KEY FACTS
Terminology
- •
Malignant tumor of bladder [95% transitional cell (urothelial) carcinoma]
Imaging
- •
Focal bladder wall thickening with intraluminal extension as mass
- •
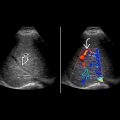
Grayscale US: Immobile polypoidal or broad-based mass along bladder wall, may present as focal wall thickening
- ○
May see associated calcification
- ○
- •
Color Doppler US shows increased vascularity in large tumors; power Doppler more sensitive in detection of vascularity in small tumors
- ○
Useful for bladder tumor screening in patients with schistosomiasis, tumor within diverticulum
- ○
- •
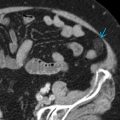
CTU: Better delineation as intraluminal filling defect, screening upper urinary tract
- •
CT sensitivity of 85% and specificity of 94% for detecting bladder tumor
- •
MR: T1WI isointense to muscle/bladder wall, T2WI slightly hyperintense to muscle, early postgadolinium enhancement
- ○
High accuracy for locoregional spread, accuracy of ~ 85% in differentiating nonmuscle invasive from muscle invasive tumor
- ○
- •
± enlarged (> 10 mm) metastatic lymph nodes
Top Differential Diagnoses
- •
Benign prostatic hypertrophy
- •
Bladder debris &/or blood clot
- •
Extrinsic tumor/mass
- •
Bladder inflammation
Pathology
- •
Superficial (70-80%) and are usually papillary (70%)
Clinical Issues
- •
Painless hematuria
- •
If tumor near UVJ, may cause hydronephrosis
Scanning Tips
- •
Check kidneys, ureters for synchronous and metachronous tumors
- •
Optimize color and power Doppler frequency and scale to demonstrate subtle vascularity
- •
Roll patient or ask patient to cough to demonstrate if bladder lesion is attached to wall
- •
Layering debris or blood clot often present and may obscure delineation of tumor