20
Atherosclerotic Disease of the Aorta, Pelvis, and Lower Extremities
Diagnostic arteriography for atherosclerotic disease of the aorta, pelvis, and lower extremities is performed after the decision to treat has been made. Clinical history and noninvasive studies that precede the angiogram almost always can make the diagnosis of chronic atherosclerotic occlusive disease and often will be able to define the levels at which critical stenoses occur. The purpose of the angiogram is to define specifically the anatomy to plan interventional or surgical therapy. Multiple views are often necessary to define the anatomy clearly (Fig. 20-1). Thus, a thorough knowledge of potential available therapies is important to obtain an adequate study.
Traditional vascular surgical techniques require that three things be defined. The first is the status of the “inflow,” that is, the arteries upstream of the target lesion. (Because atheroocclusive disease is almost always infrarenal, the infrarenal aorta and the common iliac and external iliac arteries serve as the inflow for the infrainguinal arteries, as an example.) The second is the status of the “outflow,” the vascular segment or segments downstream of the occlusive lesion. (For example, for popliteal occlusion at Hunter’s canal, the outflow is the popliteal artery and trifurcation vessels.) These two vessel sets define where the proximal anastomosis and distal anastomosis of a bypass graft are placed. The third parameter is the type of conduit, for example, autologous vein versus polytetrafluoroethylene (PTFE). Synthetic conduits are used exclusively in the aortoiliac distribution, whereas an autologous vein is much preferred for bypass to the tibial and pedal vessels. For femoropopliteal bypass grafts, if vein is available, most vascular surgeons will use it, especially if the graft has to cross the knee joint; otherwise, PTFE is used (surgical bypasses are usually named by their proximal and distal anastomoses; see Table 20-1.)
 Chronic Occlusive Disease
Chronic Occlusive Disease
Arteriosclerosis obliterans
Arteriosclerosis is a chronic disease that is progressive and usually symmetric. Patients present with gradual onset or worsening of symptoms. Most patients with arteriosclerosis obliterans present with claudication. Risk factors for arteriosclerosis obliterans include advanced age, hypertension, smoking, diabetes, hypercholesterolemia, hypertriglyceridemia, and male sex. In the United States, the most commonly accepted categorization of chronic limb ischemia is the Rutherford Criteria, which is listed in Table 20-2.1
Rutherford criteria
Category 0
Asymptomatic patients in this category include those with occlusive disease and congenital variants. The dorsal pedal pulse can be absent in about 12% of patients, although the posterior tibial pulse is rarely absent in normal patients. Asymmetric pulse decrement alone is not an indication for intervention in chronic disease.
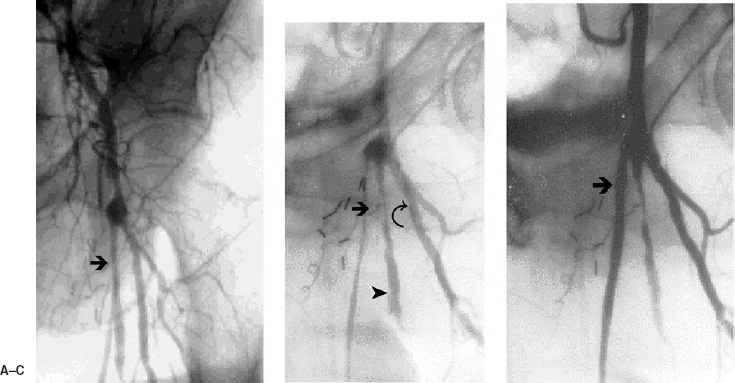
FIGURE 20-1. (A). An arteriogram was performed to evaluate a failing left common femoral to peroneal artery vein graft. The proximal portion of the graft is not seen secondary to the overlapping superficial femoral artery (arrow). (B). An oblique view demonstrates severe narrowing of the proximal portion of the vein graft (straight arrow). The superficial femoral artery (arrowhead) is seen better; the left deep femoral artery is visualized (curved arrow). (C). After balloon angioplasty of the proximal graft, flow and lumenal patency (arrow) are improved.
Categories 1–3
Patients with intermittent claudication usually have single-segment stenosis or occlusion (80% of cases). In these patients, the level of claudication usually develops distal to the level of stenosis. Claudication is a reproducible pain or soreness brought on by a defined amount of exercise and relieved by rest. (The term is derived from (Latin “to limp,” after the Roman Emperor Claudius, who limped across Europe as his armies conquered the continent). These patients usually should be treated conservatively. Claudication must be differentiated from pseudoclaudication caused by spinal stenosis. Pseudoclaudication presents with variable onset relieved by a change in position and with normal peripheral pulses. Claudication and pseudoclaudication can coexist. The prevalence of intermittent claudication increases with age and is present in 3% of the population under 60 years of age and in 20% of the population older than 75 years of age. It is relatively stable in 60% of patients, with 15% actually improving with conservative therapy such as exercise and cessation of smoking. Twenty-five percent of claudicators progress to critical ischemia. Amputation is done in only 5to 6% of patients within 10 years of presentation of peripheral vascular disease (PVD); the amputation rate is higher in smokers and diabetics. Intervention should be reserved for patients with debilitating or lifestyle-limiting claudication and for patients with critical ischemia. Itis important to remember that claudication is a marker for coronary artery disease, which is prevalent in nearly all PVD patients.
| Operation | Indication1 |
| Aortoaortic bypass | Abdominal aortic aneurysm, without iliac extension |
| Aortoiliac bypass | Abdominal aortic aneurysm extending to common iliac arteries |
| Aorto bifemoral bypass | Aortoiliac occlusive disease involving both iliac arteries |
| Femoral–femoral bypass (“cross-femoral” bypass) | Unilateral severe iliac disease ipsilateral to symptoms; needs intact donor iliac artery contralateral to symptomatic side |
| Axillofemoral bypass | Used in high-risk patients with bilateral severe iliac disease; generally, axillary artery to femoral artery bypass (ipsilateral side), combined with cross-femoral bypass |
| Femoropopliteal bypass | Long-segment superficial femoral artery stenosis/occlusion; typically, common femoral artery serves as proximal anastomosis |
| Femorotibial bypass (“fem-distal” bypass) | Combined superficial femoral and popliteal artery stenosis/occlusion; occlusive disease frequently extends into proximal/midtibial arteries |
| Profundaplasty | Surgical revision of focal profunda femoris origin stenosis; often done in conjunction with femoropopliteal bypass |
| Iliac endarterectomy | Rarely used |
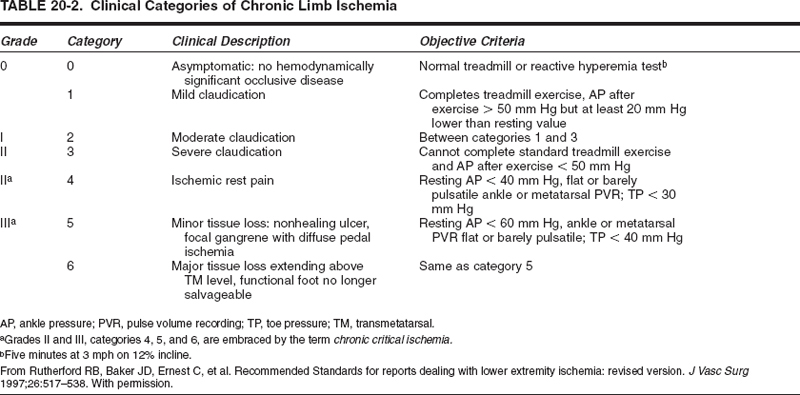
Categories 4–6
Patients with critical ischemia have a threatened extremity that requires intervention. Diagnostic studies such as angiography should be performed to plan treatment. Percutaneous and surgical interventions generally are directed at restoring continuous or “straight-line” flow to the foot. The purpose of such intervention is to maintain a functional foot and allow ambulation. Critically ischemic patients usually have multilevel occlusive disease. Symptoms from perfusion deficit develop in the end organ, that is, the skin of the foot. Ischemic rest pain (category 4) usually develops in the forefoot because 12/16/2010 resting-limb blood flow is insufficient to meet basal metabolic demand, causing pain in the cutaneous nerves. It is often nocturnal, aggravated by elevation and relieved by dependency. Dependent rubor is characteristic.
Category 5 patients present with ischemic ulcers. The lesions usually are located distally on the toes, but they also may be noted on the malleoli or shins. They may result from minor trauma that fails to heal secondary to chronically inadequate circulation. In diabetics, peripheral neuropathy allows repeated minor trauma, for example, from ill fitting shoes, to persist without being noted by the patient. Superimposed infection can put the limb at risk; gangrene may develop. These patients need to be treated aggressively. A limb with major tissue loss (category 6) does not have a salvageable foot; however, an angiogram and intervention may be indicated to preserve as much of the lower limb as possible because amputation sites may not heal in the face of vascular insufficiency.
Angiographic findings
Atherosclerotic plaque is usually irregular and eccentric but may also be smooth and concentric (Fig. 20-2). Plaques may be ulcerated. Rarely, they are weblike. Collateral development is the hallmark of chronic arterial occlusive disease, developing over time (weeks to months) (Fig. 20-3). Collateral arteries can partially compensate for occlusion of major vessels. Acute occlusion of normal vessels generally yields rapid, profound, limb-threatening ischemia. This typically occurs with trauma or arterial emboli in young patients. In patients with underlying occlusive disease, chronic collaterals may reduce the effect of an acute occlusion. (Fig. 20-4).
PVD can occur in focal and diffuse patterns. A critical stenosis can undergo in situ thrombosis and convert to a total occlusion. A superior convex meniscus usually marks the proximal edge of the thrombosis. The occurrence of acute in situ thrombosis may be marked by a sudden increase in the level of symptoms, for example, sudden progression from claudication to rest pain or by new onset claudication. With time, there is retrograde propagation to the nearest large collateral and organization of the thrombus by fibrin.
Arteriosclerosis obliterans is progressive and generally symmetric (Fig. 20-5). Significant atherosclerosis of the abdominal aorta is usually infrarenal. In adult patients, the adductor canal is usually the site of earliest plaque. In young patients with a smoking history who develop premature PVD, aortoiliac disease may be manifest first. The Leriche syndrome occurs in men and is characterized by absent or severely diminished femoral pulses, thigh and buttock claudication, and impotence. Anatomically, the Leriche syndrome consists of severe atherosclerotic narrowing of the distal aorta and common iliac arteries. Nonsmoking diabetic patients generally develop occlusions of the tibioperoneal arteries in addition to femoropopliteal lesions; aortoiliac involvement is seen much less frequently. Thus, diabetic patients presenting for limb salvage will have multilevel disease, which is generally infrainguinal and more difficult to treat than disease in the larger, more proximal vessels (Fig. 20-6).
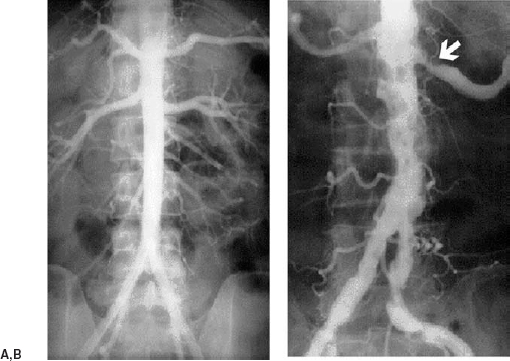
FIGURE 20-2. (A). Normal aortogram is seen. Note the smooth contour and slight tapering distally. (B). Aortogram demonstrating severe aortoiliac atherosclerosis. There also is a proximal left renal artery stenosis (straight arrow).
Lower-extremity ischemia has a differential diagnosis that is extensive and includes arteriosclerosis obliterans, thromboembolic disease, dissection, thrombosis of an aneurysm, and in situ thrombosis. Classically, patients with the “blue toe” syndrome present with ischemic toes with intact pedal pulses. This disease is due to cholesterol microembolization from aortic, iliac, and femoral artery plaques. Angiography is performed to find the source. Blue toe syndrome may be treated by angioplasty stents, atherectomy, or surgical means.
Treatment for chronic atheroocclusive disease
As noted, patients with claudication usually should be treated by managing risk factors such as hyperlipidimia and smoking; an exercise program in which walking through claudication is probably of value. In patients with critical limb ischemia (Rutherford categories 4 to 6), however, intervention is indicated. Control of pain and infection related to the ischemic limb and optimization of cardiorespiratory function are important. The primary aim of endovascular or open surgical techniques is relief of rest pain and healing of ischemic skin lesions. The choice between a percutaneous interventional procedure and open surgery generally depends on the exact level and extent of the obstructive disease. In a large series of limb salvage patients, about one third underwent angioplasty alone or angioplasty combined with open surgery to treat multisegment disease.2
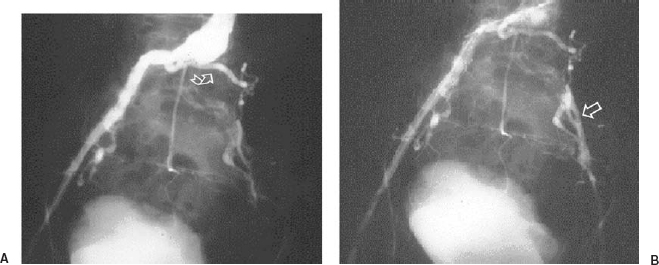
FIGURE 20-3. (A). An early phase of a pelvic arteriogram. There is diffuse narrowing of the right common and external iliac artery. The left common iliac artery is occluded, and an L4 collateral (curved arrow) is noted. (B). Reconstitution of the external iliac artery (arrow).
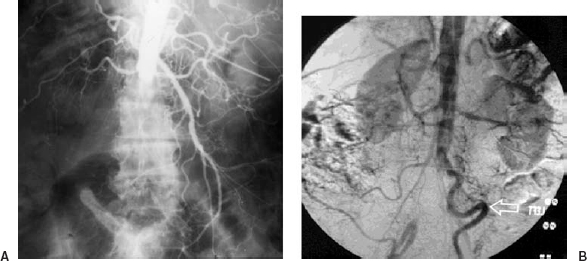
FIGURE 20-4. (A). Acute aortic occlusion, studied via translumbar aortogram. There are atherosclerotic renal arteries and a normal superior mesenteric artery. (B). Another patient demonstrates chronic aortic occlusion. There is a markedly enlarged and tortuous inferior mesenteric artery providing collateral flow.
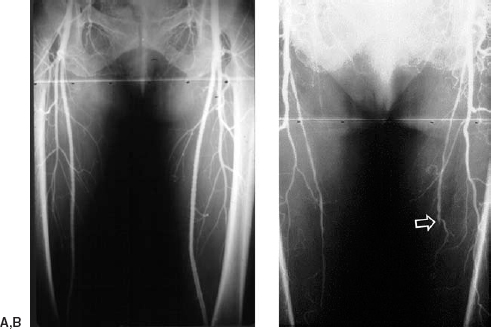
FIGURE 20-5. (A). Normal femoral arteriogram showing widely patent common, superficial, and deep femoral arteries bilaterally. (B). Arteriogram from another patient shows patent profunda femoral arteries and diffuse atherosclerosis of the superficial femoral arteries which occlude at the adductor canal on the right and just above the adductor canal on the left (arrow). Note the rear symmetry.
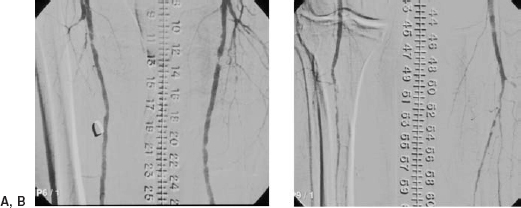
FIGURE 20-6. Severe bilateral multilevel infrainguinal disease in a male patient with diabetes mellitus. (A). Severe bilateral superficial femoral and popliteal artery occlusive disease. (The bullet in the soft tissues is old.) (B). Marked severe bilateral tibial disease.
Combinations of percutaneous and open procedures and surgery can be used to treat multisegment disease.2 For example, donor iliac artery angioplasty and stenting may be used to improve inflow for a cross-femoral graft. The presence of a pressure gradient across an iliac stenosis indicates the need for dilatation (Figs. 20-7 through 20-9).3
Some interventional radiologists prefer primary stenting of all iliac artery occlusions and stenoses; however, there is evidence to suggest that the first-line treatment for a focal, simple iliac stenosis should be angioplasty, with stenting reserved for percutaneous transluminal angioplasty (PTA) failure or complex lesion morphology such as occlusion, ulceration, or grossly irregular plaque (Fig. 20-10).4,5 Immediate PTA failure is defined by the presence of residual pressure gradient, flow limiting dissection, thrombosis, or elastic recoil with residual lumenal narrowing.6
Many interventional radiologists prefer primary stenting (i.e., stent placement without preceding PTA) of all external iliac artery lesions, believing that the external iliac artery is more susceptible to PTA-related dissection, occlusion, or perforation (Figs. 20-11 and 20-12). The use of PTA with stenting has resulted in patency rates in the iliac segments of 90% and 80% at 1 and 3 years respectively. Angioplasty alone is generally applied to focal, simple stenoses of the common iliac arteries (Figs. 20-13 through 20-15). The use of stents in conjunction with a PTA in the aortoiliac segments has improved immediate technical success and durability. Technical success for all occlusions and stenoses ranges from 85 to 99%, with primary patency and clinical success rates at 2 to 3 years of up to 80 to 82%.6–9 With secondary interventions, patency rates can be improved even further.10 Procedural complications range from 4 to 7% (Fig. 20-16).

