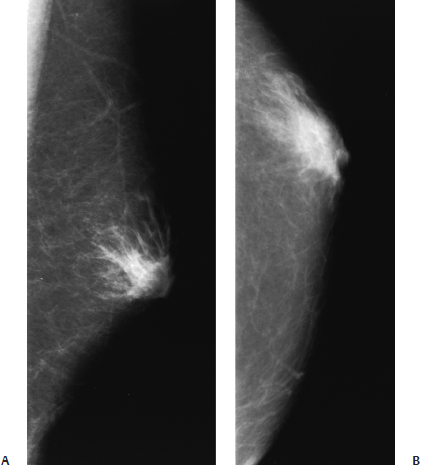
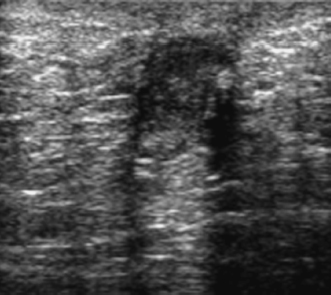
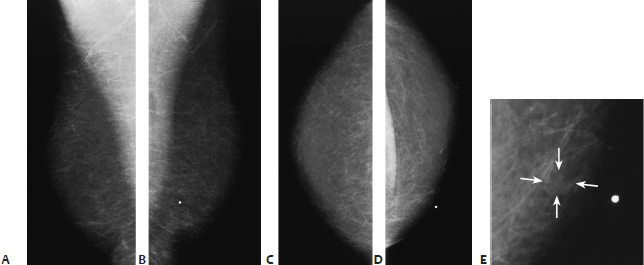
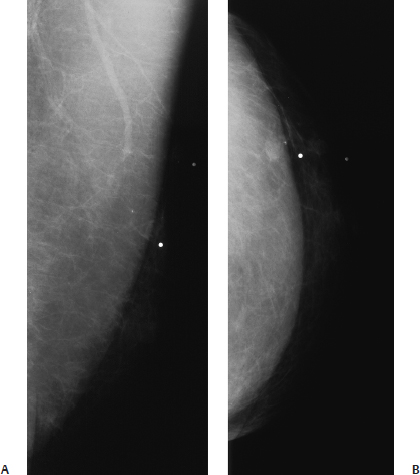
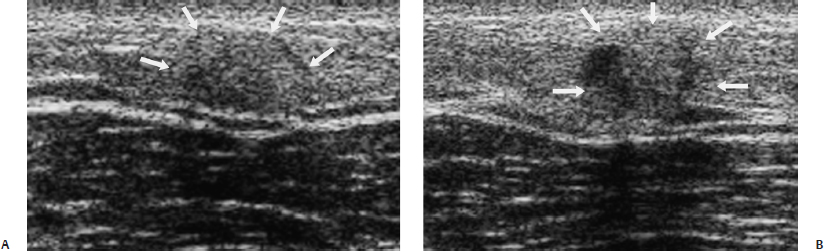
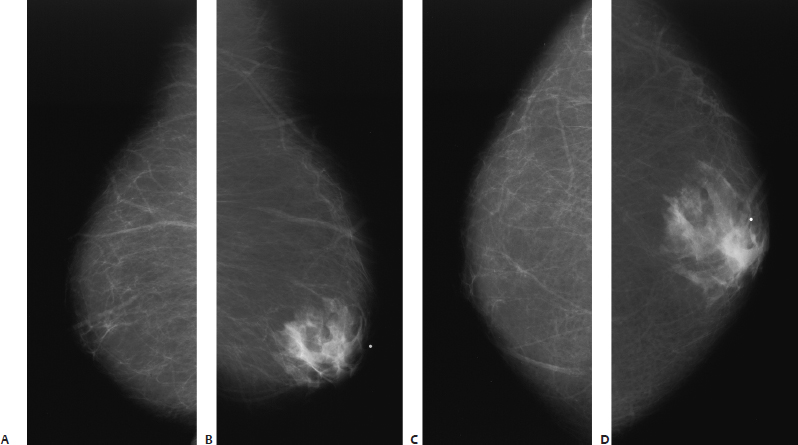
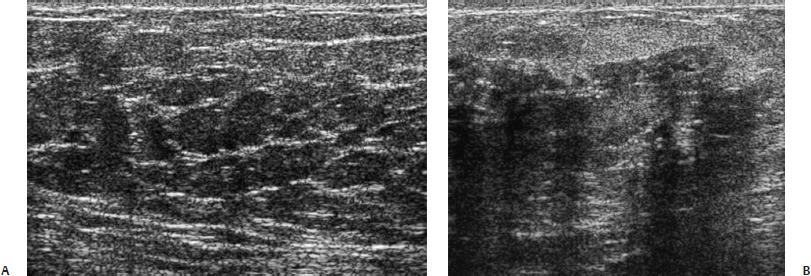
24 Benign Male Breast A 64-year-old man presents with a chronic draining sinus tract in the left breast. Two years earlier, he had a hypophysectomy for Cushing’s disease, and he has chronic pituitary insuffciency. • Left breast: ulcerated nipple with a subareolar mass • Right breast: enlarged but otherwise normal Fig. 24.1 There is ill-defined left subareolar density with coarse linear densities extending into the surrounding fat. (A) Left MLO mammogram. (B) Left CC mammogram. Frequency • 7.5 MHz Mass (Fig. 24.2) • Margin: well defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: mild acoustic enhancement • Shape: ellipsoid Fig. 24.2 Left transverse breast sonogram. Under the nipple, there is a hypoechoic, well-defined fluid collection with mild posterior acoustic enhancement. • Abscess • Nipple discharge cultures positive for Staphylococcus aureus • BI-RADS assessment category 3, probably benign; short-interval follow-up • Because subareolar abscess is a rare lesion of the male breast, there is little previous clinical and radiographic information. In women, the most common infecting organism is Staphylococcus aureus. These lesions are commonly recurrent and require excision. This patient failed antibiotic therapy and eventually was treated with excision. • In females, mammographically, these abscesses produce an ill-defined subareolar mass. Sonographically, there is a hypoechoic fluid collection, which may be mistaken for a solid mass. Appelbaum AH, Evans GFF, Levy KR, Amirkhan RH, Schumpert TD, Schumpert TD. Mammographic appearances of male breast disease. Radiographics 1999;19:559–568 Tavassoli FA. Pathology of the Breast. 2nd ed. Stamford: Appleton & Lange; 1999:792 A 75-year-old man presents with a new left breast mass. • Left breast: palpable, firm, nontender lump at the 9 o’clock position • Right breast: normal exam Mass (Fig. 24.3) • Margin: indistinct • Shape: irregular • Density: fat-containing Fig. 24.3 In the left inner breast, the palpable lump corresponds to a small, faint, ill-defined opacity that is partially fat density (arrows). (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. (E) Left CC spot magnification mammogram. • Angiolipoma • BI-RADS assessment category 2, benign finding • Angiolipomas resemble lipomas. They are encapsulated masses of mature lipocytes with a prominent vascular network. Angiolipomas are commonly found in men. An Armed Forces Institute of Pathology (AFIP) series reported that 17 (24%) of 70 breast angiolipomas were found in men. • Mammographically, angiolipomas commonly have a benign, fat density appearance. Tavassoli FA. Pathology of the Breast. 2nd ed. Stamford: Appleton & Lange; 1999:695–697 A 51-year-old man presents with new left breast lumps. • Left breast: two firm nodules between the 12 o’clock and 1 o’clock positions • Right breast: normal exam Mass (Fig. 24.4) • Margin: indistinct • Shape: oval • Density: equal density Fig. 24.4 In the left upper breast, there are two palpable lumps that correspond to two ill-defined oval masses. (A) Left MLO mammogram. (B) Left CC mammogram. Frequency • 13 MHz Mass (Fig. 24.5) • Margin: ill defined • Echogenicity: isoechoic • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 24.5 The palpable lumps correspond to two solid masses. One mass (A) is an oval, ill-defined, isoechoic mass (arrows). The other mass (B) is an oval, ill-defined mass with heterogeneous echogenicity (arrows). (A) Left longitudinal breast sonogram. (B) Left longitudinal breast sonogram. • Fat necrosis • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Fat necrosis in men is radiographically similar to that in women. Mammographically, fat necrosis produces either a well-defined fat density mass (oil cyst) or an ill-defined irregular mass. The latter abnormality generally cannot be differentiated from malignancy. • Sonographically, fat necrosis in the male breast is identical to that in the female breast. The mammographic irregular mass generally corresponds to an irregular hypoechoic mass. Occasionally, fat necrosis has a more benign hyperechoic appearance. Chantra PK, So GJ, Wollman JS, Bassett LW. Mammography of the male breast. AJR Am J Roentgenol 1995;164:853–858 Stewart RA, Howlett DC, Hearn FJ. Pictorial review: the imaging features of male breast disease. Clin Radiol 1997;52:739–744 A 72-year-old markedly obese male presents with left breast tenderness. • Left breast: mildly tender, slightly soft, fullness under the nipple without mass • Right breast: normal exam Fig. 24.6 the right breast is completely fatty and normal for an overnweight man. The left breast exhibits mild fan-shaped subareolar density which corresponds to the region of tenderness. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. Frequency • 13 MHz Fig. 24.7 Right breast (A) exhibits normal predominately fatty architecture. The tissue of the left breast is heterogeneous echogenicity with random intermittent shadowing. (A) Right radial breast sonogram. (B) Left radial breast sonogram. • Left gynecomastia • BI-RADS assessment category 2, benign finding. • Gynecomastia is clinically defined as more than 2 cm of palpable subareolar tissue in the male breast. In one nonselective autopsy study of 100 men, 55% had gynecomastia. Clinically, most men present with unilateral symptoms. Only 20 to 30% of men note bilateral breast enlargement. The breast enlargement is due to benign ductal and stromal hyperplasia. In this case, the left breast exhibits nodular gynecomastia.
Case 24.1: Abscess
Case History
Physical Examination
Mammogram (Fig. 24.1)
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 24.2: Angiolipoma
Case History
Physical Examination
Mammogram
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 24.3: Fat Necrosis
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 24.4: Gynecomastia—Nodular Pattern/Normal Fatty Male Breast
Case History
Physical Examination
Mammogram (Fig. 24.6)
Ultrasound (Fig. 24.7)
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine