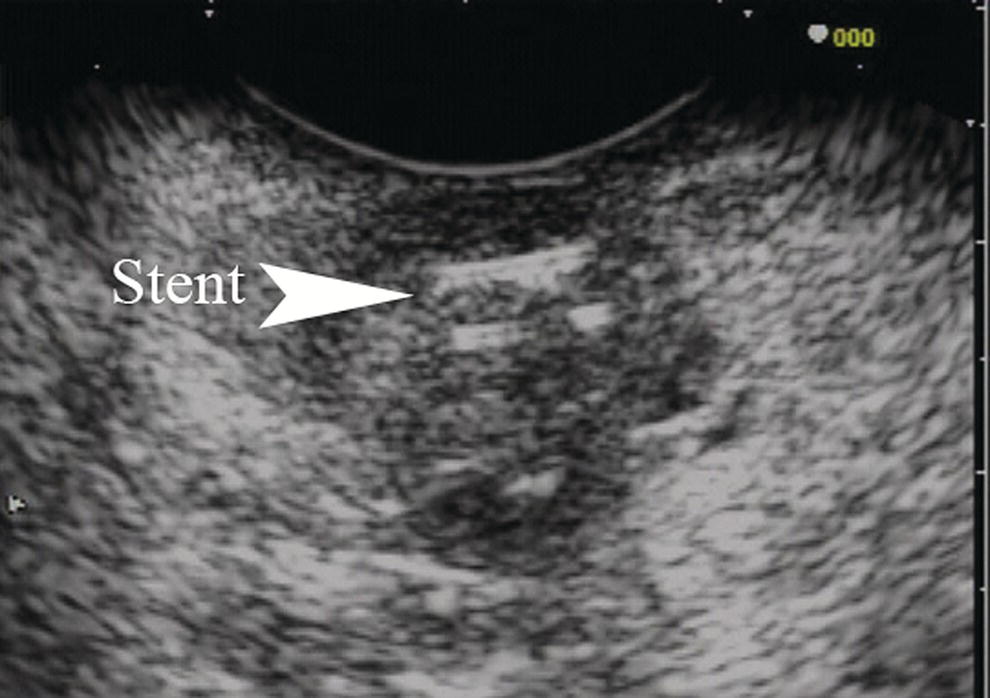
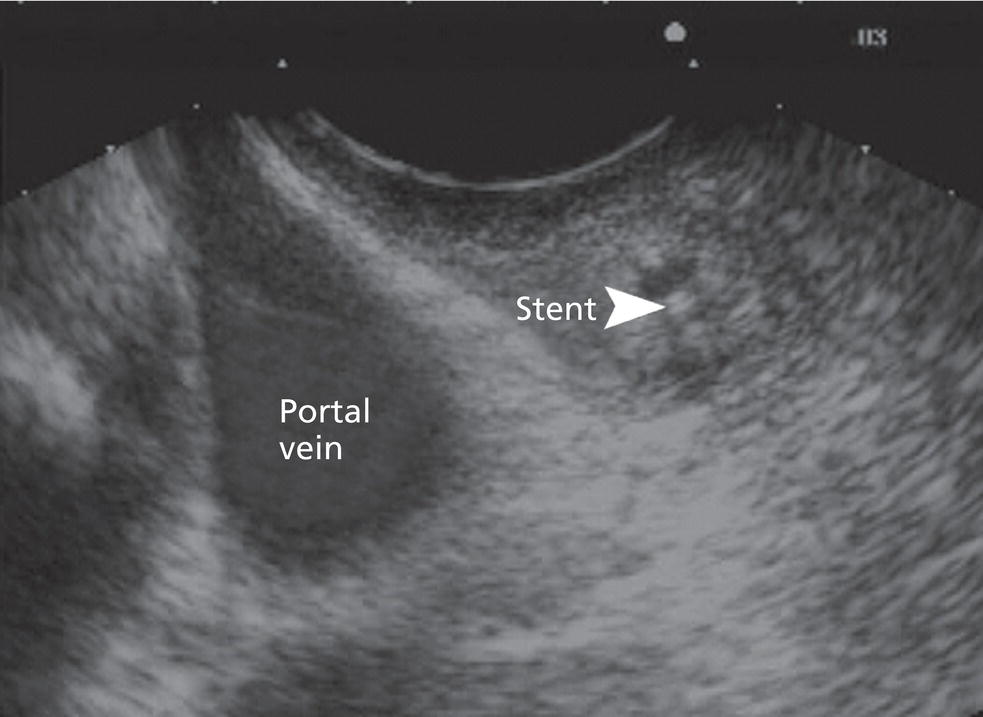
Brenna Casey1 and Kumar Krishnan2 1 Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA 2 Interventional Endoscopy, Harvard Medical School, Massachusetts General Hospital, Boston, MA, USA Cancer arising in the extrahepatic bile duct is curable by surgery in fewer than 10% of all cases. Prognosis depends in part on the tumor’s anatomic location, which determines resectability. Complete resection is possible in 25–30% of lesions that originate in the distal bile duct, whereas the resection rate is much poorer for more proximal sites. Risk factors for bile duct malignancy include a history of primary sclerosing cholangitis, choledochal cysts, or infections with Clonorchis sinensis. Patients may present with jaundice, pain, fever, and pruritus. Endoscopic ultrasonography (EUS) is an invaluable tool for the evaluation of the biliary tract. The close proximity of the echoendoscope transducer to the extrahepatic biliary tree, the lack of radiation, and the low risk of complications makes it an excellent method for examining the common bile duct. The extrahepatic ductal system can be visualized completely by EUS in 96% of patients. The role of EUS in the evaluation of the biliary tract includes biliary obstruction, suspected choledocholithiasis, indeterminate biliary strictures, idiopathic pancreatitis, unexplained right upper quadrant pain, and mass lesions within and adjacent to the biliary tree (Figures 20.1–20.4). Endoscopic ultrasound plays a key role in T‐staging of extrahepatic biliary tumors. TNM staging is as follows. Differentiating between benign and malignant biliary strictures can be challenging as up to 24% of patients with presumed hilar cholangiocarcinoma are found to have benign disease. Cholangiocarcinoma appears as a round hypoechoic lesion which may arise from a focal point on the bile duct wall or surround the duct wall circumferentially. Endoscopic ultrasound imaging alone is not capable of differentiating inflammatory lesions in the bile duct wall from malignancy and therefore tissue sampling is necessary. Fine needle aspiration cytology may be obtained under EUS guidance using linear array endosonography. In the setting of known malignancy, important staging imaging obtained via EUS should include evaluation of the portal venous system for evidence of tumor invasion. Intraductal ultrasound (IDUS) is useful in the detection and evaluation of small biliary tumors. Indicators suggestive of malignancy with IDUS include irregular wall thickening, a hypoechoic mass, a papillary projection, and disruption of the normal three‐layer wall structure of the bile duct. IDUS is ideally suited for imaging of the proximal biliary tree and facilitates imaging of the right hepatic artery, portal vein, and the hepatic duodenal ligament. It has been shown to improve the accuracy of biliary brushings by directing tissue sampling. Limited depth of imaging with IDUS renders it inappropriate for lymph node staging. Endoscopic ultrasound has emerged as a sensitive and specific precursor to endoscopic retrograde cholangiopan creatography (ERCP) for the detection of bile duct stones, and it is more sensitive for the detection of stones of less than 6 mm than magnetic resonance cholangiopancreatography (MRCP). Choledocholithiasis is easily recognized as curvilinear hyperechoic foci with strong acoustic shadowing using either standard or catheter‐based EUS. Low‐amplitude echoes without acoustic shadowing are considered sludge. While ERCP is more accurate for the detection of choledocholithiasis than EUS by a slim margin, it carries significantly higher risk of complications post procedure and is thus no longer desirable as a diagnostic test. Endoscopic ultrasound is a minimally invasive procedure with a procedural risk identical to that of esophagogastroduodenoscopy (EGD). ERCP should be reserved for planned therapeutics. IDUS is useful during ERCP for detecting small stones and sludge that might otherwise go undetected with ERCP alone. Figure 20.1 In this example of a small bile duct malignancy, a focal hypoechoic mass is seen surrounding the bile duct. A biliary stent is present within the mass. Figure 20.2 The linear array echoendoscope is positioned in the second portion of the duodenum. A hypoechoic mass is seen here within the bile duct surrounding a biliary stent. The portal vein is to the left of the mass and the pancreatic parenchyma can be seen beneath and to the right of the mass. Figure 20.3 This 78‐year‐old woman has unresectable pancreatic cancer. Endoscopic ultrasound demonstrates a markedly dilated bile duct containing a large amount of biliary sludge. The patient was treated with biliary stent placement. Figure 20.4 This 46‐year‐old woman presented with elevated liver function tests and right upper quadrant pain. Magnetic resonance cholangiopancreatography (MRCP) revealed a mildly dilated common bile duct with cholelithiasis but no choledocholithiasis. The surgical service has requested clearance of the common bile duct prior to proceeding to cholecystectomy. Endoscopic ultrasound was performed prior to endoscopic retrograde cholangiopancreatography (ERCP) and two common bile duct stones were revealed (a, b). The patient then underwent therapeutic ERCP with successful stone extraction.
20
Biliary Tract Pathology
Primary tumor (T)
TX
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ
T1
Tumor confined to the bile duct histologically
T2
Tumor invades beyond the wall of the bile duct
T3
Tumor invades the liver, gallbladder, pancreas, and/or unilateral branches of the portal vein (right or left) or hepatic artery (right or left)
T4
Tumor invades any of the following: main portal vein or its branches bilaterally, common hepatic artery, or other adjacent structures such as the colon, stomach, duodenum, or abdominal wall
Regional lymph nodes (N)
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Regional lymph node metastasis
Distant metastasis (M)
MX
Distant metastasis cannot be assessed
M0
No distant metastasis
M1
Distant metastasis


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