FIGURE 20-7. Cross-femoral bypass graft (vertical arrow). The donor right common iliac artery is moderately narrowed (arrowhead) but demonstrated no pressure gradient. The right internal iliac artery is occluded.
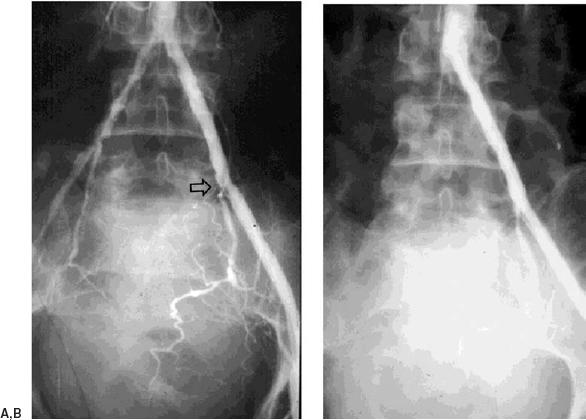
FIGURE 20-8. (A). There is a focal lesion at the junction of the common and external iliac artery (arrow). No gradient was demonstrated without pharmacologic enhancement. After a 60 mg intra-arterial bolus of papaverine, a gradient of 25 mmHg was measured. (B). After angioplasty, luminal is widely patent, and the gradient was resolved. The left iliac artery was used as a donor for a left-to-right cross-femoral bypass graft.
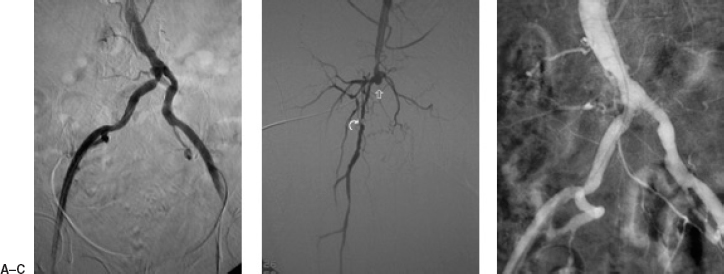
FIGURE 20-9. (A). Right common iliac artery stenosis with poststenotic dilatation in 77-year-old woman with end-stage renal disease, chronic critical lower limb ischemia, and femoropopliteal occlusion. The poststenotic dilatation infers hemodynamic significance. (B). Superficial femoral artery occlusion (vertical arrow) and marked diffuse disease of the profunda femoris artery (curved arrow). This virtually occluded outflow from the iliac segments precluded generation of an effective pressure gradient across the lesion. (C). A primary stent was placed with luminal restoration prior to planned right femoropopliteal bypass surgery.
It is important to note that many patient-related and anatomy-related factors will affect the outcome of a PTA and stenting. In general, focal disease responds well to percutaneous therapy, whereas diffuse disease does not. Proximal lesions (e.g., aortoiliac segments) respond better to either percutaneous techniques or surgery than do distal ones (e.g., tibial segments). Stenoses historically fare better than occlusions, primarily because some occlusions cannot be crossed. With current technology, virtually all femoropopliteal artery stenoses and occlusions now can be crossed and dilated. The status of runoff below the angioplasty site is an extremely important predictor of patency. Patients presenting with critical limb ischemia rather than claudication generally fare less well with percutaneous techniques, primarily because they have more diffuse disease. Similarly, diabetic patients have been reported to fare worse than nondiabetics with infrainguinal PTA, but this is probably statistically confounded by runoff status and extent of disease.11
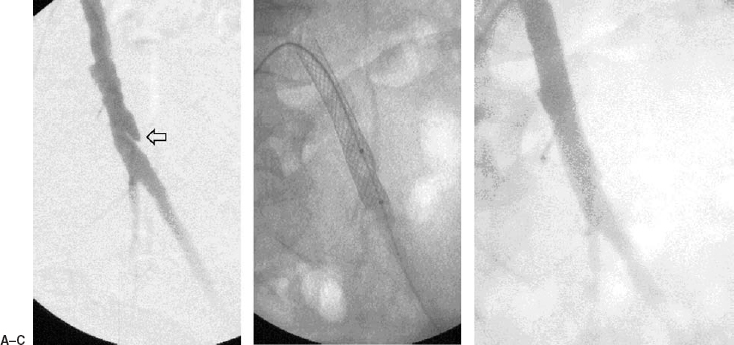
FIGURE 20-10. (A). Left common iliac artery atherosclerotic plaque with ulceration (arrow). (B). This was treated by primary stenting from the contralateral approach. (C). Follow-up arteriogram demonstrates excellent results.
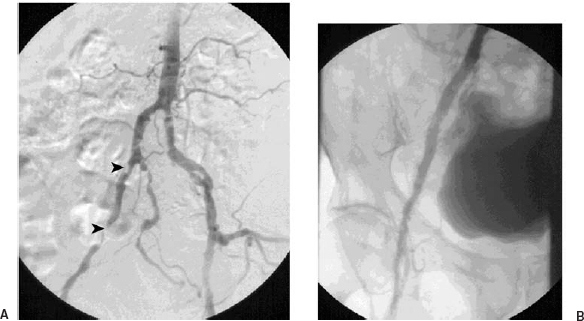
FIGURE 20-11. (A). Moderate diffuse disease of the right external artery is noted. Two focal stenoses are noted by the arrowheads. (B). The patency of the external iliac artery is restored after primary stenting.
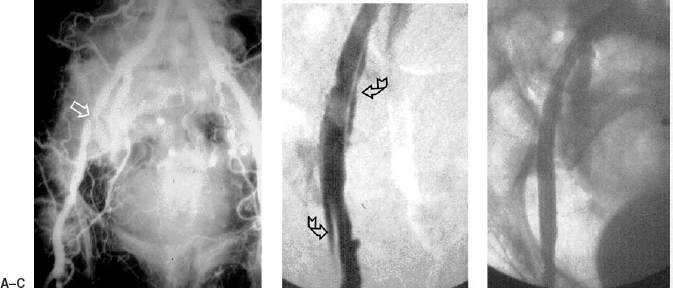
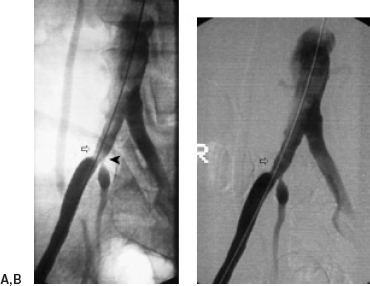
FIGURE 20-12. (A). Tight focal right external iliac artery lesion is noted (arrowhead) in a patient with severe multilevel occlusive disease and critical ischemia. Right femoropopliteal bypass graft was planned after percutaneous restoration of iliac inflow. (B). Post angioplasty dissection is noted (curved arrows). This was partially occlusive. (C). A self-expanding stent was placed to tack this dissection down, with restoration of the lumen.
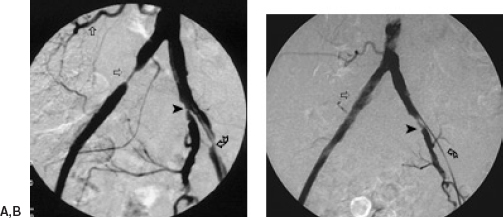
FIGURE 20-13. (A). Concentric tight focal right iliac artery stenosis (horizontal arrow). There is a large right L-4 collateral (vertical arrow). Note is also made of severe stenoses of the left external iliac (curved arrow) and internal iliac (arrowhead) arteries. The patient had markedly diminished femoral pulses bilaterally. (B). After an angioplasty of the right iliac artery that was performed around the aortic bifurcation, the sheath was placed in the left iliac artery to perform the right iliac angioplasty. There is excellent lumenal restoration (horizontal-arrow) with return of a normal right femoral pulse. The left iliac catheter is highly occlusive in the diseased external iliac artery segment with essentially no flow down the external iliac artery (curved arrow); the patient was heparinized to prevent left iliac thrombosis. The arrowhead highlights the left internal iliac artery.
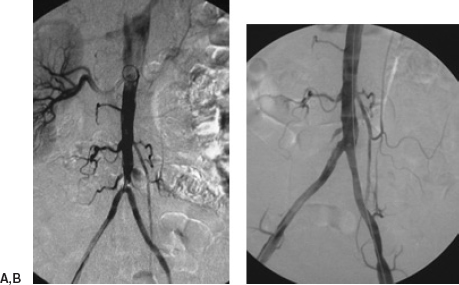
FIGURE 20-14. (A). Focal stenosis of the aortic bifurcation in a patient with Leriche’s syndrome. (B). Excellent result after angioplasty with (bilateral) “kissing balloon.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree