, surgery (mainly cardiac surgery), and malignant tumor. On conventional radiographs round atelectasis is seen as a fairly homogeneous round, oval, wedge-shaped, or irregularly shaped mass in the peripheral lung adjacent to thickened pleura ( Fig. 3.5 ). It usually measures 3 to 6 cm in greatest diameter, although it may involve an entire lobe, and is associated with loss of volume of the affected lobe. The bronchi and vessels in the vicinity of the mass are gathered together in a curvilinear fashion as they pass toward the mass, similar to the tail of a comet (comet tail sign), a feature best appreciated on CT. The abnormality occurs most commonly in the lower lobes.

The characteristic CT features consist of bronchi and vessels curving and converging toward a round or oval mass that abuts an area of pleural thickening and is associated with evidence of volume loss in the affected lobe; vessels and bronchi curve into the periphery of the mass, which forms the basis for the comet tail sign ( Fig. 3.6 ). The hilar (central) aspect of the mass usually has indistinct margins as a result of blurring by the entering vessels. Air bronchograms are identified within the mass in approximately 60% of cases. Hypertrophy of extrapleural fat may be identified adjacent to the mass, a feature that reflects chronicity and is therefore not seen in all cases.

In most patients the CT findings are sufficiently characteristic that neither biopsy nor further investigative procedures are necessary to exclude more ominous disease. 18 F-fluorodeoxyglucose (FDG) PET usually shows little or no uptake (i.e., uptake equal to or less than mediastinal blood pool) and may be helpful in distinguishing round atelectasis from carcinoma in confusing cases. Follow-up of patients who have round atelectasis has shown that the majority of lesions are stable for many years. Occasionally, a lesion decreases in size, resolves within a few weeks to several years, or enlarges. Needle biopsy may rarely be required to rule out carcinoma.
Adhesive Atelectasis
The term adhesive atelectasis is used to describe atelectasis caused, at least in part, by deficiency of surfactant. Surfactant reduces the surface tension of the alveoli as their surface area or volume decreases; thus the critical closing pressure of alveoli occurs at a lower volume and distending pressure, thereby effectively protecting against collapse. Causes of adhesive atelectasis in adults include radiation pneumonitis, smoke inhalation injury, acute respiratory distress syndrome, and pulmonary thromboembolism. Atelectasis in radiation pneumonitis is usually limited to the irradiated portions of the lungs; occasionally, it is seen outside the regions of the radiation ports, particularly on CT. The radiographic and CT findings consist of areas of ground-glass opacification or consolidation with associated loss of volume ( Fig. 3.7 ). The radiologic manifestations of radiation pneumonitis usually occur approximately 1 to 6 months after the completion of radiation therapy. Focal ischemia distal to pulmonary thromboembolism may lead to a local reduction in surfactant that results in subsegmental, segmental, or, less commonly, lobar atelectasis.

Atelectasis, particularly of the left lower lobe, is seen in the majority of patients after cardiac surgery. It is likely that adhesive atelectasis also plays a part in loss of volume postoperatively and accounts for the marked arteriovenous shunting that may occur even when the chest radiograph is relatively normal.
Cicatrization Atelectasis
Although for the sake of completeness we have included loss of volume associated with pulmonary fibrosis in the section on atelectasis, the term atelectasis is seldom used in this context. The fundamental pathologic process is one of fibrosis, the fibrous tissue undergoing retraction as it matures and resulting in loss of volume of the affected portion of lung. The fibrosis may be localized, best exemplified by long-standing tuberculosis and radiation fibrosis (see Fig. 3.7 ), or diffuse, as seen in idiopathic pulmonary fibrosis.
The bronchi and bronchioles within the affected lung are dilated because of the increased elastic recoil from the surrounding pulmonary fibrosis, a phenomenon known as traction bronchiectasis and bronchiolectasis (see Fig. 3.7 ). The radiologic signs are as might be expected: a segment or lobe occupying a volume smaller than normal with a density rendered inhomogeneous by dilated, air-containing bronchi and with irregular thickened strands extending from the atelectatic segment to the hilum. Compensatory signs of chronic loss of volume are usually evident and include local mediastinal shift (frequently manifested by a marked deviation of the trachea when segments of the upper lobe are involved), displacement of the hilum (which may be severe in upper lobe disease), and compensatory overinflation of the remainder of the affected lung.
- •
Obstructive atelectasis
- •
Distal to obstruction of a bronchus
- •
- •
Passive atelectasis
- •
Retraction of lung in the presence of pneumothorax
- •
- •
Compressive atelectasis
- •
Compression by a space-occupying process, such as a pleural effusion, pulmonary mass, or bulla
- •
- •
Adhesive atelectasis
- •
Caused by deficiency of surfactant (e.g., radiation pneumonitis)
- •
- •
Cicatrization atelectasis
- •
Caused by contraction of fibrous tissue as it matures; can be focal (e.g., tuberculosis) or diffuse (e.g., idiopathic pulmonary fibrosis)
- •
Radiologic Signs of Atelectasis
The radiologic manifestations of atelectasis may be classified into direct and indirect signs. Direct signs include displacement of the interlobar fissures and crowding of bronchi and vessels within the area of atelectasis; indirect signs include pulmonary opacification and signs related to shift of other structures to compensate for the loss of volume ( Fig. 3.8 ).

Direct Signs
Displacement of Interlobar Fissures
Displacement of the fissures that form the boundary of an atelectatic lobe is one of the most dependable and easily recognized signs of atelectasis (see Fig. 3.8 ). For each lobe the position and configuration of the displaced fissures are predictable for a given loss of volume; these factors are considered later in relation to specific patterns of lobar and segmental atelectasis.
Crowding of Vessels and Bronchi
As the lung loses volume the vessels and bronchi in the atelectatic area become crowded together. This finding is one of the earliest signs of atelectasis and can be recognized most readily when comparison is made with previous radiographs. Increased opacification of the atelectatic lobe may result in obscuration of the vessels; however, except in patients who have obstructive atelectasis, crowded air bronchograms are visible within the area of atelectasis on radiographs or CT.
Indirect Signs
Apart from the presence of increased opacity, the main indirect radiologic signs of atelectasis include mechanisms that compensate for the reduction in pleural pressure, such as diaphragmatic elevation, mediastinal shift, hilar displacement, and overinflation of the remainder of the lung (see Fig. 3.8 ). The more acute the atelectasis, the greater the predominance of diaphragmatic and mediastinal displacement; the more chronic the atelectasis, the more that compensatory overinflation of nonatelectatic lung predominates.
- •
Direct
- •
Displacement of interlobar fissures
- •
Crowding of vessels and bronchi
- •
- •
Indirect
- •
Local increase in opacity
- •
Elevation of the hemidiaphragm
- •
Shift of the mediastinum
- •
Compensatory overinflation of remaining lung
- •
Displacement of the hila
- •
The local increase in opacity results from a combination of resorption of air and accumulation of fluid. The volume of an airless lobe or segment depends not only on which order of bronchus is obstructed but also on the amount of sequestered fluid within the obstructed parenchyma. Because the lung contains a large amount of air and normal lung density is only 0.12 g/mL, the lung must become almost completely collapsed before increased opacification from loss of volume is apparent on the chest radiograph.
Elevation of the hemidiaphragm is more marked in lower than in upper lobe atelectasis. In the lower lung zones, elevation tends to occur in the area contiguous to the lobe involved—posterior elevation in lower lobe atelectasis and anterior elevation in middle lobe or lingular atelectasis, although, in the latter two situations the diaphragmatic displacement is seldom severe.
When assessing diaphragmatic elevation, it is important to be aware of possible variations in the relationship of the two hemidiaphragms. Although the right dome is normally 1 to 2 cm higher than the left, in approximately 10% of normal subjects the two hemidiaphragms are at the same level, and in 2% the right hemidiaphragm is more than 3 cm higher than the left.
The anterior and middle mediastinal compartments are more mobile than the posterior compartment and therefore shift to a greater extent in patients with atelectasis.
Overinflation of the remainder of the ipsilateral lung is one of the most important and reliable indirect signs of atelectasis. It seldom occurs rapidly and, in the early stages of lobar atelectasis, is usually of less diagnostic help than the other compensatory phenomena, such as diaphragmatic elevation and mediastinal displacement. As the period of atelectasis lengthens, however, overinflation becomes more severe and the diaphragmatic and mediastinal changes regress.
When an entire lung becomes atelectatic after obstruction of a main bronchus, the resultant loss of volume of the hemithorax must be compensated for largely by overinflation of the contralateral lung ( Fig. 3.9 ). In this situation the mediastinal shift may be large; because the mediastinum is less stable anteriorly than elsewhere, the anterior septum is rotated laterally and posteriorly, the normal lung overinflating to such an extent that it occupies the whole anterior portion of the thorax. Thus the heart and the collapsed lung are displaced into the posterior portion of the ipsilateral hemithorax.