• Heavily T2-weighted coronal oblique fast spin-echo sequence to obtain source data (aligned along the plane of the common bile duct (CBD)) • Source data allows MIP reformats to be generated (highlighting fluid-filled structures) – usually a number of coronal MIP reformats over 180° • Secretin: this stimulates exocrine pancreatic secretion, distending the pancreatic duct and improving its visualization (acts immediately, returning to baseline at 10 min) • Functional MR cholangiography: using delayed imaging at 30–60 mins with the hepatobiliary excreted contrast agents Gd-EOB-DTPA (Primovist) or Gd-BOPTA (MultiHance) • Normal morphology: only central intrahepatic ducts are normally seen (≤ 3mm) • Right posterior hepatic duct (segments VI/VII): almost horizontal course • Right anterior hepatic duct (segments V/VIII): more vertical course • Left hepatic duct (segments II–IV): joins the right to form the common hepatic duct • Cystic duct insertion into common hepatic duct: right lateral (50%) • Common variants: an aberrant right posterior duct draining into the common hepatic duct or cystic duct • Technique: volume averaging artefacts in MIP reformats can obscure filling defects – source images must always be reviewed • Normal variants: a long cystic duct running parallel to the CBD, stimulating a distended CBD • Intraductal factors mimicking filling defects: aerobilia (non-dependent) • Extraductal factors: pulsatile vascular compression from adjacent vessels mimicking a stricture (but no proximal dilatation) • Hepatobiliary iminodiacetic acid (HIDA) scintigraphy: this is a bilirubin analogue labelled with 99mTc • There is normally accumulation of isotope within liver, bile ducts, gallbladder, duodenum and small bowel by 1 h • This allows direct bile and pancreatic duct opacification, as well as visual assessment of the duodenum and ampulla of Vater • The main complication is the precipitation of pancreatitis • The main pitfall is the presence of underfilled ducts above a stricture • Stones present within the gallbladder – this affects 15% of the Western population (F>M) • Gallstone composition: cholesterol (70%) • Reasons for non-visualization of the gallbladder: a previous cholecystectomy • Biliary sludge: this is composed of calcium bilirubinate granules, cholesterol crystals and glycoproteins
Biliary
METHODS OF INVESTIGATION
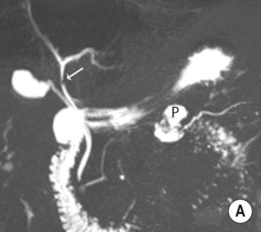
MAGNETIC RESONANCE CHOLANGIOPANCREATOGRAPHY (MRCP)
Technique
 Stationary water appears as areas of high SI and adjacent soft tissue is low SI (therefore it is not reliant on contrast excretion and can be used in jaundiced patients)
Stationary water appears as areas of high SI and adjacent soft tissue is low SI (therefore it is not reliant on contrast excretion and can be used in jaundiced patients)
 Fasting reduces any unwanted signal from the adjacent intestine
Fasting reduces any unwanted signal from the adjacent intestine
 Breath-hold or non-breath-hold (respiratory triggered) imaging
Breath-hold or non-breath-hold (respiratory triggered) imaging
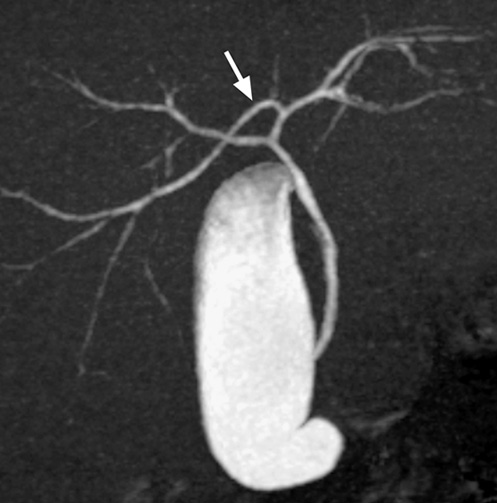
Normal anatomy
 extrahepatic ducts ≤ 7mm (CBD up to 10mm post cholecystectomy)
extrahepatic ducts ≤ 7mm (CBD up to 10mm post cholecystectomy)  pancreatic duct ≤ 3mm
pancreatic duct ≤ 3mm  accessory pancreatic duct in 45%
accessory pancreatic duct in 45%
 separate drainage of segment I
separate drainage of segment I
 anterior (30%)
anterior (30%)  posterior (20%)
posterior (20%)
 drainage of the right anterior or posterior duct into the left hepatic duct
drainage of the right anterior or posterior duct into the left hepatic duct  a triple confluence at the hilum
a triple confluence at the hilum
Imaging pitfalls
 MIP reformats can also over- and underestimate strictures
MIP reformats can also over- and underestimate strictures
 a contracted sphincter mimicking an impacted stone
a contracted sphincter mimicking an impacted stone
 flow phenomena (central signal void)
flow phenomena (central signal void)  debris
debris  haemorrhage
haemorrhage
 susceptibility artefact from surgical clips
susceptibility artefact from surgical clips
HEPATOBILIARY SCINTIGRAPHY
 It is injected intravenously with serial images obtained over 2–4 h (it requires near-normal bilirubin levels)
It is injected intravenously with serial images obtained over 2–4 h (it requires near-normal bilirubin levels)
ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY (ERCP)
 It also allows for: biopsy
It also allows for: biopsy  brushings
brushings  sphincterotomy
sphincterotomy  stone extraction
stone extraction  biliary stenting
biliary stenting  biliary stricture dilatation
biliary stricture dilatation
CHOLELITHIASIS AND CHOLEDOCHOLITHIASIS
CHOLELITHIASIS
DEFINITION
 there is a small lifetime risk of developing a gallbladder carcinoma
there is a small lifetime risk of developing a gallbladder carcinoma
 pigment stones composed of calcium bilirubinate (up to 30%)
pigment stones composed of calcium bilirubinate (up to 30%)
PEARLS
 a non-fasting state
a non-fasting state  an abnormal gallbladder position
an abnormal gallbladder position  emphysematous cholecystitis
emphysematous cholecystitis  a gallbladder full of stones
a gallbladder full of stones
 it is commonly see with fasting states, critically ill patients, pregnancy, and in those patients receiving total parenteral nutrition
it is commonly see with fasting states, critically ill patients, pregnancy, and in those patients receiving total parenteral nutrition  it resolves spontaneously in 50% of cases
it resolves spontaneously in 50% of cases
CHOLECYSTITIS
ACUTE CALCULOUS CHOLECYSTITIS
Radiology Key
Fastest Radiology Insight Engine


 the assessment of bile leaks and biliary communication with cysts
the assessment of bile leaks and biliary communication with cysts  the demonstration of segmental obstruction
the demonstration of segmental obstruction

 a contracted gallbladder (e.g. following a recent meal)
a contracted gallbladder (e.g. following a recent meal)
 it can also allow fine-needle aspiration cytology to be performed
it can also allow fine-needle aspiration cytology to be performed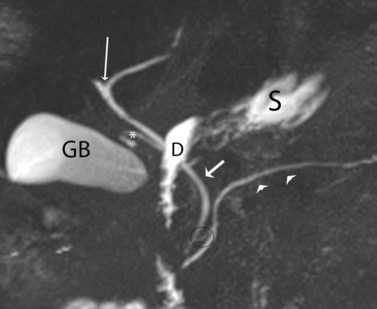



 larger stones tend to be laminated
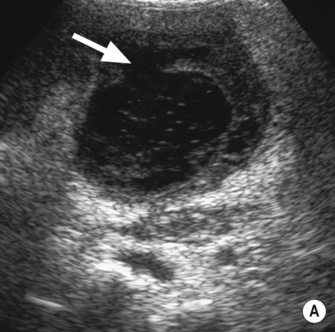
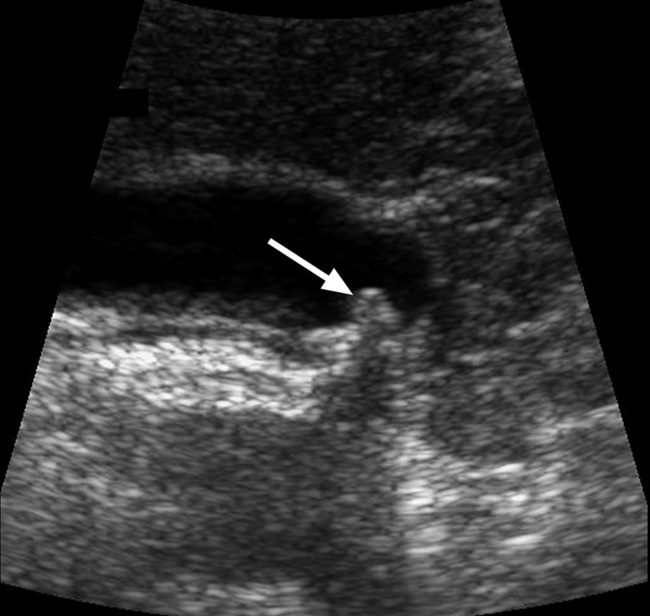
larger stones tend to be laminated gallstones appear as echogenic foci which cast acoustic shadows
gallstones appear as echogenic foci which cast acoustic shadows  stone mobility is frequently demonstrated (unless it is impacted at the neck)
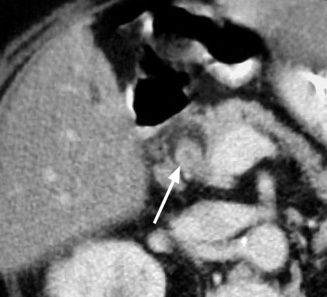
stone mobility is frequently demonstrated (unless it is impacted at the neck) these are hypodense, hyperdense or of mixed density
these are hypodense, hyperdense or of mixed density small gallstones can be difficult to detect if they lie within any sludge
small gallstones can be difficult to detect if they lie within any sludge


 primary sclerosing cholangitis
primary sclerosing cholangitis  recurrent pyogenic cholangitis
recurrent pyogenic cholangitis  Caroli’s disease
Caroli’s disease obstructive jaundice
obstructive jaundice  pancreatitis
pancreatitis a duct diameter < 4mm carries a high negative predictive value for choledocholithiasis (regardless of the gallbladder status)
a duct diameter < 4mm carries a high negative predictive value for choledocholithiasis (regardless of the gallbladder status)



 specificity > 95%)
specificity > 95%) it can diagnose stones that are <5mm in diameter
it can diagnose stones that are <5mm in diameter  its main weakness is its reliance on a near-normal serum bilirubin
its main weakness is its reliance on a near-normal serum bilirubin this has a high sensitivity (up to 94%) and specificity (99%)
this has a high sensitivity (up to 94%) and specificity (99%)  its quality is independent of the serum bilirubin levels
its quality is independent of the serum bilirubin levels haemobilia
haemobilia  flow voids
flow voids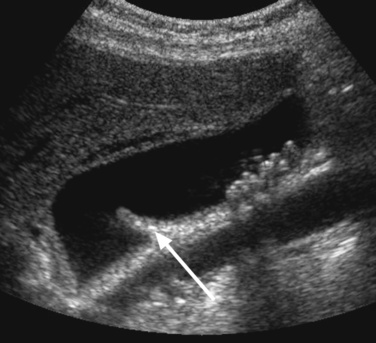

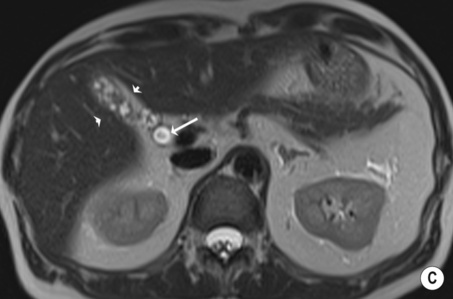
 hypoechoic line between two echogenic lines (arrow).*
hypoechoic line between two echogenic lines (arrow).*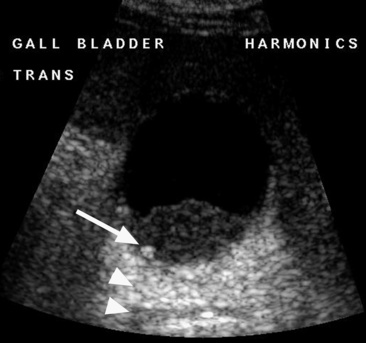


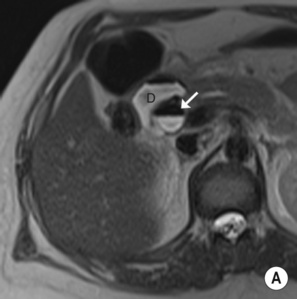
 the signs include:
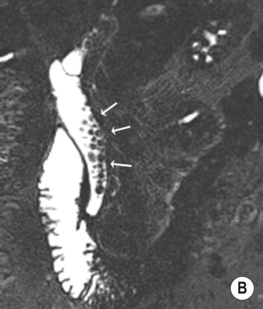
the signs include: gallbladder distension (>5cm)
gallbladder distension (>5cm)  pericholecystic fluid and gallbladder wall striations (± wall hyperaemia on Doppler)
pericholecystic fluid and gallbladder wall striations (± wall hyperaemia on Doppler)  gallstones (common bile duct stones are suggested by abnormal liver function tests)
gallstones (common bile duct stones are suggested by abnormal liver function tests)
 subserosal oedema and gallbladder distension
subserosal oedema and gallbladder distension  high-density bile
high-density bile  pericholecystic fluid and inflammatory stranding within the pericholecystic fat
pericholecystic fluid and inflammatory stranding within the pericholecystic fat  variable enhancement of the gallbladder wall
variable enhancement of the gallbladder wall emphysematous cholecystitis
emphysematous cholecystitis  empyema formation
empyema formation hepatitis
hepatitis  pancreatitis
pancreatitis  gallbladder wall varices
gallbladder wall varices  adenomyomatosis
adenomyomatosis  gallbladder carcinoma
gallbladder carcinoma internal membranous echoes resulting from sloughed mucosa
internal membranous echoes resulting from sloughed mucosa  pericholecystic fluid
pericholecystic fluid discontinuous (±) irregular mucosal enhancement
discontinuous (±) irregular mucosal enhancement  internal membranes (representing sloughed mucosa)
internal membranes (representing sloughed mucosa)  a pericholecystic abscess
a pericholecystic abscess it accounts for 1% of cases of acute cholecystitis, and has a relatively high mortality rate
it accounts for 1% of cases of acute cholecystitis, and has a relatively high mortality rate gallstones are only seen in <50% of patients
gallstones are only seen in <50% of patients a curvilinear brightly echogenic band with acoustic shadowing seen within a non-dependent portion of the gallbladder (representing intraluminal gas)
a curvilinear brightly echogenic band with acoustic shadowing seen within a non-dependent portion of the gallbladder (representing intraluminal gas) this is usually found in critically ill patients
this is usually found in critically ill patients parenteral nutrition
parenteral nutrition  AIDS
AIDS  diabetes
diabetes  chemotherapy
chemotherapy gallbladder wall thickening
gallbladder wall thickening  echogenic contents (± sloughed membranes or mucosa)
echogenic contents (± sloughed membranes or mucosa)  pericholecystic fluid
pericholecystic fluid localized gallbladder tenderness is a good predictive sign but it is difficult to assess
localized gallbladder tenderness is a good predictive sign but it is difficult to assess intramural epithelial crypts (Rokitansky–Aschoff sinuses)
intramural epithelial crypts (Rokitansky–Aschoff sinuses) an ejection fraction < 35% indicates gallbladder dysfunction
an ejection fraction < 35% indicates gallbladder dysfunction it may simulate a malignancy radiologically and pathologically
it may simulate a malignancy radiologically and pathologically the majority have gallstones (± perforation, abscess, or fistula formation)
the majority have gallstones (± perforation, abscess, or fistula formation)