Chapter Outline
Since the 1980s, advances in cross-sectional imaging and endoscopy have led to a gradual but steady decline in the number of barium studies performed in the United States. Although barium studies no longer reign supreme in the diagnosis of gastrointestinal (GI) disease, single- and double-contrast examinations continue to have a role in modern radiology practice. In general terms, barium studies can demonstrate GI abnormalities in three ways:
- 1.
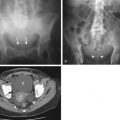
Mucosal relief views of the collapsed or partially collapsed lumen obtained with a small volume of barium. These views enable visualization of the folds in various portions of the GI tract ( Fig. 2-1A ). Because the folds contain a submucosal core, these views are particularly useful for showing abnormalities involving the submucosa, such as esophageal varices.
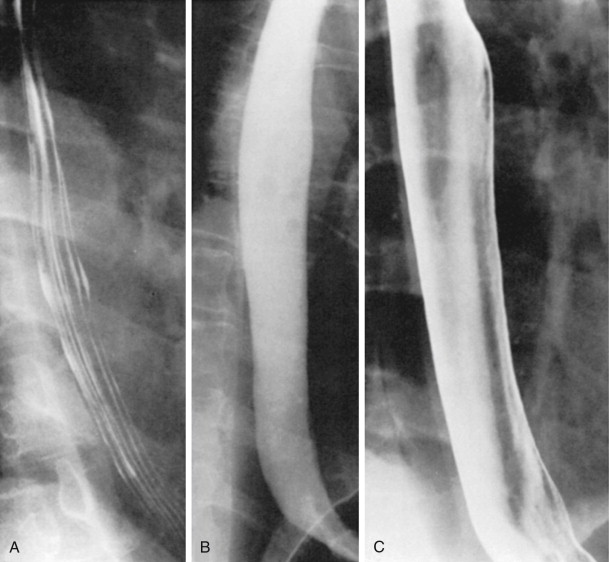
Figure 2-1
Three types of views for visualizing the gastrointestinal tract, as illustrated in the esophagus.
A. Mucosal relief view. With the esophagus collapsed and coated, the normal longitudinal folds are seen. B. Single-contrast view. With the patient continuously drinking barium in the prone position, the barium-filled esophagus is demonstrated. C. Double-contrast view. With the patient in the upright position, the smooth, featureless surface of the esophagus is seen.
- 2.
Single-contrast views of the filled lumen obtained with a large volume of low-density barium ( Fig. 2-1B ). These views enable visualization of contour abnormalities, strictures, and large polypoid defects.
- 3.
Double-contrast views obtained after the mucosal surface has been coated with a thin layer of high-density barium and the lumen has been distended with gas ( Fig. 2-1C ). These views enable visualization of subtle mucosal lesions, such as the early changes of inflammatory bowel disease and early neoplastic lesions.
Although these three types of views are incorporated to varying degrees in both single- and double-contrast examinations, single-contrast studies rely more heavily on diagnostic fluoroscopy, mucosal relief, and barium filling, whereas double-contrast studies emphasize the interpretation of double-contrast images supplemented by barium filling and mucosal relief.
In the past, there was considerable controversy about the relative virtues of single-contrast and double-contrast techniques. Currently, however, most authors believe that double-contrast techniques provide superior mucosal detail and allow earlier detection of subtle lesions than single-contrast techniques. As a result, it is generally recommended that double-contrast studies be performed on patients who are young enough and healthy enough to undergo this type of examination. In contrast, single-contrast barium studies are most appropriate in older or debilitated patients who are unable to cooperate for a double-contrast examination.
This chapter discusses the principles for performing and interpreting single- and double-contrast barium studies. These principles are illustrated with examples drawn from throughout the GI tract.
Single-Contrast Studies
Diagnostic Principles
Depending on the organ examined, single-contrast techniques may include observation of function (e.g., pharyngeal and esophageal motility), compression imaging, full-column distention, mucosal relief views, and limited air-contrast images. The use of compression during fluoroscopy is a critical component of the single-contrast examination. Small lesions (e.g., small ulcers, polypoid neoplasms) are often visible only when the barium pool is adequately thinned or displaced by manual compression. The barium suspension must also be adequately diluted if lesions (especially small lesions) are to be detected in the thinned-out barium pool.
Full-column distention of the lumen is ideal for showing strictures, large neoplasms, and lesions projecting tangentially, such as ulcers or diverticula. Full-column views of barium-filled structures in various projections enable depiction of large ulcers and tumors. However, small lesions may be visible on full-column views only when viewed in profile. In such cases, mucosal techniques are required to supplement the barium-filled views.
Equipment
Fluoroscopic equipment has evolved dramatically with the transition from analogue cassette-based radiography to digital imaging and viewing on picture archiving and communications system (PACS) workstations. Regardless of the imaging technology, single-contrast examinations can be performed with conventional or remote control fluoroscopic units. The ability to obtain optimal compression views is a major prerequisite of any well-designed fluoroscope. Compression can be performed manually or with a variety of hand-held devices on a conventional unit; alternatively, the plastic cone on the spot image device of the fluoroscope can be used for applying compression.
On remote control equipment, compression is easily performed with a vertical movable device incorporated into the machine, facilitated by the ability to angle the x-ray tube. Remote control units often contain a compression device that allows graded compression and tube angulation with compression. Nevertheless, many radiologists prefer standard fluoroscopic units rather than remote control units because it is generally easier to move, turn, and compress the patient when the fluoroscopist performing the procedure is at the tableside.
Barium Suspensions
Numerous barium products are available commercially; a number are formulated for specific purposes, whereas others can be used for a variety of examinations. Barium suspensions for single-contrast studies should be of moderate density (50%-100% w/v) when not diluted. The optimal barium suspension for a particular study depends on the structure being examined and the type of examination being performed. For example, an esophagogram requires a moderately dense barium suspension that provides full-column and mucosal relief imaging; a high-density barium suspension or paste may also be needed for optimal mucosal coating. A similar barium suspension can be used for an upper GI series, in which compression views, mucosal relief views, and limited double-contrast views are required. A standard peroral small bowel follow-through study can be performed with the same barium suspension used for the upper GI series. A single-contrast enteroclysis study requires a 15% to 20% w/v barium suspension, although somewhat denser solutions have been recommended. Finally, a 15% to 20% w/v barium suspension is used for a single-contrast barium enema, because this is the optimal suspension for obtaining compression views of the colon.
Quality Controls
Quality control for single-contrast examinations requires balancing the barium density, kilovoltage, and width of the barium column to achieve adequate translucency of the barium-filled bowel. This permits radiographic penetration of the barium suspension to visualize lesions that might otherwise be obscured by barium in the lumen. The visibility of skeletal shadows through the barium column indicates that small filling defects are more likely to be seen, which is particularly important for the detection of colonic polyps.
Another quality control consideration, especially during the barium enema and small bowel follow-through, is the ability to see through overlapping loops of bowel. On barium enemas, a tortuous sigmoid colon may have overlapping loops, even with appropriate compression. Similarly, on small bowel follow-throughs, overlapping small bowel loops in the pelvis may compromise the fluoroscopist’s ability to detect abnormalities in the distal ileum. In such cases, pelvic loops can be better visualized by placing the patient in a prone position while he or she lies on a bolster or inflated balloon to lift these loops superiorly from the pelvis.
Esophagography
Routine single-contrast esophagography includes fluoroscopic observation of the esophagus supplemented by motion recordings, full-column views, and mucosal relief views. Full-column (barium-filled views) and mucosal relief views constitute the single-contrast phase of the examination. Motion recordings can be used to document pharyngeal function and esophageal motility using analog or digital recordings or rapid sequence solid-state recordings built into modern digital fluoroscopes.
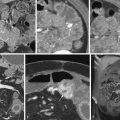
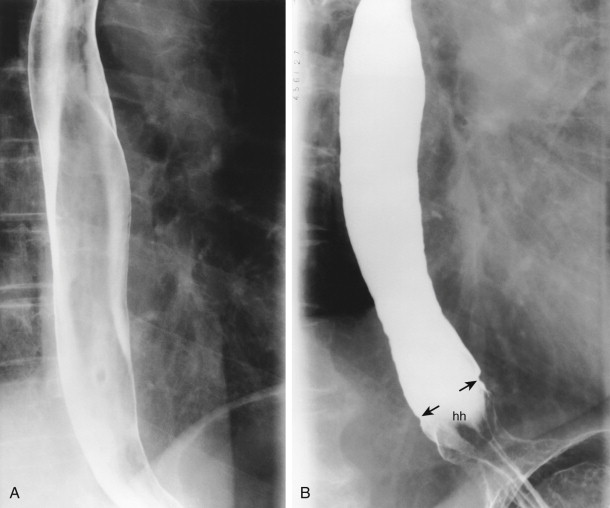
Depending on the imaging options of the fluoroscopic equipment, full-column technique is performed by obtaining partial or full-length views of the esophagus distended with barium. These views allow detection of esophageal carcinoma ( Fig. 2-2 ) and other abnormalities at the gastroesophageal junction such as hiatal hernias, peptic strictures, and lower esophageal rings. Lower esophageal rings are best visualized on prone views of the barium-filled lower esophagus, sometimes supplemented with a solid bolus such as a marshmallow or barium tablet.

Full-column images of the esophagus are usually obtained with the patient on the fluoroscopic table in the prone, right anterior oblique position; a bolster may be used to increase intra-abdominal pressure. Esophageal peristalsis is inhibited by rapid swallowing of barium, allowing the esophagus to distend fully. Multiple images of the esophagus should be obtained at all levels; these images may be full-length views of the esophagus or coned-down views at different levels, depending on the imaging options of the fluoroscopic equipment.
Maximal distention of the esophagogastric region is required for optimal detection of hiatal hernias and lower esophageal rings ( Fig. 2-3 ). Rapid ingestion of the barium suspension followed by deep inspiration (or a Valsalva maneuver) promotes distention of the gastroesophageal junction. Careful fluoroscopic observation is required to visualize lesions only seen when this region is optimally distended.
Full-column views are complemented by mucosal relief views of the collapsed esophagus, with coating of the longitudinal folds by the barium suspension. A high-density barium suspension (e.g., that used for a double-contrast upper GI series) is ideal for this purpose. The patient takes one or several swallows of high-density barium to coat the esophageal folds with barium. These mucosal relief views may reveal thickened, irregular folds, small esophageal neoplasms, and reflux or infectious esophagitis ( Fig. 2-4 ). Nevertheless, double-contrast views are better for showing the plaques of Candida esophagitis, the small ulcers of herpes esophagitis, and the giant ulcers of cytomegalovirus (CMV) or human immunodeficiency virus (HIV) esophagitis.

Single-contrast mucosal relief views are also best for detecting esophageal varices. The patient takes several swallows of the barium suspension, which coats the lower esophagus, and is then asked not to swallow to inhibit peristalsis. Intermittent fluoroscopic observation is performed for several minutes to visualize the varices optimally as they become more distended.
Fluoroscopic observation is an integral part of the radiographic evaluation of the esophagus and is usually adequate to assess esophageal function. Motion recording methods greatly aid in evaluating oropharyngeal swallowing disorders because of the rapid events that occur with deglutition, and may also be used to assess esophageal motility. Motion recordings should be obtained while the patient takes multiple discrete swallows of barium, because rapid swallowing causes reflex inhibition of esophageal peristalsis. With the use of single swallows, the single-contrast esophagogram is an excellent technique for evaluating esophageal motility.
Upper Gastrointestinal Series
The single-contrast upper GI series is a complex examination requiring fluoroscopic observation, abdominal compression, and the use of multiple techniques for examining the esophagus, stomach, and duodenum. The study can be performed quickly and is tolerated even by patients who are immobile or unable to cooperate fully.
The examination starts with the table upright. After the patient ingests several swallows of barium, the stomach is compressed with a compression paddle or the cone on the fluoroscope to demonstrate the rugal folds, assess the pliability of the gastric wall, and detect focal areas of rigidity secondary to tumor or scarring. If the stomach empties, the barium-filled duodenal bulb can also be examined by compression in the upright position.
The table is then lowered to the horizontal position, and mucosal relief views of the stomach are obtained, first with the patient in a supine position and then after the patient turns into a prone position. These views supplement the upright compression views and can sometimes show small polyps, erosions, or ulcers that are later obscured in the barium-filled stomach ( Fig. 2-5 ).

With the patient in the prone, right anterior oblique position, the esophagus is then examined using the same techniques described previously (see earlier, “Esophagography”). The gastric antrum and duodenal bulb usually fill with barium in this position, so prone compression views of the antrum and duodenal bulb should be obtained using an inflatable balloon placed beneath the patient to thin out the barium pool, enabling detection of anterior wall lesions in the antrum and duodenal bulb ( Fig. 2-6 ).

With the patient in the supine, left posterior oblique position, air in the stomach rises into the gastric antrum and duodenal bulb, so limited double-contrast images of these areas can be obtained ( Fig. 2-7 ). Compression can be used to displace the barium suspension, separate antroduodenal structures, and improve distention with air. The fluoroscopic portion of the examination is completed at this time. Some radiologists may then choose to obtain a standard set of overhead radiographs of the stomach and duodenum with the patient in prone, supine, right anterior oblique, and right lateral positions.

Small Bowel
The small bowel can be examined by single-contrast technique with a small bowel follow-through, enteroclysis, or retrograde study via an ostomy or reflux from the colon. A peroral small bowel follow-through may be performed after a single-contrast upper GI series or as a separate study. A large volume (≥500 mL) of barium is recommended to promote gastric emptying, accelerate small bowel transit, and optimally distend small bowel loops. Fluoroscopic imaging and compression of all small bowel loops is a critical component of the examination because focal lesions are easily obscured by overlapping loops of small bowel unless compression is applied to separate these loops and ensure an adequate examination.
A small bowel follow-through typically requires a minimum of 500 mL of orally ingested barium, which can be the same product used for a single-contrast upper GI series. Prone overhead or low-magnification digital images of the small intestine are taken at timed intervals (e.g., every 30 minutes) until barium fills the right side of the colon. Depending on the barium product used, transit time through the small bowel is typically 60 to 90 minutes. Fluoroscopic spot imaging with manual compression should be performed at regular intervals during the examination. Compression of all loops and appropriate imaging of the entire small bowel is required to optimize detection of abnormalities ( Fig. 2-8 ). When the barium suspension has reached the colon, compression views of the terminal ileum are obtained (typically with the patient in a supine or left posterior oblique position) for optimal visualization of this region.

Clear delineation of pelvic loops of small bowel, which often overlap, is not always possible, but several maneuvers may be performed to improve visualization of these loops. First, the patient should be told not to void during the examination because a full bladder elevates pelvic small bowel loops, enabling them to be separated with manual compression. A similar effect may be achieved by instilling air into the rectum. The patient can also be placed in a prone Trendelenburg position with an inflated balloon beneath the lower abdomen and pelvis to displace pelvic small bowel loops superiorly for better visualization of these loops. If a remote control unit is available, the tube can be angulated to further separate these loops ( Fig. 2-9 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree