1. Screening, diagnosis, and prognosis
(a) To discover candidate biomarkers
(b) To quantify sensitivity and specificity of biomarkers
(c) To monitor outcome of treatment
2. Therapy efficacy
(a) To evaluate biomarkers in clinical trials
(b) To determine the dose effect of a treatment
(c) To identify new therapeutic possibilities
3. Prediction of therapy response
(a) To identify novel targets and/or pathways
(b) To identify agents which predict clinical efficacy
(c) To develop markers which predict response to specific therapy
Biomarkers on tissue specimens (incision or excision biopsies for histology, fine needle aspiration biopsies, and brushings from bile duct strictures) may also be useful for improving the accuracy of diagnosis and prognostication. Identification of these biomarkers requires an understanding of the complex biology of cholangiocarcinoma.
1 Biological Considerations for Understanding of Biomarker Concepts
Cholangiocytes are arranged in a single layer and have important and diverse functions which affect bile flow and prevent the absorption of toxic substances in bile. They are also closely associated with dendritic cells as a protection from bacteria and other antigens. Cholangiocytes are strongly connected by cytokeratins, and they secrete bicarbonate and a number of specialized mucins to provide protection from the bile [12]. One area of importance when searching for new biomarkers is the rich mucin pool derived from cholangiocytes. The established serum biomarkers, carcino-embryonic antigen (CEA), and cancer antigen (CA) 19-9 are glycoproteins that are useful for monitoring the progress of treatment, but their sensitivity and specificity (60–80 %) make them poor diagnostic biomarkers, particularly because they are elevated in chronic inflammatory conditions which lead to the induction of cholangiocarcinoma. As they are also frequently elevated in other malignant conditions of the GI tract, they are poor discriminators between cancers of the GI tract.
Along with the production of mucin, cholangiocytes produce trefoil factor family (TFF) peptides which also protect cholangiocytes and act as receptors, inducing hyperplasia or apoptosis. These proteins have intense cross-linking with sulfur bridges. The synthesis and release of TFFs are regulated by a number of environmental and local agents, estrogens, and pro-inflammatory and anti-inflammatory cytokines [13]. It is worth noting that the majority of cholangiocarcinoma specimens demonstrate an increased production of spliced TFF2 and that when this occurs, it confers a better survival [14].
The significance of MUC mucins in the developing and the adult liver, various hepatobiliary diseases, and intrahepatic cholangiocarcinoma has recently been reviewed [15].
1.1 Importance of Glycoproteins for Cholangiocytes
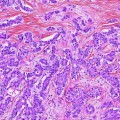
When chronic inflammation induces metaplasia, this may take on an intestinal, gastric, or pancreatic appearance. Inflammatory biliary conditions and tumors of the biliary tree are associated with altered expression of mucins. It is interesting that alteration of mucin production begins as early as the process of metaplasia leading to dysplasia and that this early switch is carried on through the malignant progression of cholangiocarcinomas [16]. Histological assessment of tissues may gain important diagnostic and prognostic information from the immunohistochemical study of the many mucins related to cholangiocarcinoma. When the metaplasia is of gastric cell type, it is likely to be associated with the production of MUC1, while metaplasia of intestinal cell arrangement is associated with MUC2 over-production, implying slightly different malignant potential.
Hughes et al. [17] found that most cases of dysplastic biliary epithelium and cholangiocarcinoma display a Brunner or pyloric gland cell phenotype and a gastric foveolar cell phenotype. However, while aggressive invasive cholangiocarcinoma frequently is associated with MUC1 over-expression, altered MUC1 gene expression also occurs in inflammatory diseases and carcinomas of the GI tract and breast [18, 19], making MUC1 a poor discriminator between tumors.
Cholangiocarcinomas with a better prognosis, particularly those of intraduct papillary type, produce large quantities of gelatinous mucin which is predominantly MUC2. Notably, there is a similar progression from preinvasive lesions in the pancreas with mucin production having a dichotomy in the dysplasia-CIS-invasive carcinoma sequence. In a study of 268 pancreatic tumors, 54 % of the intraductal papillary mucinous neoplasms expressed MUC2, whereas none of the pancreatic intraepithelial neoplasms (PanINs) did. In contrast, PanINs, especially higher-grade lesions, were often positive for MUC1 (61 % of PanIN-3), whereas the expression of this glycoprotein was infrequent in intraductal papillary mucinous neoplasms (20 %). This dichotomy was further accentuated in the invasive carcinoma group [20]. The MUC2 expression in the intrahepatic biliary system, including intestinal metaplasia, intraductal papillary tumors, and mucinous carcinoma, is dependent on the CDX2 homeobox gene, which induces intestinal differentiation [21, 22].
Over-expression of mucins MUC4 and MUC5AC has also been observed in the early phase of the development of hyperplasia and dysplasia in cholangiocarcinoma [15]. MUC4 is a novel intramembrane ligand for receptor tyrosine kinase ErbB2 (HER-2) [23], which has been shown to be associated with a poorer prognosis in patients with mass-forming intrahepatic cholangiocarcinoma [24]. The expression of MUC5AC was associated with the dysplasia–carcinoma sequence.
In summary, tumors which predominantly express the gelatinous mucins MUC2, MUC5AC, MUC5B, and MUC6 are more likely to have a good prognosis, while those associated with the transmembrane mucins MUC1, MUC3, MUC4, MUC12, and MUC17 have a poorer prognosis.
In a study of four cases of oncocytic biliary intraductal papillary neoplasms (IPNs), the IPNs were composed of distinctive oncocytic cells. The invasive carcinomas accompanying two of the cases were also composed of oncocytes. None of the cases showed aberrant expression of the Wnt/β-catenin pathway proteins which frequently have a central role regulating cell fate decisions in neoplasia by integrating signals from many other pathways, including retinoic acid, FGF, TGF-β, and BMP. Despite this, cyclin D1 was markedly over-expressed in all four cases. Three of four cases had positive staining for MUC3, MUC4, MUC5AC, MUC5B, and MUC6. Thus, the Wnt pathway proteins (especially beta-catenin and E-cadherin) are expressed normally in oncocytic variants of IPNs of the biliary tree, and the mucin profile is similar to their counterparts in the pancreas [25].
Diagnosis of cholangiocarcinoma is further complicated by the presence of intrahepatic peribiliary glands, which, particularly when dysplastic, add to the complexity of the microscopic appearance of the biliary tree. These glands are present in the large intrahepatic bile ducts [26–28]. The lobules of branched tubuloalveolar seromucous glands communicate with bile ducts via conduits [29] with serous, mucous, and endocrine cells which stain positively for somatostatin, serotonin, and pancreatic polypeptide [30, 31], which adds to the variety of cell types which may become malignant. These glands have been shown to secrete a seromucin rich in amylase and lipase [32]. As well, the bile duct wall intramural glands have sparsely branching tubular mucus glands with tall columnar cells. These glands could be confused with invasive carcinoma.
At the ampulla of Vater, the distinction between tumors arising from biliary, intestinal, or pancreatic tissue may be helped by a study of the mucus subtypes. Ampullary tumors can be classified histologically as either intestinal type or pancreaticobiliary type and display different features according to tumor location, association with adenoma, and MUC2 expression. Furthermore, KRAS mutation is supposed to be associated with tumors arising in the area from the ampulloduodenum to the ampullopancreatic duct, with metaplastic mucus occurring in both intestinal and pancreaticobiliary types [33].
2 CA19-9 and CEA: Current Markers for Cholangiocarcinoma
CA19-9 and CEA are the established tumor markers with clinical utility in the management of cholangiocarcinoma and gallbladder carcinoma. Numerous studies show that the mean values for these markers are elevated in patients with these carcinomas above those of patients presenting similarly who are found to have benign pathology [34]. However, there are numerous reasons for the limited value of these markers. Firstly, they can be extremely high [35, 36] in some patients with benign conditions, but this may be partly adjusted for by dividing the CA19-9 value by the serum CRP concentration, because the benign cases are frequently associated with inflammation [37]. Even with adjustment, however, the sensitivity, specificity, and positive predictive values remain low at 76.5, 68.6, and 70.9 %, respectively. Secondly, both CA19-9 and CEA are elevated in patients with other forms of gastrointestinal cancer and indeed cancers of the genitourinary system. Lastly, CA19-9 cannot be demonstrated in about 10 % of the population who have Lewis negative blood factors [38]. The use of these tumor markers for diagnosis of cholangiocarcinoma in patients with PSC is unfortunately not as valuable as previously reported [39]. The serum levels of CA19-9 frequently rise temporarily in association with a “biochemical relapse” of PSC (shown by increased values of serum alkaline phosphatase). However, although the marker product of CA19-9 and CEA has a low sensitivity, it has a relatively high specificity for the detection of cholangiocarcinoma in PSC patients [40]. Therefore, assessment of patients with elevated values needs to be made with the knowledge of these variations. These markers are of most value when used in conjunction with other tests, such as radiological findings.
An important drawback of CA19-9 as a tumor marker is that it does not detect early disease. A study of 208 patients with PSC who were followed longitudinally for 5 years with a cutoff of change in CA19-9 concentration of 63.2 U/ml gave 90 % sensitivity and 98 % specificity. However, only two of the 14 patients identified with cholangiocarcinoma were candidates for curative resection. Further, in a study of 866 patients with a presentation of general biliary symptoms, CA19-9 was investigated as a screening test for early pancreatic or biliary cancer. Of 117 subjects with an elevated level above the normal range, 115 did not develop a biliary or pancreatic malignancy after 2-years follow-up and therefore had a false-positive result [41]. Thus, a test with such a low specificity as CA19-9 is quite unacceptable as a screening test.
3 Use of CA15-3 and CA27.29 for Screening, Diagnosis, and Staging
Assays of the markers CA15-3 and CA27.29 are well characterized for the detection of circulating MUC1 antigen in peripheral blood. This circulating marker has prognostic relevance in early-stage breast cancer [42]. The production of MUC1 in breast cancer is very limited compared to that in cholangiocytes, and yet, this topic has been more extensively studied in relation to breast cancer. Given the importance of mucin production by cholangiocytes, it is perhaps surprising that there is a dearth of publications studying the usefulness of such measures for the management of gallbladder carcinoma and cholangiocarcinoma. Two general types of assay measuring MUC1 gene-derived glycoprotein are used: The assays for CA15-3 are sandwich assays, while those for CA27.29 are competitive assays. These types of assay measure slightly different parts of this tandem-repeat molecule. As long as the tests are calibrated carefully, CA15-3 and CA27.29 measurement of MUC1 gives comparable results [43]. While it is likely that serum tumor markers CA15-3 and CA27.29 have prognostic value, their role in the management of early-stage breast cancer is unclear [44], and although they have value in detecting recurrence [45], there is no prospective randomized clinical trial to demonstrate survival benefit and so their role remains uncertain [46]. CA15-3 or CA27.29 can be used in conjunction with diagnostic imaging, history, and physical examination for the monitoring of patients with metastatic disease during active therapy, but they should not be used in isolation.
An interesting cross-sectional study evaluating two GI markers (CA19-9 and CEA) and four breast cancer markers (CA27.29, CA15-3, MCA and CEA) in 213 patients demonstrated sensitivity of 90 %, but specificity was 40.3 % for CEA and 32.3 % for CA19-9 when GI tumors were compared to benign GI disease. This was not as good as the result for breast cancer where a sensitivity of 90 % and specificity of 70 % was obtained for CA27.29, 67.5 % for CA15-3, 52.5 % for MCA, and 40 % for CEA. Comparison of breast cancer and GI malignancies with other malignancies leads to a marked shift of the receiver operating characteristic (ROC) curve to the right and loss of specificity. High serum antigen levels were found in late-stage tumors. Further, the presence of liver metastases in breast cancer was associated with abnormal levels of CA27.29 (P = 0.028). Pancreatic adenocarcinomas had a higher CA19-9 antigen level (P < 0.001) than other GI malignancies. None of the above markers retains its specificity for pancreaticobiliary cancer when compared with a control group consisting of other malignancies [47].
4 Markers of Proliferation
Markers of cellular proliferation can be obtained from tissue samples. For many tumors, such markers can be used as predictors of a poorer prognosis. In general, markers of elevated proliferative rate correlate with a worse prognosis in untreated patients and may predict benefit from chemotherapy [48]. The implementation of DNA flow cytometry to measure proliferative rate is complicated by variation in methods of tissue preparation, differences in instrumentation, and methods for converting information on the histograms to the estimate of the cell cycle S-phase. In addition, interpretation of individual studies is difficult because many are too small to have statistical power, cutoffs have not been prospectively defined, and study populations have not been controlled for adjuvant systemic treatments.
A small number of studies have examined the value of measuring cellular proliferation in managing cholangiocarcinoma. The utility of identifying aneuploidy has been demonstrated in samples taken from paraffin blocks, indicating that this may also be a clinically useful approach in managing cholangiocarcinoma [49]. DNA flow cytometry determination of S-phase is one of the several markers of proliferative rate in tumor specimens, which is applicable to cytology specimens from the biopsy of masses or brush cytology at the time of endoscopic retrograde cholangiopancreatography (ERCP). In pancreatic cancer, aneuploidy has been shown to be predictive of a poorer outcome. Aneuploidy was associated with higher-than-normal levels of other biological markers of prognosis such as HER-2 [50]. Despite these findings, measures of proliferation rate in cholangiocarcinoma are not routinely used in clinical practice.
DNA analysis has been shown to add to the accuracy of CA19-9 and CEA for the diagnosis of cholangiocarcinoma in bile duct strictures. In 57 patients with a diagnosis of PSC undergoing ERCP, brush samples were taken from strictures for cytology and DNA analysis by flow cytometry to obtain measures of proliferation. The tumor markers CA19-9 and CEA were determined both in serum and bile fluid. Thirty-nine patients were found to have malignant strictures (seven with PSC), and a diagnostic sensitivity of 100 % and specificity of 85 % were reached when the results of brush cytology, DNA analysis, serum CA19-9, and serum CEA were combined. Analyses of CA19-9 and CEA in bile fluid yielded no diagnostic significance. The authors concluded that the combination of positive brush cytology at ERCP plus aneuploidy improves the results of serum CA19-9 and CEA. The results were valuable for distinguishing between malignant and benign biliary strictures, especially in PSC patients [51]. A recent review supports the use of fluorescent in situ hybridization (FISH) to identify cells with chromosomal abnormalities to improve sensitivity from that of routine cytology and digital image analysis to identify aneuploidy, but the sensitivity remains low at 40 % [52]. Examination of specific genetic changes in the biliary epithelium may give insights into these important mechanisms and improve our diagnostic ability.
5 P53 as a Marker for Cholangiocarcinoma
Inactivation of the tumor suppressor gene p53, either by mutation or by methylation, is the most common genetic abnormality in human cancer and has been implicated as a late event in the genesis of cholangiocarcinoma [53] and in gallbladder carcinogenesis [54]. Germline abnormalities appear to have a poor association with the onset of cholangiocarcinoma [55]. It is therefore assumed that the onset is caused by the exposure of cholangiocytes to toxic substances excreted in bile. P53 (protein) may be measured in paraffin-fixed tissue by immunohistochemistry (IHC) and p53 genetic changes by gene sequencing. P53 is accumulated in the nucleus in up to 50 % of cholangiocarcinoma cases, reflecting a minor abnormality of the protein and an inhibition of its natural degradation. Notably, about 90 different mutations of p53 have been recognized and there is little difference in the nature of these along the course of the biliary tree. The structure and function of p53 and its role in linking cancer to specific carcinogens by way of mutational signatures have been reviewed [56], and recently, the ratio of two different isoforms, 133p53/Tap53, was shown to be a potential prognostic biomarker. In a study of 36 patients with cholangiocarcinoma [57], clinical outcome was compared for abnormalities of sequencing of p53 gene in the region of exon 5–8 and for P53 protein accumulation to find which measure is the better predictor of outcome. p53 gene mutations were found in 22 of 36 (61.1 %) patients, and for P53 protein, expression was positive in 19 of 36 (52.8 %) patients. There were significant differences in the extent of differentiation and invasion between tumors with positive and negative expression of P53 protein. However, there were no significant differences in pathologic parameters between the mutated and non-mutated tumors. The authors concluded that the identification of alterations of the p53 gene evaluated by DNA sequence analysis is relatively accurate, but despite this, the over-expression of P53 protein could not act as an independent index to estimate the prognosis of cholangiocarcinoma [58]. Fluke-associated cholangiocarcinoma appears more likely to over-express p53 than sporadic cholangiocarcinoma. This may be because of the greater likelihood of an intestinal goblet cell phenotype which over-expresses p53 arising in fluke-associated cholangiocarcinoma as with gallbladder cancer [54]. Differences in the aetiopathology of the cancers may reflect different pathways to the development of cholangiocarcinoma [17].
Several studies of patients with cholangiocarcinoma suggest that high tissue P53 protein levels measured by IHC or mutations or deletions in the p53 gene measured by single-strand conformational gel electrophoresis, manual sequencing, or allele-specific polymerase chain reaction (PCR) appear to predict poor outcome (Table 2). Results in studies showing no effect of P53 accumulation on survival may have been affected by small study numbers. These studies indicate that about 36 % of cases accumulate P53 in the nucleus and that in these cases, there is a poorer survival outcome. However, it seems unlikely that for IHC, P53 will provide sufficient accurate results to be clinically useful, given that it detects both mutated p53 and stabilized wild-type p53, and conversely will miss p53 deletions. This is confirmed by a study where the patients with wild-type P53 exhibited longer overall survival than those with defective P53 [57]. Methods to define genetic abnormalities in p53 more precisely and conveniently might determine specific mutations of p53 which strongly correlate with clinical outcomes and may be a predictor of benefit from systemic therapies. However, at present, methodologies to do so are cumbersome, expensive, and not widely available as routine clinical assays, limiting the utility of this marker in clinical practice. Furthermore, no prospective studies assessing clinical benefits using these new techniques have been published.
Table 2
Studies of P53 in cholangiocarcinoma
Reference | Number of cases | P53 protein expression | |
|---|---|---|---|
Percent (%) | Effect on survival | ||
Ahrendt et al. [95] | 12 | 50 | Reduced survival |
Bergan et al. [96] | 60 ductal type | 25 | Reduced survival: 0.76 vs. 1.4 years |
22 intestinal | 50 | ||
Cong et al. [97] | 22 | 37 | Reduced survival |
Havlik et al. [98] | 29 | Reduced survival | |
Isa et al. [99] | 23 | 21 | No effect |
Jarnagin et al. [65] | 128 | 27 | None, but effect of p27 and Mdm2 seen |
Kim et al. [100] | 25 | 37 | No effect |
Liu et al. [58] | 36 | 51 | Reduced survival |
Kuroda et al. [66] | 55 | 32 | Reduced survival |
Tannapfel et al. [101] | 41 | 32 | Reduced survival |
Washington and Gottfried [102] | 41 | 58 | No effect |
Shin et al. [59] | 36 | 61 | Reduced survival |
Wang [107] | 294 | Meta-analysis reduced survival but not definitive | |
6 Markers of Epigenetic Influences on Gene Function
This is a rapidly progressing field with the advent of gene sequencing and the knowledge of the importance of epigenetic regulators of RNA function for many neoplasms. Recent development of epigenetic evaluation of cancer has demonstrated systematic aberrations where methylation silences specific genes. In particular, cholangiocarcinoma has consistent changes in CDO1, DCLK1, SFRP1, and ZSCAN18 [7]. These genetic abnormalities were seen to occur in cell lines and fresh frozen samples of cholangiocarcinoma and were confirmed in paraffin blocks. When these potential biomarkers were combined as a panel of four, the sensitivity and specificity were 100 % in fresh frozen samples, but the sensitivity fell back to 87 % when tested in validation paraffin samples in this relatively small cohort. The advantage of this technology is that the DNA is stable in bile and so can be measured in bile collected at ERCP or other forms of biliary drainage. Unfortunately, the effect of dilution in bile collections reduces the sensitivity of the method. In many cases, brush cytology is available and this material has been a useful means of obtaining samples for epigenetic studies. Shin and colleagues used a five-marker panel of CCND2, CDH13, GRIN2B, RUNX3, and TWIST1, which improved the sensitivity of cytology from 43 to 83 % [59].
Another study reported OPCML methylation in 72 % of cholangiocarcinoma specimens which was not found in the uninvolved adjacent tissue. Previous studies have demonstrated that OPCML methylation in cholangiocarcinoma is associated with poorer differentiation and as such it should be a marker of poor outcome [60].
7 Urokinase Plasminogen Activator (uPA), Its Receptor uPAR, and Plasminogen Activator Inhibitor 2 (PAI-2) as Markers of Invasiveness in Cholangiocarcinoma
The uPA system has been shown to increase invasiveness, and increased expression of these factors has been associated with poor outcome in some cancers. This system involves a cell surface receptor, uPAR, which becomes active when the uPA protein binds to it. Activation of the uPA/uPAR mechanism may be inhibited by the small proteins PAI-1 and PAI-2. Studies of pancreatico-biliary cancers indicate that poor outcome is predicted by increased expression of uPA and uPAR and further that PAI-2 is an independent predictor of improved outcome by suppression of the uPAR mechanism. Several assay formats for these markers have been evaluated, including IHC, quantitative real-time reverse transcriptase polymerase chain reaction (qRT)-PCR, and enzyme-linked immunosorbent assays (ELISA) [61]. Both qRT-PCR and IHC have been shown to be predictive of survival [62] and to indicate the presence of lymph node metastasis in cholangiocarcinoma [63].
8 Expression of Cathepsin and Cyclin Proteins as Markers of Tumor Progression in Cholangiocarcinoma
Present data are insufficient to recommend use of cathepsin measurements for management of patients with cholangiocarcinoma although studies indicate that different cathepsins are involved in the mechanism of metastasis [64].
Similarly, the cyclin proteins which are expressed in the late G1 phase and promote the transition to the S-phase of the cell cycle are abnormally expressed in some cases of cholangiocarcinoma [25, 65, 66]. They can be measured by IHC in formalin-fixed paraffin-embedded (FFPE) tissue, and mRNA for cyclin E has been quantitated by RT-PCR in fresh frozen specimens [67]. Low molecular weight (LMW) forms of cyclin E have been measured by Western blot analysis of proteins in fresh frozen tissue [68]. Discordance between IHC and Western blot analysis in assessment of the prognostic value of cyclin E may be related to the antibodies used for each assay, given that the reagents that detect intact cyclin E may not react with the LMW fragments. Further work is required to demonstrate the role of these markers in the management of hepatobiliary tumors.
It is considered that the location of a cholangiocarcinoma may be related to the etiology of that tumor which may influence the pathways in the dysplasia–carcinoma sequence. In a study of cell cycle proteins, tissue arrays from tumors at different sites in the biliary tree have been examined by IHC. p27, Cyclin D1, and Bcl2 were more frequently over-expressed in proximal tumors, while p53 and Mdm2 were more frequently over-expressed in distal tumors. While cholangiocarcinomas differentially express cell cycle regulatory proteins based on tumor location and morphology, these differences were not sufficiently distinct to be of diagnostic importance. Vascular invasion, lymph node metastases, absence of p27 expression, and Mdm2 over-expression independently predicted poor outcome on multivariate analysis, and there may be prognostic roles for the proteins Mdm2 and p27. However, these measures did not provide a strong guide for prognosis [65].
9 Proteomic Analysis of Biliary Carcinoma
New technology is revealing a complex array of proteins and peptides in tissue and blood samples and that the pattern of these is distinct for different conditions. Various mixtures of truncated peptide fragments, or of modifications of proteins or peptides, such as glycosylation, cysteinylation, lipidation, and glutathionylation, require careful evaluation to determine their biological role and the value of this new knowledge for improved diagnosis and therapeutic possibilities. It is expected that these differences, either in tissue, in the circulation, or in secreted fluids, will be sufficiently specific to evaluate many different clinical questions. For proteomic pattern analysis, computer-based algorithms have been developed to distinguish bile duct cancer from benign diseases [34]. More work is required on larger numbers of samples from patients to answer specific questions such as identifying the proteins which distinguish patients with PSC from those with cholangiocarcinoma.
Protein expression in tumors reflects the activation of biological pathways, and the degree of activation of these pathways is predictive of patient outcome [69]. Furthermore, tissue may be available for proteomic assessment from samples taken at surgery and through needle biopsy and from FNA or ERCP with cytology. Although cancer mechanisms are best studied in the cancer cells taken with laser dissection, many of the samples acquired include stroma. However, stroma may also hold important messages about cancer biology because the migration of tumor cells relies on an interaction with the stroma and the immune system through dendritic cells. Therefore, many opportunities exist for the discovery of new markers in the holistic cancer biology mechanism. These may be of necessity in low concentrations.
Many technological advances allow the assessment of numerous proteins at very low concentrations, which is useful in analysis of serum. The majority of serum proteins which differentiate patients with cancer from those without are actually not derived from the neoplastic cells, but are host-specific proteins originating in tissues such stroma, liver, or immunological material [70]. New methods that allow isolation of low abundance serum proteins which are more likely to represent tumor markers are in development [71, 72




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree